Epileptic Disorders
MENUStereo-electroencephalography (SEEG) in 65 children: an effective and safe diagnostic method for pre-surgical diagnosis, independent of age Volume 16, issue 3, September 2014
- Key words: SEEG, stereo-electroencephalography, surgery, presurgical, diagnosis, children, outcome
- DOI : 10.1684/epd.2014.0679
- Page(s) : 280-95
- Published in: 2014
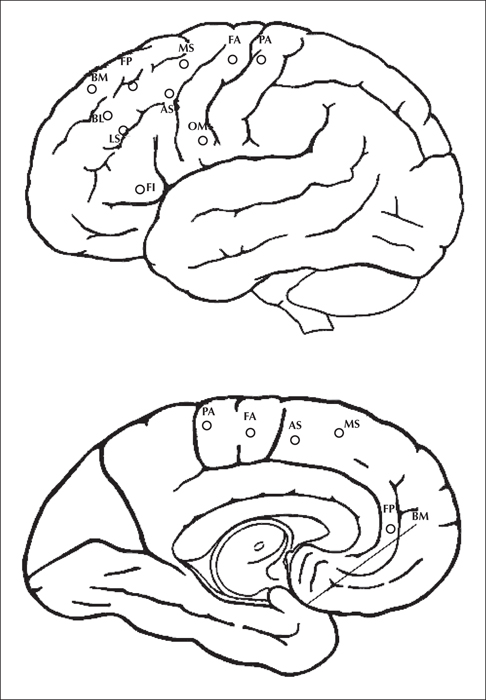
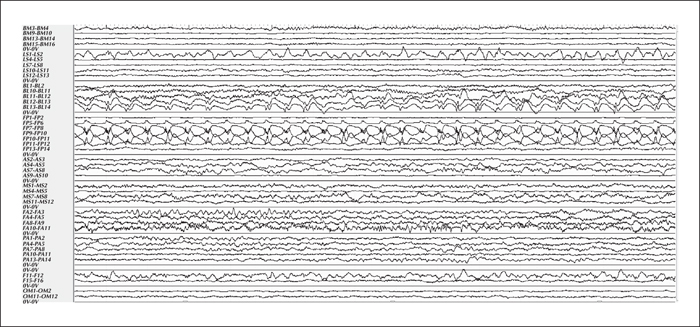
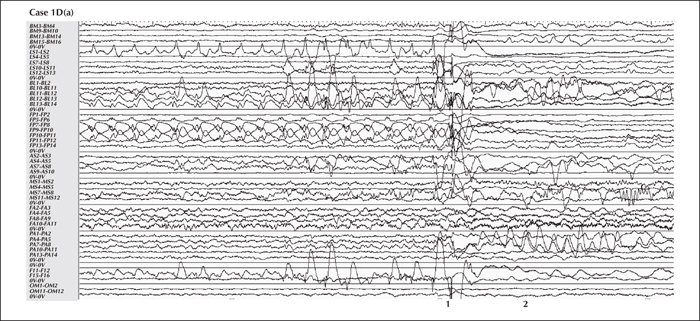
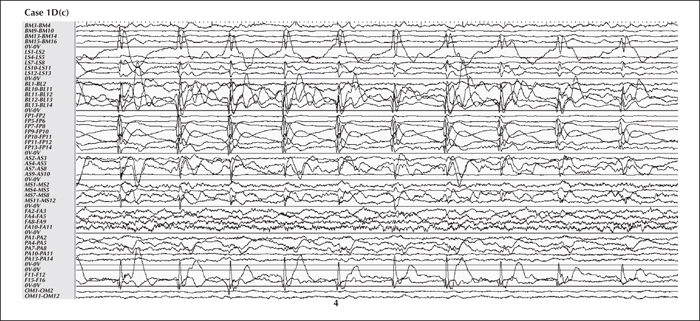
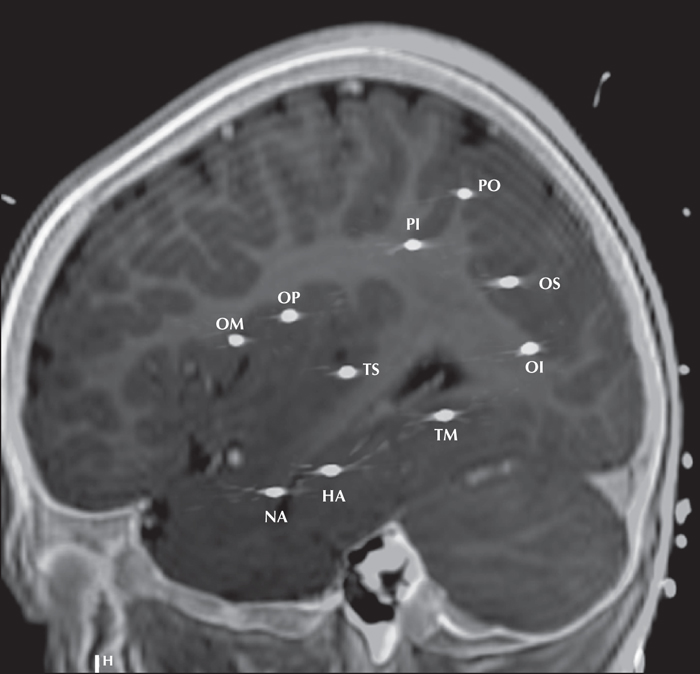
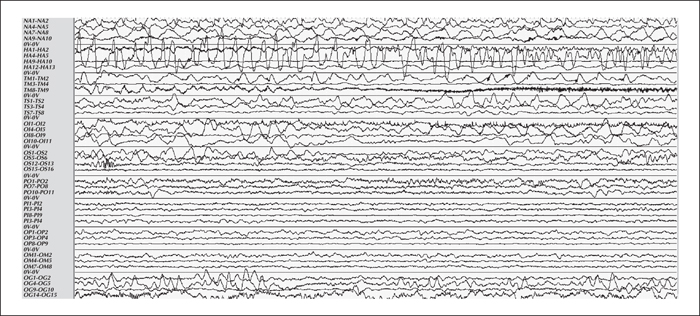
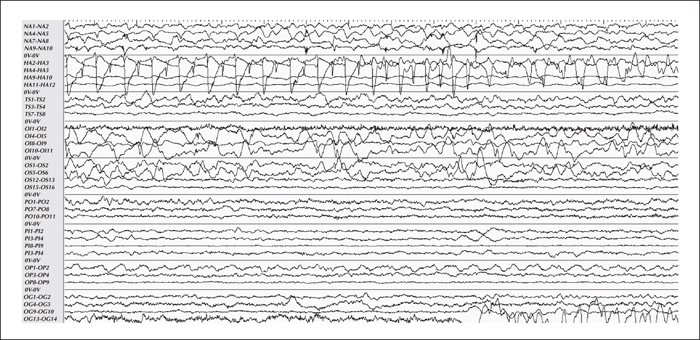
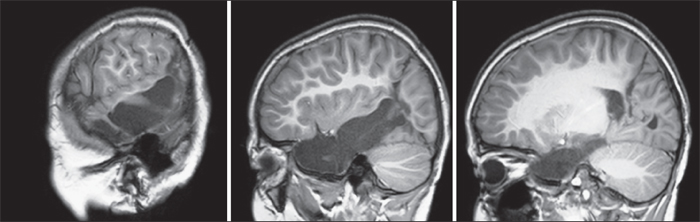
Aim. We report our experience of stereoelectroencephalography (SEEG) in 65 children with drug-resistant seizures, with a particular emphasis on young children. Methods. We retrospectively studied all SEEG performed between 2009 and 2011 in our centre. As SEEG can have several indications, the patients were classified into three categories, according to the probability of surgery. The contribution of SEEG to the final decision regarding surgery was evaluated for each category separately. We also compared the main demographic and surgical data of children younger than 5 years of age (Group 1; 21 children) with those older than five years of age at the time of investigation (Group 2; 44 patients). Results. MRI was not contributory in 20% of patients (9.5% in group 1; 25% in group 2). Electrical stimulations localised the motor area in all patients when performed (49% of patients), even in group 1 (62% of patients). SEEG led to surgery in 78% of patients (90.5% in group 1; 73% in group 2), after a second invasive investigation in 9.2 % of patients. The resection involved more than one lobe in 25% of patients (37% in group 1; 19% in group 2). Ultimately, 78% of patients with a low probability of having surgery before SEEG received surgery (88% in group 1). The surgical outcome of Engel class 1 was reported for 67% of patients (79% of patients in group 1 and 59% in group 2). No complications occurred. Conclusion. SEEG in children is safe and useful, and the surgical outcome in younger children is as good as, or sometimes even better than, that in older children. As a result of lower rates of complication and morbidity, SEEG appears to be more appropriate, in comparison to subdural grids, in situations where it is unclear if patients will have surgery after an invasive investigation.