Epileptic Disorders
MENUClassification of paroxysmal events and the four-dimensional epilepsy classification system Volume 21, issue 1, February 2019
Videos
Figures
Tables
Physicians are frequently called upon to see patients with paroxysmal events. We use the non-specific term “paroxysmal events” when we do not have sufficient evidence to diagnose with certainty whether a paroxysmal event is epileptic or non-epileptic. The paroxysmal events we evaluate as physicians, however, may be epileptic or non-epileptic. For this, we divide the paroxysmal events into epileptic paroxysmal events and non-epileptic paroxysmal events (table 1).
Once we have diagnosed that a paroxysmal event is epileptic in nature, we define the four dimensions that characterize epileptic paroxysmal events: ictal semiology, epileptogenic zone, etiology, and comorbidities.
On the other hand, if we diagnose non-epileptic paroxysmal events, we classify these as psychogenic or organic paroxysmal events. Once we confirm that a non-epileptic paroxysmal event is psychogenic in nature, we define the following three dimensions: paroxysmal event semiology, etiology, and comorbidities. In this case, we use the same semiological seizure classification used for epileptic events (see below) but replace the expression “seizure” by “event” and the expression “aura” by “aura event.” The classification of non-specific “paroxysmal events” (physician does not know if the event is epileptic or not) follows the same system as the classification of non-epileptic psychogenic paroxysmal events.
Finally, if we diagnose a patient with a non-epileptic organic paroxysmal event, we also specify the three dimensions: semiology, etiology, and comorbidities. In this case, however, the semiology is defined by the type of non-epileptic, non-psychogenic event as, for example, syncope, resting tremor, cataplexy, etc.
Following a detailed description of the 4-dimensional epilepsy classification presented below, we also included 12 educational vignettes (Appendix 1) and three more detailed case reports (Appendix 2) classified using the 2017 classifications of the ILAE (Fisher et al. 2017; 2017b) and the four-dimensional epilepsy classification described below. In addition, a case is described (Appendix 3) which is classified using the four-dimensional epilepsy classification with different degrees of precision by an emergency department physician, a neurologist, and an epileptologist.
General organization of the classification system
(1) The dimensions that characterize all the paroxysmal events are independent and defined by different diagnostic methods. For example, a patient may have bilateral clonic seizures (defined by semiology), but the MRI shows an extensive left fronto-temporal tumor (epileptogenic lesion) and the epileptogenic zone is most likely the left frontal lobe (mainly defined by interictal and ictal EEG). The independence of the different dimensions allows precise correlations between the different dimensions. For example, the four-dimensional classification of the epilepsies permits us to calculate the percentage of patients who have no focal ictal findings by semiology but have a focal epilepsy. Because of the independence of the four dimensions, the classification system permits an almost infinite number of correlation studies between the different subgroups included in each dimension.
(2) The classifications of the paroxysmal events and the four dimensions that classify the epilepsies follow the same hierarchal system. The target parameter (namely one of the dimensions) is first subdivided into broad categories and each of them is again subdivided into more specific subcategories. In many cases, these again are subdivided into even smaller categories. In other words, as we move from “left to right”, we find that the dimension is progressively defined more accurately.
The tables that follow provide a global overview of the 4-dimensional classification.
For example, in the classification of paroxysmal events (table 1), the broadest category is “paroxysmal event” that includes all the subcategories mentioned, and the second broadest category is epileptic vs non-epileptic paroxysmal events. Non-epileptic paroxysmal events are, in turn, subdivided into psychogenic and organic paroxysmal events.
The purpose of organizing the different categories into progressively smaller subgroups has the following objectives:
(i) Non-specialists who do not have the tools and knowledge to make a very precise classification of the epilepsies or other paroxysmal events can still use this classification system by just defining the broadest categories (“on the left hand of the table”). For example, if they just know that the patient was depressed and had a paroxysmal episode with generalized “twitching”, unresponsiveness, and no memory for the event afterwards, they can classify the event as follows:
Paroxysmal event:
Semiology:bilateral clonic event (LOC)
Etiology:unknown
Co-morbidities:depression
The same patient seen by an expert might obtain a detailed history from a family member who witnessed the seizure. The expert could elucidate semiological details that make the probability of an epileptic seizure much more likely (initial ictal cry, tonic phase in decerebrate posture lasting 30 seconds followed by a clonic phase lasting 1-2 minutes, “rolling back of the eyes”, blood-tainted foaming at the mouth, postictal coma with gradual recovery of consciousness over 10-25 minutes, urinary incontinence, etc.) Besides, the expert could uncover that the patient was taking a high dose of bupropion. This would lead to the following diagnosis:
Epileptic paroxysmal event:
Semiology:bilateral tonic-clonic seizure
Epileptogenic zone:generalized
Etiology:bupropion treatment
Co-morbidities:depression
(ii) As mentioned above, this classification is organized first into broad categories that are subsequently subdivided into more specific subgroups. This strategy greatly simplifies the definition of the subgroups, as all subgroups must comply with the definition of the main group. This usually also implies similarities between the pathophysiology of all the subgroups. For example, all auras consist of purely subjective ictal symptoms that tend to occur at the beginning of a clinical seizure and with few exceptions are only seen in patients with focal epilepsy. The different subgroups (visual aura, auditory aura, somatosensory aura, etc.) differ according to the type of subjective symptom and the location of the symptomatogenic zone.
Four-dimensional epilepsy classification
Epilepsy is defined as an enduring condition in which brain regions in both hemispheres or part of the brain has an abnormally low threshold to trigger seizures. The part of brain with this characteristic is called the epileptogenic zone. The clinical manifestations of epilepsies are called epileptic seizures and symptomatology is determined primarily by the location of the epileptogenic zone. The impetus to classify epilepsy and seizures is to improve epilepsy management and prognosis and to facilitate communication and enhance epilepsy-related research.
Whenever we classify a disease, we should define the objective of the classification a priori. With the advent of objective medicine in the middle of the 19th century, brain diseases have usually been classified along the following four axes:
- –Clinical semiology (Example: resting tremor, rigidity, etc. in Parkinson's disease);
- –Location of the disease (Example: substantia nigra in patients with Parkinson's disease);
- –Etiology (Example: degenerative disorder in Parkinson's disease);
- –Co-morbidities (Example: dementia in Parkinson's disease).
A four-axis classification of a neurological disease gives an excellent overview of the disease, covering not only pathophysiology but also essential information necessary for its management and prognosis. In the specific case of epilepsy, the four axes refer to the following parameters:
- –Clinical semiology = semiology of epileptic seizures;
- –Location of the disease = epileptogenic zone;
- –Etiology = etiology of the epilepsy;
- –Co-morbidities = associated co-morbidities.
The ictal semiology is the clinical manifestation of the epilepsy. The seizure semiology and the frequency of the seizures will guide our diagnosis and management. In a patient with generalized epilepsy, clinical ictal semiology also dictates the antiepileptic drugs that will be most effective to control the epileptic seizures. In a patient with focal seizures refractory to medical treatment, ictal semiology is an important piece of information to decide if a patient is a surgical candidate.
Definition of the epileptogenic zone is essential in the management of the epilepsy:
- –Focal epilepsies and generalized epilepsies frequently respond best to different types of antiepileptic medication.
- –For surgical treatment of epilepsy, precise definition of the location and extent of the epileptogenic zone is indispensable.
Etiology in most patients is another essential factor that guides treatment and prognosis.
Finally, knowledge of the main co-morbidities is essential to get a complete picture of the patient's disease, particularly cognitive impairment and psychiatric abnormalities. Besides, comorbidities such as severe renal, hepatic or psychiatric disease may greatly influence the type and dose of antiepileptic drug to use, or even the patient's candidacy for surgery.
As already mentioned above, it is essential that the different dimensions in a multi-dimensional classification system be as independent as possible. In other words, classifying one category in a dimension should not automatically define another dimension. For example, classifying the epileptogenic zone as “regional” should not force a classification of the seizure as “focal” and classifying the seizure as “focal” should not force classification of the epileptogenic zone as “regional.” Ideally, to achieve independence in each dimension, the tests and criteria we use to define each dimension should not overlap. Independence of the different dimensions also allows us to evaluate correlations between them. Example: type of semiological seizures in patients with temporal or frontal epileptogenic zones. A typical example of violating this rule of independence is the latest version of the ILAE classification of epilepsies and seizures (Fisher et al., 2017a, 2017b; Berg et al., 2010). In this classification system, all test results are used to classify both seizures and epilepsies. Therefore, no correlation studies are possible, and defining the seizures already defines the type of epilepsy.
Classification of epileptic seizures (Refer to tables 2, 3, 4, 5, 6, 7)
Investigators have taken the highly successful and biologically relevant classification of plants and animals as a template to create a similarly relevant classification of epileptic seizures. Plants and animals contain genetic evolutionary information that naturally leads to a biologically relevant classification. However, it is impossible to develop a “biologically relevant classification” system for objects, since the information contained within varies, for example, wooden boxes of different shapes, sizes, and colors. This fundamental difference in the subject matter largely explains why the ILAE's Committees have been unsuccessful in developing a biologically relevant classification of epileptic seizures that is similar to the classification of plants and animals by Linnaeus. On the other hand, the semiological characteristics of epileptic seizures contain highly relevant information regarding the origin and spread of epileptic discharges. Therefore, any classification of epileptic seizures should maximize the value of seizure semiology regarding the origin and spread of epileptic discharges.
The following principles guide the semiological seizure classification:
- –Epileptic seizures are broken down into “seizure components”. Each seizure consists of 1-4 seizure components.
- –Seizure components consist of sets of ictal symptoms that have semiological similarities and frequently a common pathophysiology, such as a common symptomatogenic zone. In other words, each seizure component tends to be triggered by a defined pathophysiology, i.e. activation of a defined symptomatogenic zone in most cases. For example: a left-hand somatosensory aura corresponds to a symptomatogenic zone in the right hemispheric hand S1 area.
- –The different seizure components are linked in a sequence by arrows. The “sequence of seizure components”, with each seizure component usually corresponding to a more or less clearly defined symptomatogenic zone, elucidate the most likely seizure spread. For example, the seizure of a patient having an aura of flashing lights in the left visual field, progressing to a sensation of nausea, chewing automatisms with loss of contact, and eventually becoming bilateral clonic, would be classified as follows:
(1) left visual aura → (2) abdominal aura → (3) automotor (LOC) → (4) bilateral clonic seizure
From this classification, we would assume that the seizure started in the right calcarine gyrus and then spread into the mesial temporal region before becoming generalized.
The concept that seizures spread and that the semiological evolution of epileptic seizures reflects the “march” of the epilepsy over the cortical surface was already applied first by Bravais in 1827 (Bravais, 1827) and was later adopted and expanded by Jackson (Taylor, 1958).
The semiological seizure classification assumes also that clinical seizures may sometimes remain limited to the first component (left visual aura in the example given above, under Point 3), occasionally spread to component 2 or 3 (left hand clonic component and left versive component in the example above), and become bilateral only rarely. If needed, this can be documented as follows:
Ictal semiology: (1) left visual aura → (2) left hand clonic → (3) left versive → (4) bilateral clonic seizure
Frequency:(1) one/week; (2) one/month; (4) one/six months
Exclusively subjective components are followed by the expression “aura” (examples: left visual aura, abdominal aura). All the objective components are expressed by adjectives (example: left hand clonic, right versive) except the last component that is followed by the expression “seizure” when classifying an epileptic paroxysmal event, or “event” when classifying a non-epileptic event or a paroxysmal event that could be epileptic or non-epileptic.
In the semiological seizure classification, a total of four seizure components are allowed. This restriction avoids excessive detail that might make the classification impractical. However, additional signs that add lateralizing/localizing power may be added to the classification. In the example of Point 3 above, we could add a “left Todd's paralysis” as a lateralizing sign. Besides, if a seizure consists of more than four seizure components and some of the redundant seizure components have lateralizing value, they can be listed under “lateralizing signs”. Table 5 shows the lateralizing signs that can be identified during epileptic ictal events.
Ictal semiology:(1) left visual aura → (2) left hand clonic → (3) left versive → (4) bilateral clonic seizure
Frequency:(1) one/week; (2) one/month; (4) one/six months
Lateralizing signs:left Todd's paralysis; left face tonic
Loss of consciousness (LOC), defined as relative unresponsiveness associated with amnesia for the episode of unresponsiveness, is an essential semiological feature. In previous classifications, loss of consciousness was the main factor dividing focal seizures into simple or complex partial seizure (Bancaud et al., 1981). In the semiological seizure classification, LOC is indicated by adding the notation “(LOC)” following the first seizure component for which the patient is relatively unresponsive and amnestic. In the example shown above a “(LOC)” will be inserted after the left hand clonic component if the patient was unresponsive during the clonic seizure component and does not remember the left clonic movements:
Ictal semiology:(1) left visual aura → (2) left hand clonic (LOC) → (3) left versive → (4) bilateral clonic seizure
Frequency: (1) one/week; (2) one/month; (4) one/six months
All epileptic seizures develop as the consequence of one or more triggers that lower the epileptic threshold. In most cases, these triggers are unknown. In some patients, however, a clearly defined trigger may be identified. Triggers that can elicit epileptic seizures are shown in table 7. Triggers are listed in the seizure classification; as shown below. The approximate percentage of seizures provoked by the trigger is listed following each trigger.
Example:
Ictal semiology:automotor seizure (LOC)
Frequency:one/month
Trigger:music (100%)
Tables 2, 3, 4 show the seizure classification. Table 2 shows the broadest categories, which are less precise and more useful to non-neurologists. Table 3 shows more detailed seizure components that can be seen during epileptic ictal events. General neurologists should have enough ictal semiology training to apply this degree of semiological precision. Finally, table 4 shows the maximum semiological detail and should be used primarily by epileptologists.
Like other dimensions, the seizure components are grouped in major sets that share similar semiological features and frequently also a similar pathophysiology (example: auras that all consist of subjective symptoms tend to occur at the beginning of a seizure and are the result of epileptiform dysfunction of a relatively limited cortical territory). As we move from left to right within the table, we find that the dimension is progressively defined more accurately. Having “seizure components” that cover all possible ictal semiological manifestations has significant advantages:
- –By design of the seizure components, any epileptic seizure can be classified semiologically.
- –Breaking down the seizure symptoms into seizure components and expressing the seizure evolution by joining different seizure components by an arrow makes it possible not only to classify the seizure symptomatology, but also to express the infinite possible patterns of evolution.
- –The same semiological seizure classification can be applied to classify newborns, children, and adults. Epileptologists only need to be aware that certain seizure components do not occur or cannot be diagnosed for certain age groups (for example, automotor seizures do not occur until age three years, and auras are not, or cannot, be reported until age 3-5 years) (Fernandez-Baca Vaca et al., 2018).
- –The same classification system can also be used to classify other paroxysmal episodes and non-epileptic psychogenic paroxysmal episodes. However, in this case, the expression “aura” is replaced by “aura event”, and the expression “seizure” is replaced by “event” at the end of the sequence of components (example: visual aura (bilateral clonic event).
Many of the auras, seizure components or seizures require a somatotopic modifier to define the semiology precisely. Examples include left visual aura, right hand somatosensory aura, and bilateral asymmetric tonic seizure component. Auras, seizure components, or seizures that may be modified by a somatotopic modifier are indicated by an asterisk in tables 2, 3, 4. Table 6 shows the somatotopic modifiers that are used. For some auras, seizure components or seizures, “left” or “right” may only be used as a somatotopic modifier (example: left auditory aura). Other auras, seizure components or seizures allow a detailed somatotopic modifier (example: left hand somatosensory aura).
Tables 2, 3, 4 also include a sixth category, labelled as “asymptomatic EEG seizures.” In the epilepsy classification, the “epileptogenic zone” will essentially define the location of the EEG seizure. This category also allows specification of the frequency of the EEG seizures.
Classification of the epileptogenic zone (table 8)
The epileptogenic zone is defined as the minimal cortical region that must be resected, disconnected, thermo-coagulated, thermo-ablated or desynchronized by multiple transections to produce seizure freedom. It cannot be determined directly but it is deduced by outlining related cortical areas, including the irritative zone, the seizure onset zone, the epileptogenic lesion, the symptomatogenic zone, and the functional deficit zone.
The epileptogenic zone can also be defined with different degrees of precision; for example, by just listing the abnormal hemisphere (left or right), one or two lobes (left fronto-temporal, right occipital) or subdivision of one lobe (left mesial temporal lobe, right fusiform gyrus, etc.). Obviously, without performing surgery, the exact location of the epileptogenic zone cannot be determined with certainty. Besides, if a patient becomes seizure-free after surgery, it only indicates that the epileptogenic zone is a subset of the resected cortex; it does not mean that all the resected tissue is part of the epileptogenic cortex.
Etiological classification (table 9)
In this classification system, special attention is given to classification of the etiology of each epilepsy with maximum precision depending on the available information. The etiology is subdivided into five broad categories, as suggested by the ILAE (Scheffer et al., 2017). For each patient, however, the most detailed etiology is indicated in parenthesis. It is the detailed etiological classification that permits the clinician to associate a specific etiology with a specific medical therapy or epilepsy surgery.
Structural refers to causes for which the seizures are the direct result of an abnormal underlying brain anatomy. Structural lesions are usually diagnosed by neuroimaging, commonly high-resolution MRI.
Genetic refers to causes for which the seizures are a direct result of a known or presumed genetic error.
Infectious refers to causes for which the development of seizures is the result of post-infectious processes.
Inflammatory refers to causes for which the development of seizures is immune-mediated central nervous system inflammation.
Unknown.
General principles guiding the etiology of epileptic seizures:
- –In all patients, the etiology of the seizures is multifactorial, including at least one (and sometimes more than one) main etiological factor (example: left parietal ganglioglioma) and a number of contributing factors, such as susceptibility genes. As genetic testing becomes routine, the multi-etiological nature of epilepsy will become more evident.
- –In general, for patient management, just specifying the broad main etiological category is of no or only minimal value. Therefore, we encourage the specification of the most precise category in each case (example: left middle cerebral artery infarction; SCN1A mutation).
Epileptic syndromes
Epilepsy syndromes consist of specific constellations of:
- –semiologies
- –EEG abnormalities
- –comorbidities
- –etiologies
Syndromes were defined by astute epileptologists who realized that the correct identification of an epilepsy syndrome was often helpful to determine prognosis and treatment. Syndromes, however, are, by definition, empirical and artificial. Modern diagnostic techniques including MRI and genetic testing now allow precise diagnosis of epilepsy causes, therefore identification of syndromes is less important than it once was (Kellinghaus et al., 2004), although several still impact therapy decisions (e.g. West syndrome, self-limited Rolandic epilepsy, juvenile myoclonic epilepsy) or have relevance to genetic research (e.g. Dravet syndrome).
As diagnostic technology and knowledge about epilepsy improve, it is likely that more syndromes will become obsolete in the near future. The emphasis of a classification scheme should not be to preserve a set of increasingly archaic conventions, but rather to define, as precisely and objectively as possible, the characteristics of each individual case of epilepsy in order to facilitate discovery of new etiologies.
However, for many decades, classic epileptology assumed that identification of an epilepsy syndrome was the diagnostic gold standard. Besides, there are innumerable publications on study treatment and prognosis for different epileptic syndromes. This information is useful for management of epileptic patients who have a well-defined epilepsy syndrome. This is the reason why we decided to include the syndrome as an option in parenthesis following the definition of the epileptogenic zone.
Example:
Epileptic paroxysmal event
Semiology:bilateral myoclonic → bilateral clonic → bilateral tonic-clonic seizure
Trigger:sleep deprivation, alcohol withdrawal
Epileptogenic zone:generalized (juvenile myoclonic epilepsy)
Etiology:genetic
Comorbidities:none
Disclosures
None of the authors have any conflict of interest to declare.
Annexe A Appendix 1. PRACTICAL EXERCISE: CLASSIFICATION USING THE ILAE AND PAROXYSMAL EVENT FOUR-DIMENSIONAL EPILEPSY CLASSIFICATION
In this exercise, we replicate the 12 vignettes that Fisher et al. (2017a) included in their “Instructor manual for the ILAE operational classification of sensory types”. The exercise consists of classifying the epilepsy in each case using the ILAE system and the paroxysmal event and four-dimensional system.
When classifying using the ILAE system, the following four levels must be specified:
- a.Seizure type
- b.Epilepsy type
- c.Epilepsy syndrome
- d.Etiology
When classifying using the paroxysmal event and four-dimensional epilepsy classification, the following dimensions must be defined:
Paroxysmal event type:
- I.Ictal semiology
- II.Epileptogenic zone
- III.Etiology
- IV.Co-morbidities
The answers for each case, under both systems of classification, with comments can be found after each vignette.
CASE 1: Unknown-onset tonic-clonic
A woman awakens to find her husband having a seizure in bed. The onset is not witnessed, but she is able to describe bilateral stiffening followed by bilateral shaking. EEG and MRI findings are normal. This seizure is classified as unknown-onset tonic-clonic. There is no supplementary information to determine whether the onset was focal or generalized. Under the old classification, this seizure would have been unclassifiable with no further qualifiers.
ILAE classification
- a.Seizure type: unknown onset tonic-clonic seizure
- b.Epilepsy type: unknown
- c.Epilepsy syndrome: N/A
- d.Etiology: unknown
Paroxysmal event and four-dimensional epilepsy classificationParoxysmal event
- I.Event semiology: bilateral tonic-clonic event
- II.Etiology: unknown
- III.Co-morbidities: none
The vignette does not contain sufficient information to reliably diagnose epilepsy. A detailed anamnesis most likely would have been sufficient to make a reliable diagnosis if the patient had an epileptic seizure or not. The interview should provide an answer to the following questions: Duration of “stiffening” and of “bilateral shaking”?
Duration of “stiffening” and of “bilateral shaking”? Eyes open or closed?
Eyes open or closed? Did the eyes “roll back”?
Did the eyes “roll back”? Was there foaming at the mouth?
Was there foaming at the mouth? Was there blood anywhere?
Was there blood anywhere? Did he wet himself?
Did he wet himself? What happened after the shaking was over? Was there stertorous hyperventilation? How long did it take him to recover consciousness?
What happened after the shaking was over? Was there stertorous hyperventilation? How long did it take him to recover consciousness? Did he complain of muscle ache the following day? Did his tongue hurt? Where did he bite his tongue?
Did he complain of muscle ache the following day? Did his tongue hurt? Where did he bite his tongue?
CASE 2: Focal-onset bilateral tonic-clonic
In an alternate scenario of Case 1, the EEG shows a clear right parietal slow-wave focus. The MRI shows a right parietal region of cortical dysplasia. In this circumstance, the seizure can be classified as focal to bilateral tonic-clonic, despite the absence of an observed onset, because a focal etiology has been identified, and the overwhelming likelihood is that the seizure had a focal onset. According to the old classification, this seizure would have been classified as partial onset, secondarily generalized.
ILAE classification
- a.Seizure type: focal to bilateral tonic-clonic seizure
- b.Epilepsy type: focal
- c.Epilepsy syndrome: N/A
- d.Etiology: genetic and structural
Four-dimensional epilepsy classificationEpileptic paroxysmal event
- I.Ictal semiology: bilateral tonic-clonic seizure
- II.Epileptogenic zone: right parietal
- III.Etiology: right parietal cortical dysplasia
- IV.Co-morbidities: none
Now even without a detailed clinical history, the chances that the patient has an epileptic seizure are extremely high. Therefore, we now classify the event as an epileptic paroxysmal event.
CASE 3: Absence
A child is diagnosed with Lennox-Gastaut syndrome of unknown etiology. EEG shows runs of slow spike-waves. Seizure types include absence, tonic, and focal motor seizures. The absence seizures are prolonged, have indistinct onset and cessation, and sometimes result in falls. In this case, the absence seizures are classified as atypical absence due to their characteristics, the EEG pattern, and underlying syndrome. The absence seizures would have had the same classification in the old system.
ILAE classification
- a.Seizure type: atypical absence, tonic seizure, focal motor seizure
- b.Epilepsy type: combined generalized and focal
- c.Epilepsy syndrome: Lennox-Gastaut syndrome
- d.Etiology: unknown
Four-dimensional epilepsy classificationEpileptic paroxysmal event
- I.Ictal semiology: tonic seizure, dialeptic seizure, motor seizure
- II.Epileptogenic zone: generalized (Lennox-Gastaut syndrome)
- III.Etiology: unknown
- IV.Co-morbidities: intellectual disability
Again, the amnestic information provided in the vignette is inadequate to properly classify the epilepsy. Duration and somatotopic distribution of the tonic seizure.
Duration and somatotopic distribution of the tonic seizure. What do you mean by “focal motor seizure”? In the ILAE classification, a focal motor seizure means that the epileptogenic zone for the motor seizure is focal (or regional). Besides, motor may imply automatisms or atonic, tonic, clonic, hyperkinetic, myoclonic manifestations as also epileptic spams! A good anamnesis certainly can resolve this dilemma.
What do you mean by “focal motor seizure”? In the ILAE classification, a focal motor seizure means that the epileptogenic zone for the motor seizure is focal (or regional). Besides, motor may imply automatisms or atonic, tonic, clonic, hyperkinetic, myoclonic manifestations as also epileptic spams! A good anamnesis certainly can resolve this dilemma. In the vignette, it is mentioned that the patient has Lennox-Gastaut syndrome. This is the reason why we added intellectual disability as a comorbidity.
In the vignette, it is mentioned that the patient has Lennox-Gastaut syndrome. This is the reason why we added intellectual disability as a comorbidity. As we mentioned in the main text, selected syndromes can be useful in the management of epileptic patients. Therefore the four-dimensional classification leaves the option open to include it in parenthesis after listing the epileptogenic zone.
As we mentioned in the main text, selected syndromes can be useful in the management of epileptic patients. Therefore the four-dimensional classification leaves the option open to include it in parenthesis after listing the epileptogenic zone.
CASE 4: Tonic
A child has brief seizures with stiffening of the right arm and leg, during which responsiveness and awareness are retained. This seizure is a focal aware tonic seizure (the words “motor onset” can be assumed). In the old system, the seizure would have been called tonic, with a perhaps incorrect assumption of generalized onset.
ILAE classification
- a.Seizure type: focal aware tonic seizure
- b.Epilepsy type: focal
- c.Epilepsy syndrome: N/A
- d.Etiology: unknown
Four-dimensional epilepsy classificationEpileptic paroxysmal event
- I.Ictal semiology: right tonic seizure
- II.Epileptogenic zone: left hemisphere
- III.Etiology: unknown
- IV.Co-morbidities: none
 The information provided in the vignette is insufficient to establish the epileptic nature of the symptomatology. With the available information listed in the vignette, we would classify this as a “paroxysmal event”, before additional data may confirm that the symptoms are epileptic. The classification listed above is based on the assumption that the epileptic nature of the symptoms has been provided.
The information provided in the vignette is insufficient to establish the epileptic nature of the symptomatology. With the available information listed in the vignette, we would classify this as a “paroxysmal event”, before additional data may confirm that the symptoms are epileptic. The classification listed above is based on the assumption that the epileptic nature of the symptoms has been provided.
 Above is a preliminary classification. Neurological examination and neuroimaging would be essential to properly classify the epilepsy.
Above is a preliminary classification. Neurological examination and neuroimaging would be essential to properly classify the epilepsy.
CASE 5: Focal impaired awareness
A 25-year-old woman describes seizures beginning with 30 seconds of an intense feeling that “familiar music is playing”. She can hear other people talking, but afterwards realizes that she could not determine what they were saying. After an episode, she is mildly confused, and has to “reorient herself”. The seizure would be classified as focal impaired awareness. Even though the patient is able to interact with her environment, she cannot interpret her environment, and is mildly confused. Prior classification would have been complex partial seizure.
ILAE classification
- a.Seizure type: focal impaired awareness seizure
- b.Epilepsy type: focal
- c.Epilepsy syndrome: N/A
- d.Etiology: unknown
Four-dimensional epilepsy classificationEpileptic paroxysmal event
- I.Ictal semiology: déjà-vu aura→ dialeptic seizure
- II.Epileptogenic zone: temporal lobe
- III.Etiology: unknown
- IV.Co-morbidities: unknown
 The information provided in the vignette is insufficient to establish the epileptic nature of the symptomatology. With the available information listed in the vignette, we would classify this as a “paroxysmal event”, before additional data may confirm that the symptoms are epileptic. The classification listed above is based on the assumption that the epileptic nature of the symptoms has been provided
The information provided in the vignette is insufficient to establish the epileptic nature of the symptomatology. With the available information listed in the vignette, we would classify this as a “paroxysmal event”, before additional data may confirm that the symptoms are epileptic. The classification listed above is based on the assumption that the epileptic nature of the symptoms has been provided
 The temporal lobe was identified as the epileptogenic zone because déjà-vu aura(dialeptic seizures almost always originate in the temporal lobe.
The temporal lobe was identified as the epileptogenic zone because déjà-vu aura(dialeptic seizures almost always originate in the temporal lobe.
CASE 6: Autonomic
A 22-year-old man has seizures during which he remains fully aware, with “hair on my arms standing on edge” and a feeling of being flushed. These are classified as focal aware nonmotor autonomic seizures, or more succinctly, focal aware autonomic seizures. Based on the old classification, these would have been referred to as simple partial autonomic seizures.
ILAE classification
- a.Seizure type: focal aware autonomic seizures
- b.Epilepsy type: focal
- c.Epilepsy syndrome: N/A
- d.Etiology: unknown
Four-dimensional epilepsy classificationEpileptic paroxysmal event
- I.Ictal semiology: vasomotor aura → pilomotor aura
- II.Epileptogenic zone: temporal lobe
- III.Etiology: unknown
- IV.Co-morbidities: none
 The information provided in the vignette is insufficient to establish the epileptic nature of the symptomatology. With the available information listed in the vignette, we would classify this as a “paroxysmal event” before additional data may confirm that the symptoms are epileptic. The classification listed above is based on the assumption that the epileptic nature of the symptoms has been provided
The information provided in the vignette is insufficient to establish the epileptic nature of the symptomatology. With the available information listed in the vignette, we would classify this as a “paroxysmal event” before additional data may confirm that the symptoms are epileptic. The classification listed above is based on the assumption that the epileptic nature of the symptoms has been provided The temporal lobe was identified as the epileptogenic zone because vasomotor aura (pilomotor auras almost always originate in the temporal lobe. In many cases, the epileptogenic zone is an inference from the semiology, until additional investigations provide more information. This may not be accurate as the epileptogenic zone may be a non-eloquent area from where the seizure spreads to a symptomatogenic zone.
The temporal lobe was identified as the epileptogenic zone because vasomotor aura (pilomotor auras almost always originate in the temporal lobe. In many cases, the epileptogenic zone is an inference from the semiology, until additional investigations provide more information. This may not be accurate as the epileptogenic zone may be a non-eloquent area from where the seizure spreads to a symptomatogenic zone.
CASE 7: Focal clonic
A one-month-old boy has rhythmic jerking of the left arm that does not remit when repositioning the arm. Corresponding EEG shows right frontal ictal rhythms. These seizures are focal motor onset clonic seizures, or more parsimoniously, focal clonic seizures. Because the level of awareness cannot be ascertained, awareness is not involved in classifying this seizure. No appropriate term exists under the old classification.
ILAE classification
- a.Seizure type: focal clonic seizures
- b.Epilepsy type: focal
- c.Epilepsy syndrome: N/A
- d.Etiology: unknown
Four-dimensional epilepsy classificationEpileptic paroxysmal event
- I.Ictal semiology: left arm clonic seizure
- II.Epileptogenic zone: right frontal lobe
- III.Etiology: unknown
- IV.Co-morbidities: none
None.
CASE 8: Sequential seizure manifestations
A seizure begins with tingling in the right arm of a 75-year-old man. The patient says that it then progresses to rhythmic jerking of the right arm, lasting for about 30 seconds. He retains awareness and memory for the event. This seizure is a focal (non-motor-onset) sensory seizure. Additional description would be useful, namely focal sensory seizure with somatosensory features progressing to right arm clonic activity. If the sensory and motor events were to be discontinuous or the clinician had reason to consider the event to be two separate (bifocal or multifocal) seizures, then each component would be classified as a separate seizure. Under the old classification, this would have been called a simple partial sensorimotor seizure. An advantage of the 2017 classification is specification of the sensory onset, which may have clinical importance.
ILAE classification
- a.Seizure type: focal sensory seizure
- b.Epilepsy type: focal
- c.Epilepsy syndrome: N/A
- d.Etiology: unknown
Four-dimensional epilepsy classificationEpileptic paroxysmal event
- I.Ictal semiology: right arm somatosensory aura → right arm clonic seizure
- II.Epileptogenic zone: left parietal
- III.Etiology: unknown
- IV.Co-morbidities: none
 The information provided in the vignette is insufficient to establish the epileptic nature of the symptomatology. With the available information listed in the vignette, we would classify this as a “paroxysmal event” before additional data may confirm that the symptoms are epileptic. The classification listed above is based on the assumption that the epileptic nature of the symptoms has been provided
The information provided in the vignette is insufficient to establish the epileptic nature of the symptomatology. With the available information listed in the vignette, we would classify this as a “paroxysmal event” before additional data may confirm that the symptoms are epileptic. The classification listed above is based on the assumption that the epileptic nature of the symptoms has been provided
 The left parietal lobe was identified as the epileptogenic zone because right arm somatosensory aura → right arm clonic seizures almost always originate from the left parietal lobe.
The left parietal lobe was identified as the epileptogenic zone because right arm somatosensory aura → right arm clonic seizures almost always originate from the left parietal lobe.
CASE 9: Myoclonic-atonic
A four-year-old boy with Doose syndrome has seizures with a few arm jerks and then a rapid drop with loss of tone. These are now classified as myoclonic-atonic seizures. Based on prior unofficial usage, these would have been called myoclonic-astatic seizures.
ILAE classification
- a.Seizure type: myoclonic-atonic seizures
- b.Epilepsy type: generalized
- c.Epilepsy syndrome: Doose syndrome
- d.Etiology: unknown
Four-dimensional epilepsy classificationEpileptic paroxysmal event
- I.Ictal semiology: bilateral myoclonic axial atonic seizure
- II.Epileptogenic zone: generalized (Doose syndrome)
- III.Etiology: unknown
- IV.Co-morbidities: none
None.
CASE 10: Myoclonic-tonic-clonic seizures
A 13-year-old with juvenile myoclonic epilepsy has seizures beginning with a few jerks, followed by stiffening of all limbs and then rhythmic jerking of all limbs. These would be classified as myoclonic-tonic-clonic seizures. No corresponding single seizure type exists in the old classification, but they might have been called myoclonic or clonic seizures followed by tonic-clonic seizures.
ILAE classification
- a.Seizure type: myoclonic-tonic-clonic seizures
- b.Epilepsy type: generalized
- c.Epilepsy syndrome: juvenile myoclonic epilepsy
- d.Etiology: genetic
Four-dimensional epilepsy classificationEpileptic paroxysmal event
- I.Ictal semiology: bilateral myoclonic → bilateral tonic-clonic seizures
- II.Epileptogenic zone: generalized (juvenile myoclonic epilepsy)
- III.Etiology: genetic
- IV.Co-morbidities: none
None.
CASE 11: Focal epileptic spasms
A 14-month-old girl has sudden extension of both arms and flexion of the trunk for about 2 seconds. These seizures repeat in clusters. EEG shows hypsarrhythmia with bilateral spikes, most prominent over the left parietal region. MRI shows a left parietal dysplasia. Resection of the dysplasia terminated the seizures. Because of the ancillary information, the seizure type would be considered as focal epileptic spasms (the term “motor onset” can be assumed). Based on the previous classification, these would have been called infantile spasms, with information on focality not included. The term “infantile” can still be used when spasms occur in infancy.
ILAE classification
- a.Seizure type: focal epileptic spasm
- b.Epilepsy type: focal
- c.Epilepsy syndrome: West syndrome
- d.Etiology: genetic and structural
Four-dimensional epilepsy classificationEpileptic paroxysmal event
- I.Ictal semiology: bilateral epileptic spasm
- II.Epileptogenic zone: left parietal (West syndrome)
- III.Etiology: left parietal dysplasia
- IV.Co-morbidities: none
None.
CASE 12: Unclassified
A 75-year-old man, known to have epilepsy, reports an internal sense of body trembling and a sense of confusion. No other information is available. EEG and MRI are normal. This event is unclassified.
ILAE classification
- a.Seizure type: unclassified
- b.Epilepsy type: unknown
- c.Epilepsy syndrome: unknown
- d.Etiology: unknown
Four-dimensional epilepsy classificationParoxysmal event
- I.Event semiology: aura → dialeptic event
- II.Etiology: unknown
- III.Co-morbidities: unknown
 The vignette is very confusing. It indicates that the patient has epilepsy but does not indicate the seizure semiology of “known” epileptic seizures.
The vignette is very confusing. It indicates that the patient has epilepsy but does not indicate the seizure semiology of “known” epileptic seizures.
 The paroxysmal events are very non-specific and could well be non-epileptic paroxysmal events.
The paroxysmal events are very non-specific and could well be non-epileptic paroxysmal events.
 The patient requires additional testing to elucidate the nature of the symptomatology (MRI and video EEG)
The patient requires additional testing to elucidate the nature of the symptomatology (MRI and video EEG)
Annexe B Appendix 2. CASE STUDIES: AN EXAMPLE OF THREE PATIENTS WITH PAROXYSMAL EVENTS
CASE 1
A 20-year-old, right-handed woman presents for evaluation of paroxysmal events. Onset of the events was at age 15.
(1) ANAMNESIS
Per patient: The last thing she remembers before her events is a “weird feeling”, which she cannot further describe, and then she knows that the seizure is coming. This feeling just lasts for few seconds (∼20 seconds). The next thing she remembers is laying on the floor, being surrounded by people and feeling confused. She feels tired and she goes back to sleep until the next day. She does not recall any particular difficulty talking or understanding after her events. She denies any particular pain, such as muscular pain, jaw pain or tongue soreness. She does not recall any episode with urinary incontinence.
Per witness: The mother hears a loud cry at the onset of the episode. Then the patient is unresponsive and turns her head to one side (the mother recalls “to the left”), while her eyes are open and “rolled back”. This is followed by bilateral shaking with arms and legs extended; lasting for about a minute. She does not recall any foaming at the mouth. After the episode, the patient is unresponsive and her breathing is deep and stertorous for several seconds. She is then confused for about 20-30 minutes. No urinary incontinence. When asked, the patient denies recalling any pulling of her head towards one side or the other.
She is currently having 1-2 events a month.
Classification after clinical history
2017 ILAE classification system
- a.Seizure type: focal to bilateral tonic-clonic seizure
- b.Epilepsy type: focal
- c.Epilepsy syndrome: NA
- d.Etiology: unknown
Four-dimensional epilepsy classificationEpileptic paroxysmal event
- I.Ictal semiology: aura → left versive (LOC) → bilateral tonic-clonic seizure
- II.Epileptogenic zone: right hemisphere
- III.Etiology: unknown
- IV.Co-morbidities: none
Comment: The description of the mother is consistent with generalized tonic-clonic seizures. This is also consistent with the history obtained by the patient; no recollection of the generalized convulsions. These facts support the conclusion that the patient has “epileptic paroxysmal events”. Not infrequently, the observers are relatively inaccurate when lateralizing versions. Therefore, after obtaining the clinical history, the seizures could also be classified as follows:
Aura→versive (LOC) →bilateral tonic-clonic seizure.
The epileptogenic zone would be “focal”.
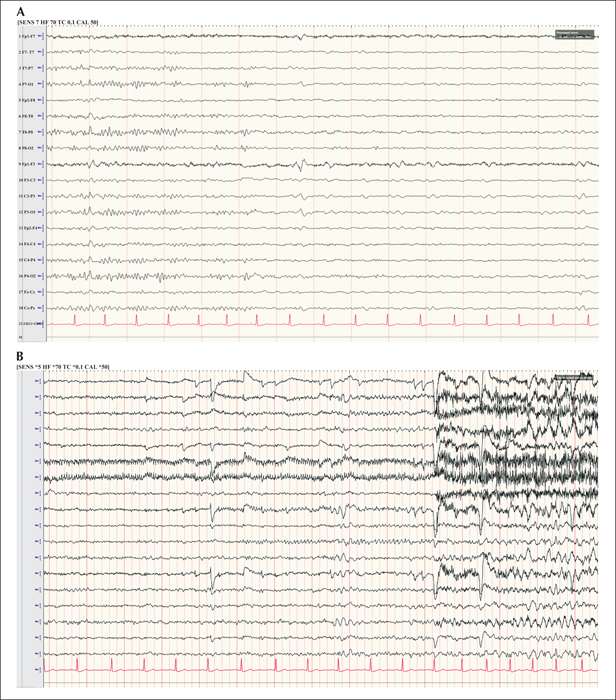
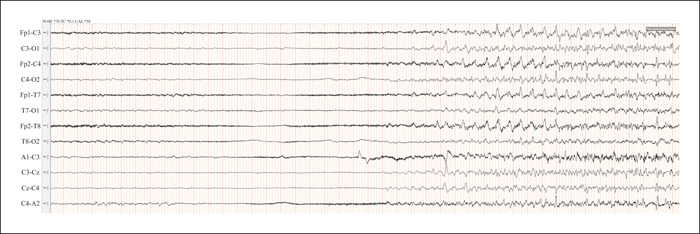
(2) EMU EVALUATION (figure 1A, B and video 1).
Interictal: sharp waves, left frontal (F3-C3)
Ictal: right versive (LOC)→ right face tonic → bilateral asymmetric tonic clonic seizure
Lateralizing signs: right M2e, right sign of 4
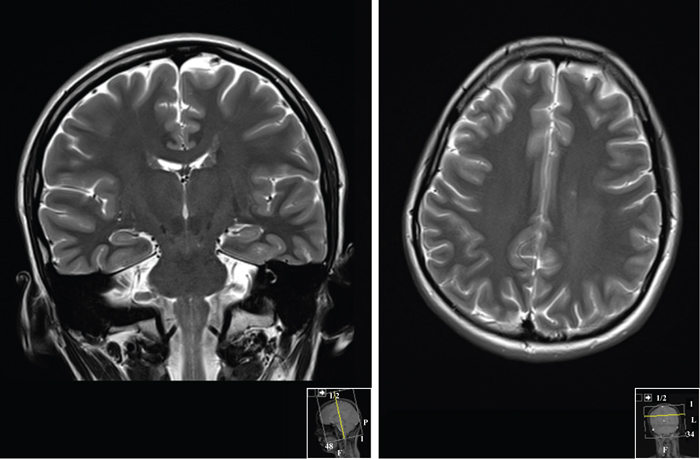
(3) NEUROIMAGING (figure 2).
Small focus of abnormal signal in the left frontal periventricular white matter.
(4) FINAL CLASSIFICATION
2017 ILAE classification system
- a.Seizure type: focal to bilateral tonic-clonic seizure
- b.Epilepsy type: focal
- c.Epilepsy syndrome: NA
- d.Etiology: unknown
Four-dimensional epilepsy classificationEpileptic paroxysmal event
- I.Ictal semiology: aura→ right versive (LOC) → right face tonic → bilateral asymmetric tonic clonic seizure
- II.Epileptogenic zone: left frontal
- III.Etiology: unknown
- IV.Co-morbidities: MRI shows a small focus of abnormal signal in the left frontal periventricular white matter
CASE 2
(1) ANAMNESIS
A 53-year-old, left-handed woman with dyslipidemia and hypothyroidisms presents to the epilepsy clinic for evaluation of paroxysmal events that started at age eight.
Per patient: Her episodes are nocturnal. She wakes up with a feeling “the seizure is coming and I am losing control”. This feeling last for just “a second”. Then, she remembers her left arm shakes uncontrollably. She tries to stop it by grabbing her left arm with the right hand, but she cannot control it. Occasionally, she also feels her legs moving up and down. The episodes last 2-3 minutes. After the seizure, she feels slightly confused, tired, and she has difficulty talking, but she feels she is able to understand. She denies biting her tongue and she only recalls urinary incontinence on one occasion. She feels she is probably aware during the entire episode, but she is not totally sure.
Per witness (husband): The patient suddenly wakes up and yells “help”. Then, she starts moving uncontrollably all over. Her eyes are open. Her arms and legs move up and down. There is no foaming at the mouth, nor eye or head deviation that he recalls. Eyes do not roll up. After the seizure, she seems awake but confused and tired. He is not sure whether she would be able to follow any commands during this time, but she would know that she just had an episode.
On presentation, she was having one episode per week while on two AEDs.
Classification after clinical history
2017 ILAE classification system
- a.Seizure type: focal aware non-motor onset
- b.Epilepsy type: focal
- c.Epilepsy syndrome: N/A
- d.Etiology: unknown
Four-dimensional epilepsy classificationEpileptic paroxysmal event
- I.Ictal semiology: aura → left arm clonic → hypermotor seizure
- II.Epileptogenic zone: right frontal
- III.Etiology: unknown
- IV.Co-morbidities: none
Comment: The duration and stereotypy of the episodes strongly suggests an epileptic paroxysmal episode. Besides, in this case, the patient herself lateralized the clonic seizure. This is usually a reliable lateralizing sign.
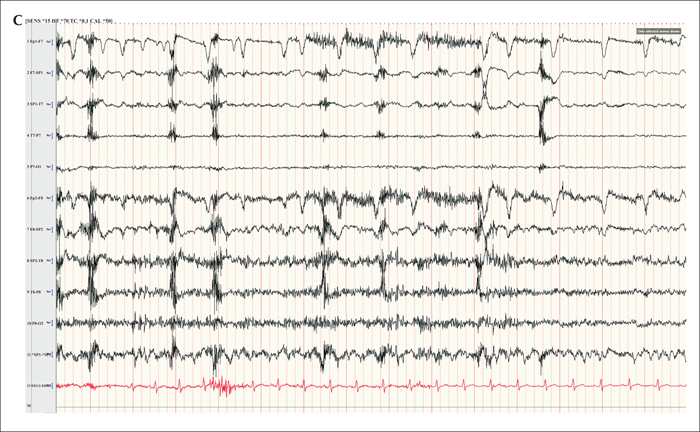
(2) EMU EVALUATION (figure 3A, B, C and video 2)
Interictal: sharp waves, maximum at right temporal electrodes (F8 and Sp2) (figure 3).
Ictal:
-Seizure semiology: emotional hypermotor seizure (video 2)
-EEG seizure pattern: right temporal (figure 3).
Comment: After the EMU evaluation, the seizure semiology classification was adjusted. The “aura” and the “left arm clonic” components were removed from the classification. Her subjective sensation started at the same time as the emotional hypermotor seizure, therefore it was felt to be most likely caused by it. Also, her left arm never moved in a clonic fashion, but rather exhibited complex movements, as expected in a hypermotor seizure. This exemplifies how the four-dimensional epilepsy classification may change overtime as the patient may undergo further investigations.
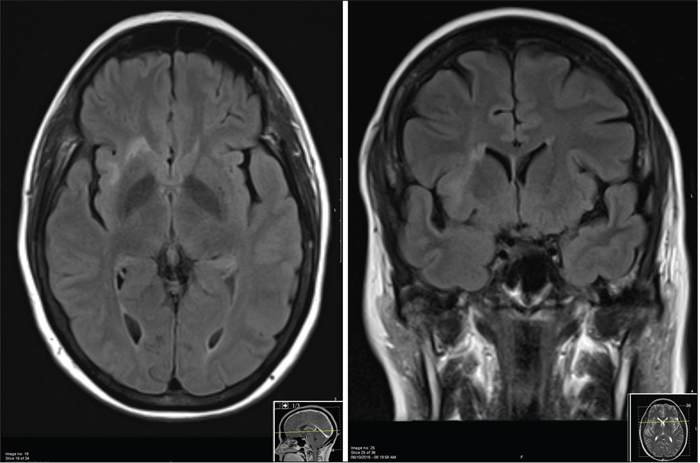
(3) NEUROIMAGING (figure 4)
Axial and coronal FLAIR MRI shows a “comet-like” high signal in the right anterior insula, consistent with a cortical dysplasia. The main juxtacortical lesion has a “tail”, tracking along the expected course of the radial glial fibers to the subependimal margin.
(4) FINAL CLASSIFICATION
2017 ILAE classification system
- a.Seizure type: focal aware hyperkinetic seizure
- b.Epilepsy type: focal
- c.Epilepsy syndrome: NA
- d.Etiology: structural and genetic
Four-dimensional epilepsy classification
- I.Ictal semiology: emotional hypermotor seizure
- II.Epileptogenic zone: right insula
- III.Etiology: structural and genetic (right insular cortical dysplasia)
- IV.Co-morbidities: none
CASE 3
(1) ANAMNESIS
An 11-day-old boy, born full-term, with no complications at birth presents with a five-day history of paroxysmal episodes.
Per witness (parents): Episodes of bilateral shaking of arms and legs which may be preceded by episodes of stiffening. These last for about one minute and are stereotypic. Initial frequency was once a day, but for the last days, the frequency has increased to four episodes a day. The patient's uncle had epileptic seizures during the newborn period which he outgrew during his first year.
Classification after clinical history
2017 ILAE classification system
- a.Seizure type: sequential
- b.Epilepsy type: NA
- c.Epilepsy syndrome: unknown
- d.Etiology: unknown
Four-dimensional epilepsy classificationEpileptic paroxysmal events
- I.Ictal semiology: bilateral tonic → bilateral clonic seizure
- II.Epileptogenic zone: unknown
- III.Etiology: unknown
- IV.Co-morbidities: none
Comment: Again, the duration and stereotypy of the episodes strongly suggests an epileptic paroxysmal episode.
(2) EMU EVALUATION (figure 5 and video 3)
Ictal: bilateral asymmetric tonic → bilateral clonic → left clonic seizure
EEG seizure pattern: generalized.
(3) EVOLUTION
During his initial evolution, blood and urine and metabolic work-up was negative. Lumbar puncture was normal. Seizures responded to phenobarbital. At seven months, he had developed normally and no further seizures were noticed. Therefore, phenobarbital was stopped.
He is currently eight years old. He has growth and development appropriate for his age. He has been seizure-free, off phenobarbital, since age seven months old.
(4) FINAL CLASSIFICATION
2017 ILAE neonatal classification system
- a.Seizure type: sequential seizure
- b.Epilepsy type: NA
- c.Epilepsy syndrome: self-limited neonatal or familial neonatal epilepsy
- d.Etiology: genetic
Four-dimensional epilepsy classificationEpileptic paroxysmal event
- I.Ictal semiology: bilateral asymmetric tonic → bilateral clonic → left clonic seizure
- II.Epileptogenic zone: generalized (self-limited neonatal or familial neonatal epilepsy)
- III.Etiology: genetic
- IV.Co-morbidities: none
Annexe C Appendix 3. CASE STUDY: A PRACTICAL EXAMPLE OF USING THE EPILEPSY CLASSIFICATION WITH DIFFERENT DEGREES OF PRECISION
Case study
A 35-year-old man presents to the emergency department (ED) for a new-onset paroxysmal event that occurred earlier that day. The ED physician gathers some information from the patient's wife who describes the patient having violent shaking of all limbs. The patient now feels that his condition corresponds to baseline. He has also had anxiety and depression for the last five years.
Based on the information gathered by the ED, the physician could try to classify the patient's epilepsy using the epilepsy classification and semiological classification with low or moderate complexity.
Paroxysmal event
Ictal semiology: bilateral motor event
Frequency: one event, hours ago
Etiology: unknown
Comorbidities: anxiety and depression
The patient is seen by a junior neurology resident who has rotated in the epilepsy service a few times. He asks additional questions to the patient's wife. The resident finds out the patient has been having brief episodes of staring and unresponsiveness for the last year, with an approximate frequency of one every month. In addition, he had urinary incontinence and has bitten his tongue today.
Based on the additional information, the resident suspects an epileptic paroxysmal event and he can further develop the epilepsy classification using the more complex semiological classification. At this moment, he is unsure whether the patient may have a focal vs a generalized epileptogenic zone.
Epileptic paroxysmal event
Ictal semiology: (1) dialeptic → (2) bilateral clonic seizure
Frequency: (1) one/month; (2) once today
Epileptogenic zone: unknown.
Etiology: unknown.
Comorbidities: anxiety and depression
The patient is later seen by the epilepsy faculty who accompanies the resident to see the patient again. The part of the interview that focuses on the ictal semiology is outlined below:
Epilepsy doctor:Mr. S, what is the last thing you remember before the episode? I would like you to tell me only your own experience, not what you have been told.
Mr. S:I just recall waking up this morning feeling fine and the last thing I remember is going into the kitchen to get some coffee.
Epilepsy doctor:Anything else unusual preceding the episode that you may remember?
Mr. S:I may have felt nauseated for a second, but I am not sure.
Epilepsy doctor:What is the next thing you remember?
Mr. S:I just remember hearing my wife, asking me questions, like “How are you feeling? Can you stand up?”
Epilepsy doctor:How were you feeling at that point?
Mr. S:I was feeling confused, but otherwise OK.
Epilepsy doctor: Any particular pain?
Mr. S:Not that I can recall.
Epilepsy doctor:What about now? Any particular pain now?
Mr. S:Well... yes, my tongue, my tongue feels swollen and painful. My jaw is sore and I have some muscle aches around my shoulders, but overall, I feel fine. Just tired.
Epilepsy doctor: Your wife has mentioned you may have been having other episodes where you would stare. Were you aware of these?
Mr. S: She has told me before, but I am really not sure what she means.
Epilepsy doctor:Have you been feeling anything else unusual?
Mr. S:Now that you mention... I have been getting this feeling in my stomach... It is like an anxiety or nausea feeling or like being in a roller coaster. And I get this sensation of déjà vu or familiarity, as if I am experiencing something that has happened before. I mentioned this because lately it has gotten quite strong, and makes me even a little scared.
Epilepsy doctor:For how long does it last and how often do you get these sensations?
Mr. S:It is just a matter of seconds. I get these maybe once or twice a week, but for the last few days, I have them almost daily. It was really striking.
Epilepsy doctor:Mrs. S, I would like to ask you a few questions regarding the episodes you have seen. Can you start by describing these staring spells? Can you give me an example?
Mrs. S:Well, the last one I saw, we were seating on the couch, just watching TV, and I just saw him staring.
Epilepsy doctor:But what caught your attention? Anything in particular that made you look towards your husband while watching TV?
Mrs. S:He makes these chewing sounds with his mouth. And I try calling him, but he does not respond.
Epilepsy doctor:For how long does it last for? And what happens afterwards?
Mrs. S:It usually lasts for 1-2 minutes and afterwards he is somewhat confused.
After further questioning the patient's wife, the Epilepsy doctor can gather additional information that is convincing for a generalized tonic-clonic seizure: ictal cry, blood-tainted foaming at the mouth, “eyes rolled back”, tonic phase in decerebrate posture lasting 15 seconds followed by a clonic phase lasting approximately one minute, all followed by postictal coma for 5-10 minutes and gradual recovery.
Based on the additional information, the epilepsy faculty can further develop the epilepsy classification using the semiological classification of moderate complexity.
Epileptic paroxysmal event
Ictal semiology: (1) abdominal aura→ (2) psychic aura → (3) automotor (LOC) → (4) bilateral clonic seizure
Frequency: (1) (2) one/day; (3) one/month; (4) once today
Epileptogenic zone: temporal lobe
Etiology: unknown
Comorbidities: anxiety and depression
We know now that the patient has focal epilepsy, and among the focal epilepsies that can cause this seizure type, the most likely is temporal lobe epilepsy. This maybe correct for now, nevertheless this classification can be further developed and confirmed over time with additional testing, such as EEG, epilepsy monitoring unit (EMU) admission, and MRI of the brain.