Sang Thrombose Vaisseaux
MENUVulvar venous malformations: surgical treatment remains an option Volume 33, issue 2, March-April 2021
- Key words: venous malformations, female external genitalia, vulva, surgery, gynecology
- DOI : 10.1684/stv.2021.1164
- Page(s) : 73-9
- Published in: 2021
Background
Our aim was to evaluate the benefit of surgical resection of the venous malformation (VM) of the external female genitalia.
Methods
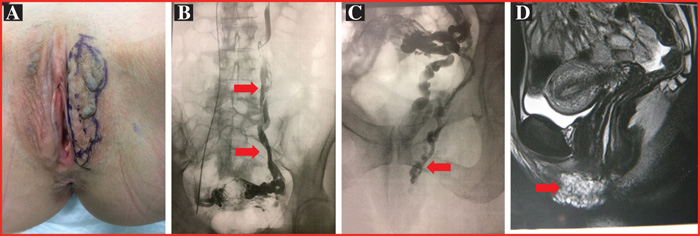
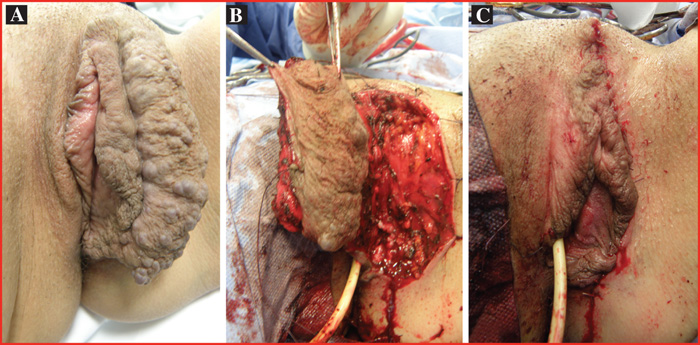
Over the period of 2009-2019, 18 consecutive females underwent surgical resection for vulvar VM. Evaluations included preoperative Doppler ultrasound, MRI, and pre-and postoperative photographic imaging. The main outcomes were: residual pain, cosmetic distortion, residual VM, and quality of life.
Results
Over a 10 year periods, 18 females, mean age 35 years (range 9-71) were included in this study. All patients were symptomatic: 16 had intermittent pain or discomfort, 1 had bleeding and 2 requested cosmetic treatment. Of these cases, there were 5 isolated vulvar VM, 12 associated VM: 3 of the clitoral hood, 3 troncular pelvic vein insufficiency and 12 of the lower limb. Eight patients had undergone previous procedures: 2 sclerotherapy treatments (1 to 3 sessions), 4 partial surgical resections. There were 18 single resections in the vulva (7 focal, 11 complete), 2 partial resections in clitoral hood and 2 had resection of a VM in the peritoneo-vaginal canal at the same time. The mean follow-up was 42. 9 months (range 6-120). Two patients were lost to follow-up at 6 months. For all patients, elimination of pain and soft tissue redundancy was achieved. Two patients had persistent discomfort and 2 requested cosmetic treatment.
Conclusion
Surgical resection of vulvar VM can be the best approach with few postoperative complications, good functional and cosmetic results. Appropriate preoperative evaluation is required to identify isolated VM or VM associated with ovarian vein or internal iliac vein insufficiency requiring to be treated before surgery.