Editors' Choice
Classification of paroxysmal events and the four-dimensional epilepsy classification system
Hans Lüders, Guadalupe Fernandez-Baca Vaca, Naoki Akamatsu, Shahram Amina, Alexis Arzimanoglou, Christoph Baumgartner, Selim R. Benbadis, Andrew Bleasel, Adriana Bermeo-Ovalle, Alireza Bozorgi, Mar Carreño, Michael Devereaux, Stefano Francione, Naiara García Losarcos, Hajo Hamer, Hans Holthausen, Shirin Jamal-Omidi, Giri Kalamangalam, Andrés M. Kanner, Susanne Knake, Nuria Lacuey, Samden Lhatoo, Shih Hui Lim, Luisa V. Londoño, Jayanti Mani, Riki Matsumoto, Jonathan P. Miller, Soheyl Noachtar, André Palmini, Jun Park, Felix Rosenow, Asim Shahid, Stephan Schuele, Bernhard J. Steinhoff, Charles Ákos Szabó, Nitin Tandon, Kiyohito Terada, Walter van Emde Boas, Peter Widdess-Walsh, Philippe Kahane - Epileptic Disord. 10.1684/epd.2019.1033
This educational review describes the classification of paroxysmal events and a four-dimensional epilepsy classification system. Paroxysmal events are classified as epileptic and non-epileptic paroxysmal events. Non-epileptic events are, in turn, classified as psychogenic and organic paroxysmal events. The following four dimensions are used to classify epileptic paroxysmal events: ictal semiology, the epileptogenic zone, etiology, and comorbidities. Efforts are made to keep these four dimensions as independent as possible.
The review also includes 12 educational vignettes and three more detailed case reports classified using the 2017 classification of the ILAE and the four-dimensional epilepsy classification. In addition, a case is described which is classified using the four-dimensional epilepsy classification with different degrees of precision by an emergency department physician, a neurologist, and an epileptologist. [Published with video sequences on www.epilepticdisorders.com]
Aicardi's Diseases of the Nervous System in Childhood; 4th Edition
Ishaq Abu-Arafeh - Epileptic Disord. 2018 Dec 1;20(6):563-564
Jean Aicardi is a name synonymous with modern child neurology. Single-handedly, he wrote the first edition of the book, which bears his name and was published in 1995. The fourth edition, 23 years later, is edited by four eminent child neurologists and written by 47 authors. Recent advancement in areas of neuroimaging, molecular biology, and molecular genetics have unravelled many of the mysteries that challenged paediatric neurologists over the years, leading to a better understanding of many disease [...]
Neurosyphilis: a masked evildoer
Adam Włodarczyk, Joanna Szarmach, Mariusz S. Wiglusz - Epileptic Disord. 2018 Dec 1;20(6):562
To the Editor, We read with interest the paper by Sakai et al. (2018) addressing an case of a 33-year-old male suffering from repetitive tonic-clonic seizures due to neurosyphilic infection. The paper describes the uncommon onset of Treponema pallidum infection with regards to its presentation, complicating the differential diagnosis. However, in our opinion, the differential diagnostic process should also cover the neuropsychiatric presentation of neurosyphilis. Danielsen et al. (2004) found that [...]
A new home for the Genetic Literacy series
Nigel CK. Tan, Samuel F. Berkovic, Daniel H. Lowenstein - Epileptic Disord. 2018 Dec 1;20(6):456
When we first conceived the Genetic Literacy series (Tan et al., 2015), we envisaged the audience as a group of motivated health professionals who were cognizant of their knowledge gaps in epilepsy genetics and who were keen to learn. We wanted to provide this audience with a resource for their learning; hence the start of the Genetic Literacy (GL) series. The ILAE Genetics Commission collectively planned the GL series with clear goals in mind (Tan et al., 2015), deciding on a sequence of papers [...]
A web-based diagnostic reference centre for the European Reference Network “EpiCare”: recommendations of the eNeuropathology working group
Konrad Kölble, J. Helen Cross, Albert Becker, Ingmar Blümcke - Epileptic Disord. 2018 Oct 1;20(5):339-345
Epilepsy surgery is a valuable treatment strategy for a selected group of patients with drug-resistant focal epilepsy. While reliable disease classification is essential for the optimal management of patients in general and crucial for the development of more personalized therapies in the future, arriving at a precise diagnosis often poses considerable difficulties due to the broad and variant-rich spectrum of epilepsy-associated brain lesions. Given the scarcity of European institutions diagnostically focusing on the histopathology of epilepsy surgery cases, the provision of subspecialty expertise as well as training opportunities remains logistically and financially challenging. To improve this situation, the European Reference Network's (ERN) epilepsy care program (EpiCare, http://epi-care.eu) has set out to develop a web-based microscopy referral and teaching framework. This paper reviews the aspects of digital microscopy, data storage, and image analysis technology relevant to the practice of neuropathology. Cognizant of the European data security requirements and regulations, we propose a collaborative, diagnostic network initiative (the eNeuropathology reference centre) and delineate a roadmap for its implementation favouring open-source, vendor-independent browser platforms.
Epilepsy surgery for polymicrogyria: a challenge to be undertaken
Louis Maillard, Georgia Ramantani - Epileptic Disord. 2018 Oct 1;20(5):319-338
Polymicrogyria (PMG) is one of the most common malformations of cortical development (MCDs), with epilepsy affecting most patients. PMG-related drug-resistant epilepsy patients can be considered for epilepsy surgery in well-selected cases. In this context, a comprehensive presurgical evaluation, often including stereo-electroencephalography (SEEG), is warranted to accurately delineate the epileptogenic zone. The heterogeneity of intrinsic epileptogenicity in PMG, together with the additional or predominant involvement of remote cortical areas, calls for a different strategy in PMG compared to other MCDs, namely one that is not predominantly MRI- but rather SEEG-oriented. Favourable results in terms of seizure freedom and antiepileptic drug cessation are feasible in a large proportion of patients with unilateral PMG. PMG extent should not deter from exploring the possibility of epilepsy surgery. On the other hand, patients with hemispheric PMG can be excellent hemispherotomy candidates, particularly when presenting with contralateral hemiparesis. Recent findings support the early consideration of surgery in PMG-related drug-resistant epilepsy.
Genetic literacy series: genetic epilepsy with febrile seizures plus
Kenneth A. Myers, Ingrid E. Scheffer, Samuel F. Berkovic - Epileptic Disord. 2018 Aug 1;20(4):232-238
Genetic epilepsy with febrile seizures plus (GEFS+) is a familial epilepsy syndrome in which affected individuals within a family typically have a variety of epilepsy phenotypes, varying from simple febrile seizures and febrile seizures plus with a good outcome to severe epileptic encephalopathies. Here, we review the spectrum of epilepsy phenotypes, the genetic architecture of GEFS+, and the implicated genes. Using an illustrative clinical case study, we describe important steps in managing patients with GEFS+: making the diagnosis of GEFS+, appropriate genetic testing, and counselling.
Ictal spitting in non-dominant temporal lobe epilepsy: an anatomo-electrophysiological correlation
Marcos Quevedo-Diaz, Adrià Tauste Campo, Manel Vila-Vidal, Alessandro Principe, Miguel Ley, Rodrigo Rocamora - Epileptic Disord. 2018 Apr 1;20(2):139-145
We report a patient presenting drug-resistant, non-dominant temporal lobe epilepsy with ictal spitting and prosopometamorphopsia, both extremely rare semiologies. Second-phase pre-surgical monitoring was performed using SEEG due to lesion-negative imaging and the rare semiology. The seizure onset zone was delimited to the right anterior hippocampus and the temporobasal cortex, with the propagation zone within the entorhinal cortex. Interestingly, direct electrical stimulation to the entorhinal cortex, which was reproduced in a number of trials, evoked spitting without leading to seizures or post-discharges. After the resection of the epileptogenic zone, the patient remained seizure-free without AEDs for a follow-up period of five years (Engel Class 1a). The neuropathology revealed a focal cortical dysplasia type FCD-Ia. Spectral analysis of intracranial ictal EEG (iEEG) data suggested a possible role of the basal temporal and entorhinal cortex as a necessary node in ictal spitting. [Published with video sequences on www.epilepticdisorders.com].
The link between structural connectivity and neurocognition illustrated by focal epilepsy
Elise Roger 1, Laurent Petit 2, Marcela Perrone-Bertolotti 1, Anne-Sophie Job 3, Lorella Minotti 3, Philippe Kahane 3, Monica Baciu 1 * - Epileptic Disord. 2018 Apr 1;20(2):88-98
Increasing attention is being paid to the assessment of white matter properties and its structural connectivity, both in healthy subjects and patients with cerebral lesions. Within this framework, new neurocognitive models based on hodological properties have been developed under a connectomic perspective in order to explain substrates and cognitive mechanisms related to cerebral functions such as language and memory. With regards to focal and drug-resistant epilepsy conceived as a network disorder, new insights in terms of structural connectivity have led to significant advances in epilepsy research, concerning fundamental research (neurocognitive mechanisms of plasticity) and clinical application (optimization of decision making for curative surgery). We believe that such findings in the literature, focused on the role of white matter in cerebral functioning in relation to neurocognition, may be helpful for both researchers and clinicians working in the field of epilepsy.
Keywords: connectivity, white matter, hodology, focal epilepsy, plasticity, cognition
The 2017 ILAE classification of seizure types and the epilepsies: what do people with epilepsy and their caregivers need to know?
Martin J. Brodie, Sameer M. Zuberi, Ingrid E. Scheffer, Robert S. Fisher - Epileptic Disord. 2018 Apr 1;20(2):77-87.
The International League against Epilepsy (ILAE) published in the April 2017 edition of Epilepsia three companion articles on the classification of seizures and the epilepsies. These represent a long-awaited update on the original 1981 and 1989 publications and provide a modern descriptive template. The new classification presents three levels of terminology, involving seizure types, epilepsy types, and syndromes. In this fourth paper, we present an interpretation of these new concepts for people with epilepsy and those who care for them, as well as for young medical doctors not specialized in epilepsy and nurses. Our goal in writing this paper is to ensure that everyone is speaking and understanding the same language, which is fundamental to the optimal management of people with epilepsy.
Facing the hidden wall in mesial extratemporal lobe epilepsy
Theys T, Decramer T, Van Paesschen W, De Tiège X, Minotti L, von Lehe M, Chabardès S, Kahane P, Job AS. - Epileptic Disord. 2018 Feb 1;20(1):1-12.
The risk of unprovoked seizures in population-based cohorts of cerebral infection survivors is 7-8% in developed countries, rising to considerably higher rates in resource-poor countries. The main risk factors for epilepsy after cerebral infection, besides acute seizures, are infection-associated brain lesions and status epilepticus during the acute phase. Despite the high prevalence of pharmacoresistant epilepsies after cerebral infections, especially in patients with MRI-identifiable lesions, only a small minority undergoes epilepsy surgery. However, excellent surgical candidates are particularly those with a history of meningitis or encephalitis in early childhood, hippocampal sclerosis on MRI, as well as a history, seizure semiology, and EEG-findings compatible with the diagnosis of mesial temporal lobe epilepsy syndrome. More challenging are patients with neocortical/extratemporal lobe epilepsies post cerebral infection. Finally, patients with a severe hemispheric injury with contralateral hemiparesis are candidates for hemispherectomy/hemispherotomy. This review attempts to shed some light on this frequent cause of symptomatic focal epilepsy, with an emphasis on the chances offered by epilepsy surgery.
Epilepsy after cerebral infection: review of the literature and the potential for surgery
Georgia Ramantani, Hans Holthausen - Epileptic Disord. 2017 Jun 1;19(2):117-136.
Refractory extratemporal lobe epilepsy (ETLE) tends to have a less favourable surgical outcome in comparison to temporal lobe epilepsy. ETLE poses specific diagnostic and therapeutic challenges, particularly in cases where seizures develop from the midline. This review focuses on the diagnostic challenges and therapeutic strategies in mesial ETLE. The great diversity of interhemispheric functional areas and extensive connectivity to extramesial structures results in very heterogeneous seizure semiology. Specific signs, such as ictal body turning, can suggest a mesial onset. The hidden cortex of the mesial wall furthermore gives rise to specific diagnostic difficulties due to the low localizing value of scalp EEG. Advanced imaging, as well as targeted intracranial studies, can substantially contribute to depict the seizure onset zone since electroclinical findings are difficult to interpret in most cases. Surgical accessibility of the interhemispheric space can be challenging, both for the placement of subdural grids, as well as for resective surgery. When facing the hidden cortex on the mesial wall of the hemispheres, targeted intra- or extra-operative intracranial recordings can lead to satisfactory outcomes in properly selected cases.
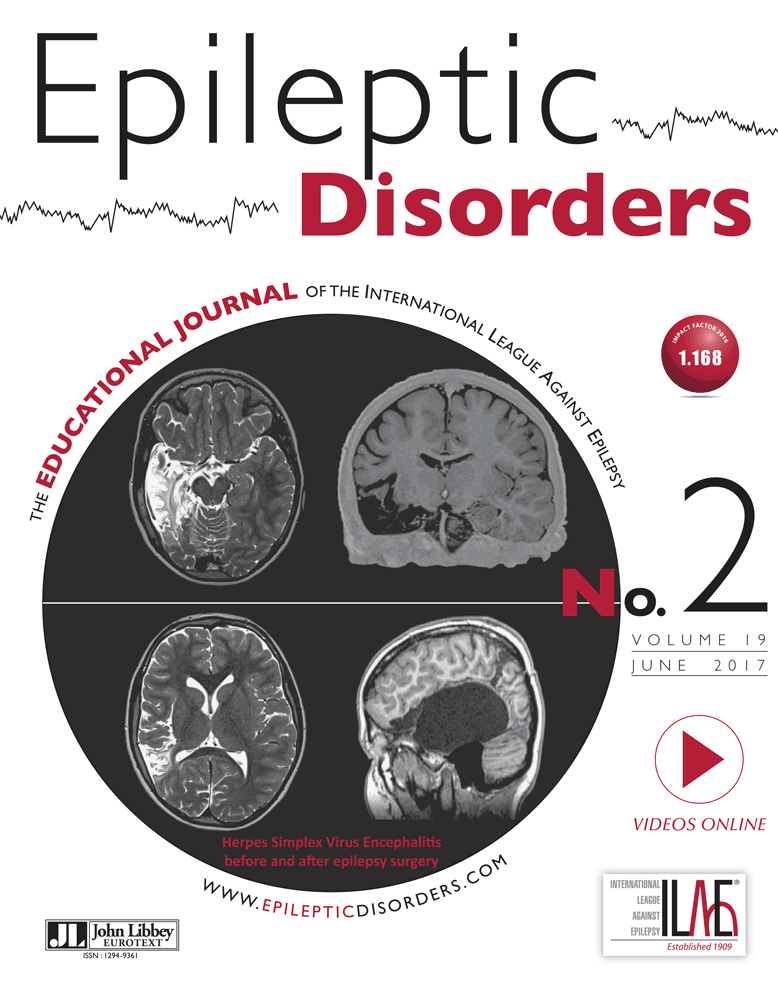
Epilepsy after cerebral infection: review of the literature and the potential for surgery
Georgia Ramantani, Hans Holthausen - Epileptic Disord. 2017 Jun 1;19(2):117-136.
The risk of unprovoked seizures in population-based cohorts of cerebral infection survivors is 7-8% in developed countries, rising to considerably higher rates in resource-poor countries. The main risk factors for epilepsy after cerebral infection, besides acute seizures, are infection-associated brain lesions and status epilepticus during the acute phase. Despite the high prevalence of pharmacoresistant epilepsies after cerebral infections, especially in patients with MRI-identifiable lesions, only a small minority undergoes epilepsy surgery. However, excellent surgical candidates are particularly those with a history of meningitis or encephalitis in early childhood, hippocampal sclerosis on MRI, as well as a history, seizure semiology, and EEG-findings compatible with the diagnosis of mesial temporal lobe epilepsy syndrome. More challenging are patients with neocortical/extratemporal lobe epilepsies post cerebral infection. Finally, patients with a severe hemispheric injury with contralateral hemiparesis are candidates for hemispherectomy/hemispherotomy. This review attempts to shed some light on this frequent cause of symptomatic focal epilepsy, with an emphasis on the chances offered by epilepsy surgery.
Drug-resistant parietal lobe epilepsy: clinical manifestations and surgery outcome
Marjan Asadollahi, Michael R. Sperling, Amin H. Rabiei, Ali A. Asadi-Pooya - Epileptic Disord. 2017 Mar 1;19(1):35-39.
Aim. We reviewed a large surgical cohort to investigate the clinical manifestations, EEG and neuroimaging findings, and postoperative seizure outcome in patients with drug-resistant parietal lobe epilepsy (PLE). Methods. All drug-resistant PLE patients, who were investigated for epilepsy surgery at Jefferson Comprehensive Epilepsy Center between 1986 and 2015, were identified. Demographic data, seizure data, EEG recordings, brain MRI, pathological findings, and postsurgical seizure outcome were reviewed. Results. In total, 18 patients (11 males and seven females) were identified. Sixteen patients (88%) had tonic-clonic seizures, 12 (66%) had complex partial seizures, and 13 (72%) described auras. Among 15 patients who had brain MRI, 14 patients (93%) had parietal lobe lesions. Only three of 15 patients (20%) who had interictal scalp EEG recordings showed parietal interictal spikes. Of 12 patients with available ictal surface EEG recordings, only three patients (25%) had parietal ictal EEG onset. After a mean follow-up duration of 8.6 years, 14 patients (77.7%) showed a favourable postoperative seizure outcome. Conclusion. In patients with PLE, semiology and EEG may be misleading and brain MRI is the most valuable tool to localize the epileptogenic zone. Postsurgical seizure outcome was favourable in our patients with drug-resistant parietal lobe epilepsy.
Epileptic spasms in congenital disorders of glycosylation
Karina A. González-Otárula, Blanca Mercedes Álvarez, François Dubeau
Andreia G. Pereira, Nadia Bahi-Buisson, Christine Barnerias, Nathalie Boddaert, Rima Nabbout, Pascale de Lonlay, Anna Kaminska, Monika Eisermann - Epileptic Disord. 2017 Mar 1;19(1):15-23
Aim. Congenital disorders of glycosylation (CDG) are a group of rare metabolic diseases, characterized by impaired glycosylation of proteins and lipids. Multisystemic involvement is common and neurological impairment is notably severe and disabling, concerning the central and peripheral nervous system. Epilepsy is frequent, but detailed electroclinical description is rare. Methods. We describe, retrospectively, the electroclinical features in five children with CDG syndrome and epileptic spasms. Results. Epileptic spasms were observed in patients with CDG Ik, Ic, Ix, and Ip subtypes, and occurred at an early age, before six months in all cases, except one who had spasms that started at 18 months. In this patient, spasms had an unusual aspect; they did not occur in clusters and were immediately preceded by a myoclonus. All but one child also presented rare myoclonias. On EEG, background activity was poorly organized with abundant posterior spike and fast rhythm activity, but without hypsarrhythmia. At the last evaluation (age range: 6-12 years), two patients still presented epileptic spasms and subcortical myoclonias, one showed rare generalized tonic-clonic seizures, and two were seizure-free. Conclusion. CDG disorders are associated with epileptic spasms with particular features, such as absent hypsarrhythmia, posterior EEG anomalies, and an unusual combination of epileptic spasms with myoclonus. These features, associated with pre-existing developmental delay and subcortical myoclonias, may contribute to the diagnosis of CDG syndrome.
Surgery for epilepsy: a systematic review of current evidence
Siobhan West, Sarah J Nolan, Richard Newton
Epileptic Disorders; 18: 113-21, 2 (June 2016)
This seminar discusses the history and development of techniques for surgical intervention for people with refractory focal epilepsy. Published surgical success rates and prognostic factors associated with post-operative seizure freedom from individual studies have been variable and contradictory. We present here the key findings of a Cochrane systematic review of all evidence published since the introduction of magnetic resonance imaging (MRI) to pre-operative surgical assessment in 1984. Our findings show the usefulness of uncontrolled case series is now past. Future studies with a prospective controlled design should focus on specific research questions to help improve results and provide better-informed advice.
From here to epilepsy: the risk of seizure in patients with Alzheimer’s disease
Nicolas Nicastro, Frédéric Assal, Margitta Seeck
Epileptic Disorders, Volume 18, numéro 1, March 2016, p. 1-12. DOI:10.1684/epd.2016.0808
Aim. To describe the association between Alzheimer's disease and seizures by reviewing epidemiological data from available literature and to assess the putative pathophysiological links between neurodegeneration and altered cortical excitability. We also discuss specific antiepileptic treatment strategies in patients with Alzheimer's disease, as well as transient epileptic amnesia as a possible crossroads between degeneration and epilepsy. Methods. Regarding epidemiology, we searched publications in Pubmed, Medline, Scopus and Web of Science (until September 2015) using the keywords “incidence”, “prevalence” and “frequency,” as well as “Alzheimer's disease” and “seizures”. In addition, therapeutic aspects for seizures in Alzheimer's disease were searched using the key words “antiepileptic drugs,” “seizure treatment,” and “Alzheimer.”
Results. The prevalence and incidence rates of seizures were found to be increased 2 to 6-fold in patients with Alzheimer's disease compared to age-adjusted control patients. Treatment strategies have mainly been extrapolated from elderly patients without dementia, except for one single randomised trial, in which levetiracetam, lamotrigine and phenobarbital efficacy and tolerance were investigated in patients with Alzheimer's disease. Mouse models appear to show a major role of amyloid precursor protein and its cleavage products in the generation of cortical hyperexcitability.
Conclusion. A link between Alzheimer's disease and epilepsy has long been described and recent cohort studies have more clearly delineated risk factors associated with the genesis of seizures, such as early onset and possibly severity of dementia. As genetic forms of Alzheimer's disease and experimental mouse models suggest, beta-amyloid may play a prominent role in the propagation of synchronised abnormal discharges, perhaps more via an excitatory mode than a direct neurodegenerative effect.
Epileptic auras: phenomenology and neurophysiology
A comment from Ghazala Perven and Norman K So
Epileptic Disorders, Vol. 17, No. 4, December 2015, p. 349-62. DOI:10.1684/epd.2015.0786
This review discusses the phenomenology, neurophysiology, and localization of epileptic auras with particular emphasis on how auras can manifest as part of an epileptic network. Epileptic auras, as the first clinical symptom of a seizure, may lead us to infer the site of seizure onset. At the same time, auras can also be a result of activation or alteration in an epileptic network. They can be highly specific or ill-defined in symptomatology. They occur as a result of limited seizure activation, allowing access of the neural signal to the conscious brain. An understanding of epileptic auras offers a window into understanding fundamental brain functions, and helps the clinician at the bedside to make appropriate diagnostic and therapeutic choices.
Epilepsies and Wikipedia
A comment from Mike Kerr, Associate Editor
Information seeking behaviour for epilepsy: an info epidemiological study of searches for Wikipedia articles.
Brigo et al, EpileptiDisord, Vol. 17, No. 4, December 2015, p; 460-6
There are many applications of media and this is increasingly important in epileptology; as excellently highlighted in a recent symposium at the AES in Philadelphia. Doctors should no longer be threatened by patients bearing literature, newspaper clippings or pdfs of papers. However, we should be knowledgeable of the sources of information our patients identify.
This variety of sources may explain misunderstandings between patients and clinicians; this article by Brigo and colleagues provide valuable information in the way our patients locate knowledge from the web.
The authors focus on Wikipedia and they explored English speaking searches, and they provide fairly contemporary information from 2008-2014.
It would seem that people who search the site use broad terms, epilepsy and driving being commonly searched, more than epilepsy in children or epilepsy and employment. Epilepsy searches are less common than those for MS and similar to those for migraine, syncope is relatively less searched.
The article provides useful trend data and comparators. The authors make a strong point that people are searching on the negative impact of epilepsy. This should in my opinion strengthen our resolve to communicate negative impact in our clinical settings. The drive to communicate on SUDEP would be a clear example and it will be interesting to see how it figures in future wiki searches.
A Task Force of the ILAE is currently working in collaboration with Wikipedia to ameliorate information available
Epileptic auras: phenomenology and neurophysiology
Epileptic Disord, Vol. 17, No. 4, December 2015, p; 349-362
This Seminar in Epileptology manuscript by Ghazala Perven and Norman So, also accompanied by a series of educational slides, discusses the phenomenology, neurophysiology, and localization of epileptic auras with particular emphasis on how auras can manifest as part of an epileptic network.
Epileptic auras, as the first clinical symptom of a seizure, may lead us to infer the site of seizure onset. At the same time, auras can also be a result of activation or alteration in an epileptic network. They can be highly specific or ill-defined in symptomatology.
Relative incidence of auras in focal epilepsies is discussed. The authors summarize in a didactic way all major publications on auras from the temporal lobe, the insula, the frontal lobe and the posterior cortex.
Auras occur as a result of limited seizure activation, allowing access of the neural signal to the conscious brain. An understanding of epileptic auras offers a window into understanding fundamental brain functions, and helps the clinician at the bedside to make appropriate diagnostic and therapeutic choices.
Focal ESES as a selective focal brain dysfunction: a challenge for clinicians, an opportunity for cognitive neuroscientists
A comment from Tassinari CA et al
Epileptic encephalopathy with continuous spikes and waves in the occipito-temporal region during slow-wave sleep in two patients with acquired Kanji dysgraphia
Ichiro Kuki, Hisashi Kawawaki, Shin Okazaki, Hiroko Ikeda, Kiyotaka Tomiwa
Epileptic Disorders 2014; 16 (4): 540-5. DOI: 10.1684/epd.2014.0698
We have read with great interest the report by Kuki et al. (Epileptic encephalopathy with continuous spikes and waves in the occipito-temporal region during slow-wave sleep in two patients with acquired Kanji dysgraphia who describe in two young Japanese boys (10 and 11 years old, respectively), the occurrence of an "encephalopathy related to electrical status epilepticus during sleep" (ESES) with a very peculiar clinical picture. In fact, the encephalopathy was very selective indeed since, through the evolution of ESES, both patients retained normal social behaviour and intelligence, and whereas they had no problems reading and writing in the Kana syllabic language, they developed a selective dysgraphia for ideographic Kanji language learnt at school, which, however, could be correctly read and copied. These two written languages are processed through different pathways. The Kanji system is mediated by the posterior inferior temporal cortex (PITC), thalamus, and parietal lobe (Sakurai et al., 2000; Usui et al., 2005). In the patients of Kuki et al., Kanji dysgraphia partially recovered after the disappearance of status epilepticus during sleep (SES). Since functional neuroimaging and MEG dipole clustering of spike activity during ESES suggested a dysfunction in the left posterior inferior temporal lobe, the authors concluded that a very selective impairment, such as the kanji dysgraphia, "may occur due to an electroclinical dysfunction of the left posterior inferior temporal cortex (PITC) in children with ESES".
According to the study of Dehaene and collaborators (Nakamura et al., 2005), the left PITC is activated when a Japanese person is requested to write in Kanji, which requires visualization in space of the complex characters of this language (Tokunaga et al., 1999; Nakamura et al., 2000). Furthermore, since "the left occipito-temporal region is activated by written not pronounced words in every person who can read" (Dehaene, 2007), we can attempt to extend this unique information reported by Kuki et al. to other non-Japanese cognitive acquisitions. Some evidence provided by brain imaging and electrophysiological recording studies in humans has demonstrated that the posterior ventral temporal cortex, including the PITC, is composed of a complex mosaic of functionally discrete columns that respond preferentially to faces, objects, and letters (Puce et al, 1996; Ishai et al., 1999; Dehaene et al., 2002). The dysfunction of a very restricted patch of cortex or even of a limited number of cortical columns could result in such a selective impairment of functions, which could be easily overlooked on clinical grounds. This may well be the case in ESES, particularly at the onset of this condition.
The pathophysiological mechanisms underlying the appearance of cognitive and behavioural disorders in ESES are still poorly elucidated. It has been proposed that epileptic EEG paroxysms may interfere with physiological functions, and possibly, with neuroplasticity processes involved in higher cortical functions (such as learning and memory) that occur during sleep (Tassinari and Rubboli, 2006). Indeed, several studies support a role of sleep in neuroplastic remodelling of neural networks mediating cognitive performances and behaviour, particularly in children. Recent experiments in humans showed that a learning task performed during the day can trigger a local increment of slow wave activity (SWA) during sleep, in correspondence with the cortical regions that were involved in the performance of that task (Huber et al., 2004). This local increase in SWA may imply direct or indirect local plastic changes mediating learning processes and demonstrates a correlation between local SWA homeostasis during sleep and learning/cognitive performances related to the cortical areas where SWA homeostasis was modulated, as postulated by the "synaptic homeostasis hypothesis" (SHY), proposed by Tononi and Cirelli (2006). In the SHY, it is accepted that the synapses are strengthened during wakefulness and weakened or rebalanced during sleep through a process of synaptic downscaling. In other words, strengthening of synapses corresponds to the neuronal process of learning. Occurrence of synaptic downscaling can be indirectly assessed by measuring changes in the slope of EEG slow waves throughout overnight sleep (Vyazovskiy et al., 2009). According to this hypothesis, ESES may represent a model of the clinical effects of the disruption, caused by prolonged focal epileptic activity during sleep, of local SWA homeostatic processes involved in the local plastic changes associated with learning and/or other cognitive functions performed at the site of the epileptic focus (Tassinari and Rubboli, 2006; Tassinari et al., 2012). Indeed, recently, Bölsterli et al. (2011, 2014) observed, in a cohort of children with ESES, no significant change in slow wave slope overnight at the site of the epileptic focus. In addition, spike wave density was correlated with the impairment of the overnight slope decrease. These findings led to the conclusion of a local impairment of the synaptic downscaling process, caused by prolonged focal spike wave activity during sleep, as the potential mechanism underlying the development of neuropsychological deficits in ESES, as previously postulated (Tassinari and Rubboli, 2006). Interestingly, these concepts provide a new approach in the evaluation of the relevance of paroxysmal activities during sleep, not only for ESES, but for a large population of children with significant activation of focal paroxysmal activity during sleep (Cantalupo et al., 2011).
In the children described by Kuki et al. (2014), recovery was achieved in a relatively short time, likely because of the early detection of the selective impairment of Kanji reading, leading to a prompt effective treatment of SES. In this context, EEG and other functional data, as in the cases of Kuki et al., can be particularly helpful in identifying, at an early stage, which functional area(s) might likely be affected by a SES-induced impairment of local SWA homeostasis. In addition, it raises the issue of the need for appropriate neuropsychological testing, individually tailored to specific deficits and interpreted in the light of the neurophysiology and functional neuroimaging data (Filippini et al., 2013). Lastly, these data suggest that, even in individual cases, adequate neurophysiological examination (i.e. electrical and/or magnetic source imaging to localize the "functional lesion"), combined with meticulous neuropsychological evaluation, can be an indirect way to study the cortical network subserving specific cognitive functions.
Carlo Alberto Tassinari, Department of Neuroscience, University of Parma, Parma, Italy
Gaetano Cantalupo, Child Neuropsychiatry, Department of Life and Reproduction Sciences, University of Verona, Verona, Italy
Guido Rubboli, Danish Epilepsy Center, Filadelfia/University of Copenhagen, Dianalund, Denmarkand and IRCCS Institute of Neurological Sciences of Bologna, Bellaria, Hospital, Bologna, Italy
Article | Article PDF | Commentary | Commentary PDF
References
- [Bölsterli et al., 2011] Bölsterli B.K., Schmitt B., Bast T. Impaired slow wave sleep downscaling in encephalopathy with status epilepticus during sleep (ESES). Clin Neurophysiol. 2011;122:1779-1787. 9
- [Bölsterli et al., 2014] Bölsterli Heinzle B.K., Fattinger S., Kurth S. Spike wave location and density disturb sleep slow waves in patients with CSWS (continuous spike waves during sleep). Epilepsia. 2014;55:584-591. 4
- [Cantalupo et al., 2011] Cantalupo G., Rubboli G., Tassinari C.A. Night-time unravelling of the brain web: impaired synaptic downscaling in ESES-the Penelope syndrome. Clin Neurophysiol. 2011;122:1691-1692. 9
- [Dehaene, 2007] Dehaene S. Les neurones de la lecture. Paris: Jacob; 2007.
- [Dehaene et al., 2002] Dehaene S., Le Clec'H.G., Poline J.B., Le Bihan D., Cohen L. The visual word form area: a prelexical representation of visual words in the fusiform gyrus. Neuroreport. 2002;13:321-325. 3
- [Filippini et al., 2013] Filippini M., Arzimanoglou A., Gobbi G. Neuropsychological approaches to epileptic encephalopathies. Epilepsia. 2013;54:38-44. 8
- [Huber et al., 2004] Huber R., Ghilardi M.F., Massimini M., Tononi G. Local sleep and learning. Nature. 2004;430:78-81. 6995
- [Ishai et al., 1999] Ishai A., Ungerleider L.G., Martin A., Schouten J.L., Haxby J.V. Distributed representation of objects in the human ventral visual pathway. PNAS. 1999;96:9379-9384. 16
- [Kuki et al., 2014] Kuki I., Kawawaki H., Okazaki S., Ikeda H., Tomiwa K. Epileptic encephalopathy with continuous spikes and waves in the occipito-temporal region during slow-wave sleep in two patients with acquired Kanji dysgraphia. Epileptic Disord. 2014;16:540-545. 4
- [Nakamura et al., 2000] Nakamura K., Honda M., Okada T. Participation of the left posterior inferior temporal cortex in writing and mental recall of kanji orthography: a functional MRI study. Brain. 2000;123:954-967. 5
- [Nakamura et al., 2005] Nakamura K., Dehaene S., Jobert A., Le Bihan D., Kouider S. Subliminal convergence of Kanji and Kana words: further evidence for functional parcellation of the posterior temporal cortex in visual word perception. J Cogn Neurosci. 2005;17:954-968. 6
- [Puce et al., 1996] Puce A., Allison T., Asgari M., Gore J.C., McCarthy G. Differential sensitivity of human visual cortex to faces, letter strings, and textures: a functional magnetic resonance imaging study. J Neurosci. 1996;16:5205-5215. 16
- [Sakurai et al., 2000] Sakurai Y., Momose T., Iwata M. Different cortical activity in reading of Kanji words, Kana words and Kana nonwords. Brain Res Cogn Brain Res. 2000;9:111-115.
- [Tassinari et al., 2006] Tassinari C.A., Rubboli G. Cognition and paroxysmal EEG activities: from a single spike to electrical status epilepticus during sleep. Epilepsia. 2006;47:40-43. 2
- [Tassinari et al., 2012] Tassinari CA, Cantalupo G, Dalla Bernardina B, et al. Encephalopathy related to status epilepticus during slow sleep (ESES) including Landau-Kleffner syndrome. In: Bureau M, Genton P, Dravet C, et al. Epileptic syndromes in infancy, childhood and adolescence. 5th ed. John Libbey Eurotext, 2012: 255-75.
- [Tokunaga et al., 1999] Tokunaga H., Nishikawa T., Ikejiri Y. Different neural substrates for Kanji and Kana writing: a PET study. Neuroreport. 1999;10:3315-3319. 16
- [Tononi and Cirelli, 2006] Tononi G., Cirelli C. Sleep function and synaptic homeostasis. Sleep Med Rev. 2006;10:49-62.
- [Usui et al., 2005] Usui K., Ikeda A., Takayama M. Processing of Japanese morphogram and syllabogram in the left basal temporal area: electrical cortical stimulation studies. Brain Res Cogn Brain Res. 2005;24:274-283.
- [Vyazovskiy et al., 2009] Vyazovskiy V.V., Olcese U., Lazimy Y.M. Cortical firing and sleep homeostasis. Neuron. 2009;63:865-878.
When patients with epilepsy or “epilepsy” might need a pacemaker
 Ictal asystole mimicking seizure deterioration in temporal lobe epilepsy
Ictal asystole mimicking seizure deterioration in temporal lobe epilepsy
Clinical Commentary with video sequence
Baburhan Guldike, Elisabeth Hartl, Jan Rémi, Soheyl Noachtar
Epileptic Disorders 2015; 17 (3): 332-5
Invited Editorial Comment by John B.P. Stephenson
Cruachan, Bowmore, Isle of Islay, Scotland
Epileptic Disord 2015; 17 (3): 209-10
Ictal asystole means cardiac standstill during an epileptic seizure, as in the woman described by Guldiken et al., (2015) in this issue. If the asystole lasts long enough more than 6 seconds then a syncope results (Bestawros et al., 2015). This is a situation in which a patient with definite epilepsy might need a cardiac pacemaker, but only after careful thought (Benditt et al., 2015).
Much more common is the scenario in which a patient is treated for “epilepsy” but instead has non-epileptic reflex syncope with or without cardiac asystole (Stephenson, 1990; Petkar et al., 2012).
It seems worthwhile to discuss how one should make one or other diagnosis, how one should treat, and especially whether a cardiac pacemaker might be indicated. Read full commentary
Management of epilepsy in resource-limited settings
 Roberto Caraballo, Natalio Fejerman. Neurology Department, Hospital de PediatrÃa JP Garrahan, Buenos Aires, Argentina.
Roberto Caraballo, Natalio Fejerman. Neurology Department, Hospital de PediatrÃa JP Garrahan, Buenos Aires, Argentina.
Epileptic Disorders 2015; 17(1): 13-18.
Commentary by Mike Kerr, Associate Editor
Professor of Learning Disability Psychiatry, Insititute of Psychiatric Medicine & Clinical Neurosciences, Cardiff
The Epilepsy Treatment Gap is huge, as the authors state, 80% of the Global epilepsy population living in resource poor nations; and 90% of these receive no treatment. This seminars series article highlights the challenges including: high incidence, frequent preventable causes, prohibitive cost of treatment and limited availability of trained professionals.
The message for solutions is well made. Information is the key, through high quality epidemiological studies. Though such studies are themselves challenging due to the multiple aetiologies and clinical presentations, especially in countries who have sparse diagnostic resources. Such information can lead to policy focusing on international human rights standards. Rare local neurological professionals need a broad role as educators, advisors and advocates. The next generation of neurologists should be offered training in better resourced epilepsy settings enabling them to cascade their knowledge to less trained local professional.
There are many other good suggestions in this article. In fact I suspect many readers from higher income countries will find the problems resonate with their own experience especially a lack of policy, poor information and continued stigma.
The authors reflect on the importance of the Global Campaign Against Epilepsy. For me their most powerful message is the way a lack of epidemiological evidence means the burden of disease is not communicated, patients are not identified and as a result of this epilepsy does not feature in public health priorities.
Lastly there could not be a more timely publication in the light of the recent fantastic announcement that the resolution, Global burden of epilepsy and the need for coordinated action at the country level to address its health, social and public knowledge implications, was approved on May 26, 2015by the WHO General Assembly and it is now an official WHO document. This great work by ILAE and IBE should be further step to reducing the treatment gap.
Concept of epilepsy surgery and presurgical evaluation
 Rathore C, Radhakrishnan K.
Rathore C, Radhakrishnan K.
Epileptic Disorders 2015; 17(1): 19-31.
Commentary by Silvia Kochen, Associate Editor
Epilepsy Center, Neurology Division, Ramos Mejia Hospital, Buenos Aires, Argentina
The authors, Chaturbhuj Rathore and Kurupath Radhakrishnan from Kerala and Manipal in India, outline the importance of adequate resources for the surgical treatment of epilepsy.
In the first place, they point out the necessity to have human resources with satisfactory knowledge. They divide the population into two groups. The first group concerns patients for whom it is possible to define the epileptogenic zone without invasive investigation, b ut with a clear and precise diagnostic algorithm which is relatively easy to reproduce using continuous video-EEG and MRI. The second group concerns patients for whom invasive recordings are necessary; in this case, the resources, both human and technology-based, are more complex.
The message of the authors is very important because it considers the cost-benefit ratio. In countries with fewer resources, it is possible to offer epilepsy surgery and most candidates for surgical treatment do not require invasive studies.
Editorial Office Note: You can also read in the same issue of Epileptic Disorders another Seminars in Epileptology publication on "Management of epilepsy in resource-limited settings" by Roberto Caraballo and Natalio Fejerman.
Antiepileptic Drugs: Two articles
The clinical pharmacology of traditional antiepileptic drugs.
Vajda FJE, Eadie MJ. Epileptic Disorders 2014; 16: 395-408.
Interactions between antiepileptic drugs, and between antiepileptic drugs and other drugs.
Zaccara G, Perucca E. Epileptic Disorders 2014; 16: 409-432.
Commentary by Graeme J Sills PhD, Associate Editor.
Department of Molecular & Clinical Pharmacology, University of Liverpool, UK
There’s a festival of pharmacology in this issue of Epileptic Disorders! This month we have two Seminars in Epileptology articles, each provided by a duo of very eminent authors who are internationally renowned for their long-standing work in the field of epilepsy therapeutics. Together, these contributions provide an excellent overview of the clinical pharmacology of antiepileptic drugs and their associated pharmacokinetic interactions and are essential reading for those who may be unfamiliar with how some of our most widely-used drugs behave.
In the first article, Vajda & Eadie focus specifically on traditional antiepileptic drugs. They cover a huge volume of information, ranging from mechanisms of action, pharmacokinetics, clinical use and adverse effects, in an impressively succinct fashion. All of the major established agents are included and oxcarbazepine has even snuck in! The text is economical and to the point – if you want detailed discussions and lists of supportive references, you are advised to look elsewhere. If, however, you want facts and lots of them, plus some pithy clinical observations borne of years of experience, then this article is for you (and your trainees).
In the second article, Zaccara & Perucca regale the reader with everything they would ever want to know about pharmacokinetic interactions with antiepileptic drugs. It is important to remember that drugs used in the treatment of epilepsy are amongst the most notorious in terms of their propensity to elicit and/or succumb to drug-drug interactions. Everything from routes of elimination, mechanisms of interactions, and comprehensive lists, tables, and supplementary boxes on interactions with drugs from most major classes is here. The best part, however, is the colourful graphic that successfully illustrates, in one half page, the nature and extent of all pharmacokinetic interactions between existing antiepileptic drugs. This image also adorns the front cover of this issue and is a helpful point of reference for prescribers everywhere.
It is heartening to see pharmacology feature so prominently in this issue of Epileptic Disorders. Starting, stopping and adjusting antiepileptic medication is routine for a sizeable number of medical practitioners - not just epilepsy specialists - and yet the basic therapeutics of these agents is often over-looked or taken for granted. An occasional reminder of what these drugs do and how you can expect them to behave clinically does no harm whatsoever.
Disconnective surgery in posterior quadrantic epilepsy: a series of 12 paediatric patients
Peng-Fan Yang, Zhen Mei, Qiao Lin, Jia-Sheng Pei, Hui-Jian Zhang, Zhong-Hui Zhong, Jun Tian, Yan-Zeng Jia, Zi-Qian Chen, Zhi-Yong Zheng
Epileptic Disorders. 2014 Sep;16(3):296-304
Commentary by Pr. Douglas Nordli Jr, Associate Editor
From my perspective as a pediatric epileptologist involved in single-stage ECoG-guided resections for the past 25 years one of the most challenging aspects of pediatric temporal lobe surgery for intractable epilepsy due to cortical dysplasia is making sure all of the posterior extent of the lesion has been identified so that the surgeon can achieve a complete resection.
This is complicated because the lesion may sometime extend posteriorly and inferiorly a considerable distance beyond the usual margins of a typical temporal lobe resection necessitating a multilobar resection with encroachment into the parietal and occipital lobes. In the past, with the limited surgical exposures for a standard temporal lobectomy and no navigational guidance systems this was very challenging. Nowadays, in centers all around the world we have learned to expect this extent of the lesion and to anticipate the need for more extensive surgery in these cases.
A residual challenge is the best approach for children who have total or near-total involvement of the temporal parietal and occipital lobes with lesions which by themselves, do not need to be resected. Here, multilobar resections will result in a removal of a large amount of substrate and leave large defects, each with their attendant complications. A functional disconnection of these areas may be an elegant alternative approach, particularly if the patient already has a contralateral visual field defect.
P-F Yang and colleagues describe their experience with 12 children who underwent disconnection of the posterior quadrant for intractable epilepsy and highlight the feasibility of this approach. For the most part, these children had concordant clinical neurophysiological, MR and PET pre-operative results implicating the posterior quadrant. None had markedly discordant findings and none had lesions that would require resection for proper management, such as tumors or vascular malformations. Their surgical approach allowed for small incisions with minimal blood loss. Once they mastered the technique of sparing bridging vessels there were no significant unanticipated complications. All children had expected contralateral field defects, as expected. The outcomes at an average of 34 months were favorable with 75% of patients being seizure-free. Comparison of pre- and post-operative neuropsychological testing showed significant improvement (Global IQ mean of 58 versus 47, p < 0.04).;
This very useful contribution to the surgical literature supports the use of a disconnection strategy for patients with extensive involvement of the posterior quadrant with lesions that by themselves do not require resection.
Persistent frequent subclinical seizures and memory impairment after clinical remission in smoldering limbic encephalitis
Kyoko Kanazawa, Riki Matsumoto, Akihiro Shimotake, Masako Kinoshita, Akiko Otsuka, Osamu Watanabe, Keiko Tanaka, Ryosuke Takahashi, Akio Ikeda.
Epileptic Disorders. 2014 Sep;16(3):312-7
Commentary by Pr. Yushi Inoue, Associate Editor
Not only the seizures but also impairment of cognition such as memory are important sequelae of limbic encephalitis in both acute and chronic phases. This manuscript described two patients with immune-mediated limbic encephalitis who had clinical seizures and memory impairment. Although clinical seizures remitted, memory impairment persisted over one to two years. The authors then gave the patients immunotherapy, which resulted in memory improvement. The clue was the EEG. The authors suggest a residual active chronic process of inflammation years after acute phase in a "smoldering" limbic encephalitis, and the importance of Video-EEG recording in diagnosing and treating such cases.
This contribution offers an important clinical message, as it seems that patients with limbic encephalitis need long term follow-up and assessment; the insult from the encephalitis may be not solely due to initial damage but also a lingering auto immune pathology that may need reinvestigation and treatment.
Time to relapse after epilepsy surgery in children: AED withdrawal policies are a contributing factor.
Boshuisen et al.
Epileptic Disorders. 2014 Sep;16(3):305-11
Commentary by Pr. Michael Duchowny, Associate Editor
Director, Neurology Training and the Comprehensive Epilepsy Center
Miami Children's Hospital, Professor of Neurology and Pediatrics, University of Miami Miller School of Medicine
Florida, USA
Can the time course of seizure recurrence after epilepsy surgery in childhood be explained by operative or post-operative factors? This question has practical relevance as many children with intractable focal epilepsy who fail to become seizure-free after an excisional procedure return for further surgical consideration. Early postoperative seizure recurrence (generally regarded as occurring within the first six months) is traditionally believed to indicate a failure to fully excise the entire epileptogenic zone and structural lesion if found on MR imaging. Re-emergence of a postoperative seizure semiology that resembles the pre-operative pattern is believed to further implicate residual epileptic tissue in seizure persistence rather than a new independent seizure focus.
Until now there has been little interest in the specific role of post-operative AED withdrawal in promoting seizure recurrence. Indeed, studies of post-operative medical treatment have mainly focused on how long to continue treatment rather than examining any cause and effect relationship on seizure recurrence. Boshuisen and colleagues (1) set out to examine this issue in the Paediatric Epilepsy Surgery cohort of 95 patients from the “Time to Stop” study (2). Using multivariate analyses, they found that a shorter interval to AED reduction was the only independent predictor of a shorter time to relapse, revealing more rapidly whether surgery had the intended curative effect, independently of the other factors involved. It was also noted that univariate analysis identified incompleteness of resection of the epileptogenic zone was also associated with a shorter time to recurrence.
These observations extend the traditional view of surgical failure and in doing so raise many interesting questions. Does medication withdrawal “promote epileptogenesis after surgery and if so, how does this situation differ from the contribution of AED withdrawal in medical epilepsy patients? Should postoperative AED treatment be prolonged for a longer period of time, and are these findings unique to the pediatric patient? Further studies are clearly in order to address the questions raised by this important and provocative study.
Importantly, surgery was finally offered in more than 3/4 of the most complicated cases (25/32), with results that remained very good (64% of Engel class I). Even patients whose pathology finally proved normal or inconclusive - a finding, which remains challenging in the field of epilepsy surgery - could do well after surgery, although the rate of seizure freedom proved much less satisfactory (36% of Engel class I).
Overall, the merit of this study is to exist, and to serve as a reference in the field of invasive evaluation in children older than 2 years of age. The advent of 3D multimodality imaging methods should help in the future to better target the regions suspected to be epileptogenic, in order to avoid a second SEEG investigation (which represented almost 10% of the cases) and improve surgical results (17% of the children were classified as Engel class IV after surgery).
References:
1) Boshuisen K, Schmidt D, Uiterwaal CS, Arzimanoglou A, Braun KP, TimeToStop Study Group. Time to relapse after epilepsy surgery in children: AED withdrawal policies are a contributing factor. Epileptic Disord. 2014 Sep;16(3):305-11.
(2) Boshuisen K, Arzimanoglou A, Cross JH, Uiterwaal CS, Polster T, van Nieuwenhuizen O, Braun KP; TimeToStop study group. Timing of antiepileptic drug withdrawal and long-term seizure outcome after paediatric epilepsy surgery (TimeToStop): a retrospective observational study. Lancet Neurol. 2012
Sep;11(9):784-91.
Stereo-electroencephalography (SEEG) in 65 children: an effective and safe diagnostic method for pre-surgical diagnosis, independent of age
Taussig D, Chipaux M, Lebas A, Fohlen M, Bulteau C, Ternier J, Ferrand-Sorbets S, Delalande O, Dorfmüller G.
Epileptic Disorders. 2014 Sep;16(3):280-95
Commentary by Pr. Philippe Kahane, Associate Editor
Director Epilepsy Unit, Neurology & Psychiatry Department Grenoble University Hospital, France
More than half a century after its development at Sainte Anne Hospital in Paris (1), the SEEG methodology, both in adults and children, has gained an increasing interest worldwide. For many years, the method has remained challenging in the young paediatric population, both for technical reasons (thickness and rigidity of the skull, tolerance to long-term monitoring) and for age-related semiological and neurophysiological peculiarities, which make localizing hypotheses more complex and difficult to elaborate than in adults.
Only a few studies have dealt specifically with SEEG in children (2, 3), thus making the present publication from the Rothschild Foundation team in Paris particularly interesting. Delphine Taussig and colleagues report their experience on the largest published series of SEEG in children (n=65), putting emphasis on the safety of the procedure (no morbidity, even in children as young as 20 months) and efficiency (78% of the patients eventually received surgery).
Interestingly, a large majority of the surgical procedures were monolobar, even in young children, which contrasts with the common idea that large resections are often mandatory at this age group. Such results confirm and underscore the fact that the main aim of SEEG investigations is to tailor the resections. Overall, 67% of the children became seizure-free (Engel class I), with results that appear better in young patients (n=21; age at SEEG < 5 years; seizure-free: 79%) as compared with the older children (n=44; age at SEEG > 5 years; seizure-free: 59%).
Importantly, surgery was finally offered in more than 3/4 of the most complicated cases (25/32), with results that remained very good (64% of Engel class I). Even patients whose pathology finally proved normal or inconclusive - a finding, which remains challenging in the field of epilepsy surgery - could do well after surgery, although the rate of seizure freedom proved much less satisfactory (36% of Engel class I).
Overall, the merit of this study is to exist, and to serve as a reference in the field of invasive evaluation in children older than 2 years of age. The advent of 3D multimodality imaging methods should help in the future to better target the regions suspected to be epileptogenic, in order to avoid a second SEEG investigation (which represented almost 10% of the cases) and improve surgical results (17% of the children were classified as Engel class IV after surgery).
References:
- Bancaud. Apport de l’exploration fonctionnelle par voie stéréotaxique à la chirurgie de l’épilepsie. Neurochirurgie 1959;5:5–112.
- Cossu et al. Stereo-EEG in children. Childs Nerv Syst 2006;22:766-778.
- Cossu et al. Stereoelectroencephalography in the presurgical evaluation of focal epilepsy in infancy and early childhood. J Neurosurg Pediatr 2012;9:290-300.
Can ACTH therapy improve the long-term outcome of drug-resistant frontal lobe epilepsy?
Giuseppe Gobbi, Giulia Loiacono, Antonella Boni, Lucia Marangio, Alberto Verrotti
Epileptic Disorders. Volume 16, Number 2, 185-190, June 2014
Commentary by Aristea S. Galanopoulou MD PhD, Epileptic Disorders Associate Editor
Professor, Saul R. Korey Department of Neurology
Associate Professor, Dominick P. Purpura Department of Neuroscience
Albert Einstein College of Medicine, Bronx NY, USA
Adrenocorticotropic hormone (ACTH) has been extensively used in the treatment of West syndrome (WS) but also for other early life epileptic encephalopathies, such as Landau Kleffner syndrome (LKS), and continuous spike wave in slow wave sleep syndrome (CSWS). These are epileptic syndromes that manifest in infancy or early childhood, do not necessarily have the same types of epileptic seizures, but have prominent interictal epileptic abnormalities with neurodevelopmental sequelae. Gobbi et al (Epileptic Disorders, June issue) report here beneficial effects of ACTH treatment in 5/6 young patients with drug-resistant frontal lobe epilepsy. Unlike patients with the classical ACTH-responsive epileptic encephalopathies (WS, LKS, CSWS), this small cohort included teenagers as well as children (range 4 to 17 years old). Their seizures were atypical absences, tonic or tonic versive or drop attacks, and all had secondary bilateral synchrony with focal abnormalities on their EEGs. Seizures stopped within 6 weeks in 83% of them. Among the responders, 60% maintained seizure freedom at 6 months of follow up while eventually all initial responders achieved seizure freedom at 12 months of follow up. No serious adverse effects were reported in this cohort.
The findings of Gobbi et al (Gobbi et al. 2014) indicate that ACTH may not be strictly the medical treatment for WS or LKS and CSWS but could potentially be considered in other drug resistant epileptic syndromes, as in frontal lobe epilepsy. Precedents do exist to support this concept. Snead et al (Snead et al. 1983) reported that 12/18 (66.7%) of children with drug-resistant epilepsies without infantile spasms responded to high dose ACTH, although the relapse rate was 40%. Okumura et al (Okumura et al. 2006) reported seizure freedom in 13/15 patients (86.7%) with generalized seizures (atypical absences, tonic, drop attacks or myoclonic but not infantile spasms) although again 46% relapsed. Kalra et al (Kalra et al. 2009) also reported therapeutic effects of ACTH in two patients (3 and 7 year old) with drug resistant epilepsies. In a Cochrane type review performed by Gayatri et al (Gayatri et al. 2007) only one double blind randomized prospective study was found that intended to evaluate the efficacy of steroids or ACTH4-9 analogue in children with intractable epilepsy without infantile spasms (Pentella et al. 1982). The study showed mild to moderate reduction in seizures in 3 / 4 children.
The existing small cohort studies are certainly valuable and maintain our interest in further exploring the possibilities of ACTH therapy in the pediatric epilepsy population, raising important questions. Which epilepsy syndromes might benefit from ACTH beyond WS / LKS / CSWS? Is ACTH beneficial only for very young patients or also for older age groups as the Gobbi study suggests? What are the long-term outcomes of ACTH treatment? The need for randomized, blinded, controlled, well powered studies to address these questions is evident, although such studies are not easy to be done.
References:
- Gayatri NA, Ferrie CD, & Cross H. Corticosteroids including ACTH for childhood epilepsy other than epileptic spasms. Cochrane Database Syst Rev 2007: CD005222.
- Gobbi G, Loiacono G, Boni A, Marangio L, & Verrotti A. Can ACTH therapy improve the long-term outcome of drug-resistant frontal lobe epilepsy? Epileptic Disord 2014; 16: 185-190.
- Kalra V, Sharma S, & Arya R. ACTH therapy in refractory generalized epilepsy. Indian J Pediatr 2009; 76: 91-93.
- Okumura A, Tsuji T, Kato T, Natsume J, Negoro T, & Watanabe K. ACTH therapy for generalized seizures other than spasms. Seizure 2006; 15: 469-475.
- Pentella K, Bachman DS, & Sandman CA. Trial of an ACTH4-9 Analogue (ORG 2766) in children with intractable seizures. Neuropediatrics 1982; 13: 59-62.
- Snead OC, 3rd, Benton JW, & Myers GJ. ACTH and prednisone in childhood seizure disorders. Neurology 1983; 33: 966-970.
Early add-on treatment vs alternative monotherapy in patients with partial epilepsy
Franck Semah, Pierre Thomas, Safia Coulbaut, Philippe Derambure
Epileptic Disorders. Volume 16, Number 2, 165-174, June 2014
Commentary by Graeme J Sills PhD, Epileptic Disorders Associate Editor
Department of Molecular & Clinical Pharmacology, University of Liverpool, UK
There are many significant questions in epilepsy therapeutics that remain to be answered, not least of which is what to do after the first drug fails. Much has been written on this issue but relatively few investigators have been brave enough to tackle it in a prospective manner. In this issue, Semah and colleagues report the outcome of a 10-year odyssey to shed light on whether it is better to switch or to add after the first medication has proved ineffective. In doing so, they also highlight the many challenges associated with these types of investigations.
In some ways, the results are the least interesting aspect of this article. In patients with recently diagnosed focal epilepsy who have failed their first choice antiepileptic drug due to incomplete seizure control at an adequate dose, there is no apparent difference between switching to another appropriate monotherapy and adding-in a second drug, in terms of either efficacy or tolerability. This is perhaps unsurprising given the size of the study population, their expected pharmacological responsiveness, and what we know from previous work.
Instead, it is the extreme heterogeneity, in both patient characteristics and drug choice, that sparks the greatest interest in this report and which serves as a reminder of the difficulty in delivering a study that is reflective of real-world clinical practice but also scientifically and statistically robust. This article is far from definitive in terms of treatment policy after initial drug failure in epilepsy but the authors should be applauded for their initial ambition, their continuing perseverance and their eventual honesty. There is a salutary lesson here for anyone who dreams of tackling the big issues in the pharmacological management of epilepsy.
Paediatric epilepsy surgery in the posterior cortex: a study of 62 cases
Alexandra Liava, Roberto Mai, Laura Tassi, Massimo Cossu, Ivana Sartori, Lino Nobili, Giorgio Lo Russo, Stefano Francione
Epileptic Disorders 2014; 16(2): 141-64.
Commentary by Pr. Michael Duchowny, Associate Editor
Director, Neurology Training and the Comprehensive Epilepsy Center
Miami Children's Hospital
Professor of Neurology and Pediatrics, University of Miami Miller School of Medicine
Clinical Professor, Department of Neurology Florida International University College of Medicine
Miami, Florida, USA
Intractable focal epilepsy that begins in early postnatal life is associated with long-term neuro-cognitive dysfunction. Recognition of this poor prognosis is a decisive factor in the early surgical referral with a goal of definitive cure. However, candidates for surgical therapy in the first decade of life have many different etiologies and multiple regions of involvement that are approached utilizing different anatomic procedures. Despite these challenges, temporal and extra-temporal pediatric epilepsy surgery data in very early life is now widely available and serves as a helpful guide; the experience with MRI-negative patients has also been described (Duchowny et al, 1998; Jayakar et al, 2009). Missing from this picture, however, are large cohort studies focused more specifically on childhood surgery for focal seizures originating in the posterior hemispheric regions.
The recently published cohort study of 62 children with focal epilepsy arising in the posterior cerebral hemispheres (Liava et al, 2014) is therefore a welcome step towards filling this gap. Although the outcome of posterior hemisphere pediatric epilepsy surgery has been reported previously (Fogarisi et al, 2003), additional carefully collected data is extremely valuable. Liava and colleagues (2014) describe their experience with 62 cases undergoing excisional procedures and functional disconnections who had thorough pre-operative investigations. The cohort was primarily MRI-positive- only 3 cases had unremarkable MRI studies, and 24 patients (39%) underwent stereo-EEG recordings. Not surprisingly, the cohort was heterogeneous with regard to etiology, surgical procedure and region(s) of involvement. The occurrence of varying degrees of pre-existing cognitive disturbance in a high proportion of cases is fully consistent with both pediatric surgical series and childhood epilepsy in general. The 29% incidence of hemianopic visual field defect is also not surprising in this selected cohort.
The investigators achieved a very high rate of seizure freedom with 86% achieving Engel Class 1 outcomes. This result is even more remarkable given the authors acknowledgement that complete resection “did not necessarily imply the complete resection of the MRI-detectable lesion”. That this cohort could attain such a high rate of seizure-freedom is welcome news for pediatric epilepsy surgery teams.
Although posterior hemispheric cases constitute a minority pediatric epilepsy surgery caseloads, they are by no means rare. Cortical malformations can occur anywhere within the cerebral cortex and osterior cortical involvement is common. The Milano cohort included a high proportion of multi-lobar cases, many of whom had ill-defined resection margins and involvement of eloquent (visual, somatosensory) cortex. Addressing both issues is a primary pediatric epilepsy surgery challenge and often contributes to compromised surgical success. As there is greater experience in adult epilepsy surgical populations with posterior resections and their challenges, the results of the Milano group offer important reassurance that similar approaches can also be used successfully in very young patients.
An important distinguishing feature of the Liava et al (2014) study is their attention to their patients’ seizure semiology. As the authors correctly note in their introduction, seizures that arise in the posterior cortex may propagate widely via multiple fascicular pathways resulting in clinical features more typical of secondary sites. This issue is especially problematic for seizures that arise in the parietal lobe as electrographic seizure onset is often clinically silent and thus associated with a falsely localizing “pseudo-focus” (Jayakar et al, 1991). With this understanding, the authors were able to identify a specific complex of symptoms and signs that were strongly suggestive of primary occipital lobe seizure origin. These included the presence of a pre-existing visual field defect and lateralized complex visual hallucinations in conjunction with oculogyric or oculo-clonic movement at ictal onset. Equally important, the investigators noted that ictal blindness and eye deviation were much less specific. Fear was a frequent subjective ictal complaint that disappeared in six of 7 patients undergoing parietal resection. However, although the perception of fear is described in patients with parietal lobe seizures, caution should be exercised as ictal fear can occur in patients with seizures arising in the frontal and temporal lobes (Toth et al, 2010; Akiyama et al, 2014).
All three MRI-negative patients had poor outcomes. While the presence of a discrete lesion on imaging is a useful marker of the epileptogenic zone, favorable postoperative outcomes are still possible without it (Jayakar et al, 2009). Functional imaging was not employed in the pre-operative evaluations of the Liava et al (2014) cohort and one is left wondering whether including this information might have made a difference. As electrophysiological information was insufficient for surgical planning in approximately one-third of cases and the scalp interictal EEG was judged to be misleading in approximately one-fifth of cases, it is understandable that accurate localization would be extremely difficult. However, for MRI-positive patients, complete removal of the anatomic lesion was not required for seizure-freedom, and the MRI-negative group, though small, likely failed for different reasons. It is known that resection of either the anatomic lesion or the epileptogenic zone can result in good outcome even if the other is not fully excised (Perry et al, 2010). The epilepsy in the MRI-negative patients was probably secondary to Type 1 focal cortical dysplasia and surgical failure was likely due to incomplete resection of a dysfunctionally activated cortical network. Whether the ability to define dysfunctional epileptic networks in the posterior cerebral hemisphere is comparable to anterior networks remains unknown. It is even less certain whether anatomically diverse networks are functionally similar.
The Liava et al (2014) study findings should be viewed as an important step in our progress towards understanding the surgical implications of lesion-driven posterior hemispheric seizure surgery. Lesionectomy, lobectomy, multi-lobar resection and disconnection, the surgical procedures employed in this report, are all preferable to more radical procedures such as hemispherectomy- the ability to achieve function-sparing seizure-freedom is obvious. The rate of seizure-freedom in this series is certainly comparable to the outcomes reported for frontal lobe cases. The justification for this “less is more” approach will become more secure if longitudinal studies can assess the long-term cognitive, behavioral and social outcomes of early posterior hemisphere surgery, particularly after tailored resection and lesionectomy. Pre-operative and post-operative neuropsychological data was collected by the investigators in this study and will hopefully be reported in a future publication.
References:
- Akiyama M, Kobayashi K, Tukushi I et al. Five pediatric cases of ictal fear with variable outcomes. Brain Dev (2014), http://dx.doi.org/10.1016/j.braindev.2013.11.011
- Duchowny M, Jayakar P, Resnick T et al. Epilepsy surgery in the first three years of life. Epilepsia 1998; 39:737-743.
Fogarasi A, Boesebeck F, Tuxhorn I. A detailed analysis of symptomatic posterior cortex seizure semeiology in children younger than seven years. Epilepsia 2003; 44:89-96. - Jayakar P, Duchowny M, Alvarez L et al. Pitfalls and caveats in localizing seizure foci. J Clin Neurophysiol 1991; 8(4): 414-431.
- Jayakar P, Dunoyer C, Dean P et al. Epilepsy surgery in children with normal or non-focal MRI scans: integrative strategies offer longterm seizure relief. Epilepsia 2008; 49:758–764
- Liava A, Mai R, Tassi L et al. Paediatric epilepsy surgery in the posterior cortex: a study of 62 cases. Epileptic Disord 2014; 16(2): 141-64.
- Perry S, Dunoyer C, Dean P et al. Predictors of seizure freedom after incomplete resection in children. Neurology 2010;75:1448–1453
- Toth V, Fogarasi A, Karadi K et al. Ictal affective symptoms in temporal lobe epilepsy are related to gender and age. Epilepsia. 2010 ;51(7):1126-32.
Cortical network dysfunction in musicogenic epilepsy reflecting the role of snowballing emotional processes in seizure generation: an fMRI-EEG study.
Volker Diekmann & Anselm C. Hoppner
Epileptic Disorders. Volume 16, Number 1, 31-44, March 2014
Comments by Associate Editor Sara Wilson
Within the field of epilepsy research, musicogenic epilepsy has received scant attention, with little known about its underlying mechanisms despite being described over 75 years ago. By contrast, the field of music neuroscience is burgeoning with studies investigating the music networks of the brain, including the potent ability of music to activate reward and emotion processing systems. Musicogenic seizures provide an obvious opportunity to investigate these networks and their dysfunction in people with epilepsy. In the current study this was done in a patient using the gold-standard technique of EEG-fMRI.
An intriguing aspect of musicogenic epilepsy is triggering by highly selective music stimuli, which in this case was a specific type of Russian music as opposed to similar music of different origin. In addition to pink noise, the latter provided an ideal control stimulus, allowing the specificity of network dysfunction to be explored. This revealed activation of the affective network, particularly regions involved in positive emotional processing, at the onset of the Russian music. A clear strength of the study was subsequent exploration of the way this activation changed over time, prior to the emergence of a seizure. This analysis identified maladaptive interactions between components of the cognitive control, autobiographic memory and affective networks, with reduced cognitive down regulation thought to allow ‘snowballing’ activity in emotion-related areas, ultimately triggering the seizure.
By drawing on the broader cognitive neuroscience literature investigating network function in healthy individuals combined with careful examination of this instructive case, this study presents a compelling argument that musicogenic epilepsy may not just arise from musicological features of the stimulus per se. Moreover, the researchers propose that similar mechanisms of cognitive dysregulation of emotion processing networks may apply in other cases of reflexive epilepsy, such as reading epilepsy. This interesting hypothesis provides an exciting direction for future research into this poorly understood form of epilepsy.
Generalised electrographic seizures presenting as perioral myoclonia
Jennifer Deraborn and Peter Kaplan
Epileptic Disorders. Volume 16, Number 1, 13-18, March 2014
Comments by Associate Editor Yushi Inoue MD PhD
A 41-year-old man had several episodes of rhythmic and intermittent, sometimes lateralized chin twitching lasting over a week for a seven years period. He reported understanding what was said but had difficulty replying due to the chin movement. The EEG during the episode showed paroxysms of polyspike and slow wave activity, maximal over the fronto-central regions, correlating with the chin movements. Brain imaging was normal. On one occasion, the episode was followed by a generalized tonic-clonic seizure. Levetiracetam added to valproate resolved the episode.
The authors along with video presentation guide the reader to the interesting differential diagnosis of this peculiar case with late onset long-lasting repetitive myoclonia localized to the perioral area with preserved consciousness. Published with videosequences
Extreme startle and photomyoclonic response in severe hypocalcaemia
Marcello Moccia, Roberto Erro, Elvira Nicolella, Pasquale Striano, Salvatore Striano
Epileptic Disorders. Volume 16, Number 1, 13-18, March 2014
Moccia and colleagues report a case with episodes of sudden generalised muscle contractions resulting in violent falls with injuries and urinary incontinence. The fits appeared to relate to sudden auditory stimuli. During the examination, a sudden and unexpected noise triggered a violent startle with a forceful closure of eyes, cranial muscle contraction, and raising of arms over the head, immediately followed by generalised stiffness for several seconds. Flashing light triggered an excessive startle followed by myogenic potentials. There was no epileptic activity on the EEG. Blood tests revealed severe hypocalcaemia and the symptoms disappeared after calcium supplementation.
This report teaches us that electrolyte disturbances can be associated with abnormal startle responses. Published with videosequences
Confirming an expanded spectrum of SCN2A mutations: a case series
Dena Matalon, Ethan Goldberg, Livija Medne, Eric D. Marsh
Epileptic Disorders. Volume 16, Number 1, 13-18, March 2014
Comments by Associate Editor Aristea S. Galanopoulou MD PhD
Mutations in voltage-sensitive sodium channels (SCN) have been increasingly identified in human epilepsy syndromes. These syndromes include both “benign” forms (e.g., benign familial neonatal-infantile epilepsy) and more severe types (e.g., Dravet syndrome, infantile epileptic encephalopathies). Matalon and colleagues here describe the clinical features of 3 girls with 3 different de novo SCN2A mutations that presented with early onset epilepsies, poor developmental outcomes and axial hypotonia. Thinning of the corpus callosum was eventually identified in two of the patients. Two of the girls manifested infantile spasms whereas the third had neonatal tonic seizures. In one of the patients with infantile spasms choreiform movements were also observed.
Of interest, a subsequent independent study by Hackenberg et al (Neuropediatrics, 2014) describes an identical mutation (c.4025T>C) of the SCN2A gene in a different girl who also presented with infantile spasms, choreiform movements, hypersomnia and progressive brain atrophy. These observations lend support to the pathogenicity of this specific mutation but also to its functional impact on both cortical and subcortical structures. Matalon et al nicely review the literature on genotype-phenotype correlations of the known human SCN2A mutations, discussing the inherent heterogeneity but also increasing evidence for a possible involvement of these mutations as modifiers of human epilepsies. Further studies are certainly needed to confirm the functional consequences of these mutations in the developing brain. The need for creation of comprehensive public access genotype-phenotype databases and animal models of the known and emerging epilepsy-related mutations is however becoming increasingly evident, so as to best study their clinical and pathogenic relevance.