Cahiers Santé Médecine Thérapeutique
MENUPyoderma gangrenosum in chronic inflammatory bowel disease: Three new cases Volume 31, issue 3-4, Mai-Août 2022
- Key words: corticosteroid therapy, pyoderma gangrenosum, chronic inflammatory bowel disease
- DOI : 10.1684/sanmt.2023.144
- Page(s) : 202-7
- Published in: 2022
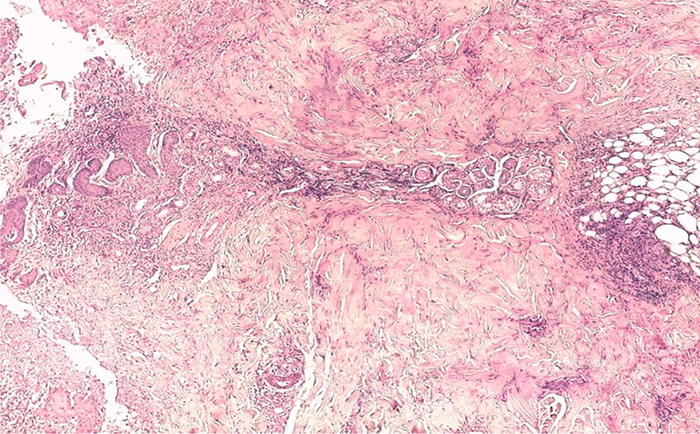
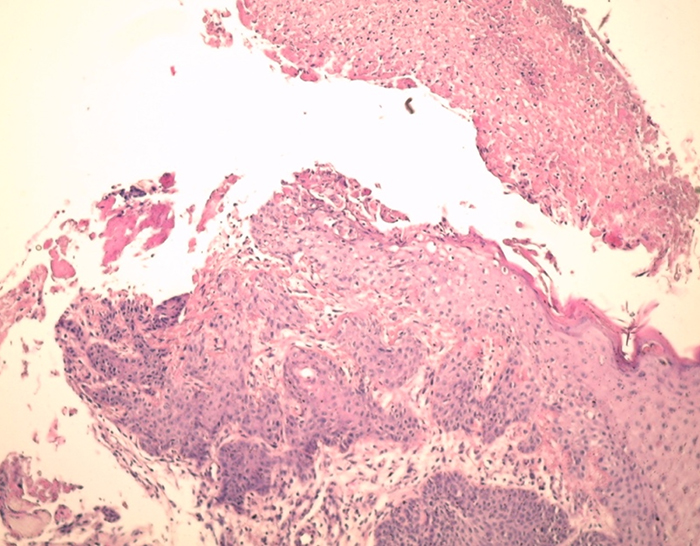
Pyoderma gangrenosum (PG) is an ulcerative form of neutrophilic dermatosis of unknown etiology. It complicates 2 to 3% of inflammatory bowel diseases (IBD). Materials and methods: This is a descriptive monocentric retrospective study of 3 patients with PG associated IBD hospitalized in our hepatogastroenterology department between March 2014 and March 2018. The diagnosis of PG was based on histological study of cutaneous biopsies. Results: Among 176 patients followed for IBD, 3 patients had a PG associated with IBD (2 women and 1 man) i.e. 1.71%. The mean age of the patients was 44 years. The average duration of disease progression was 10 years. One patient had ulcerative colitis (UC) in procto-sigmoiditis, and the other two patients had Crohn’s disease (CD), with a fistulizing and stenosing ileal-colic form in one patient and colic form in the second case. PG was confirmed on skin biopsy in all our patients. In 2 patients, IBD preceded PG. All our patients received systemic corticosteroid therapy. Maintenance treatment was based on azathioprine alone in 2 cases and infliximab in one 1 case. Complete healing of PG was achieved in all patients. Conclusion: The association of PG and IBD is rare but severe and autonomous. The use of TNF-α antagonists have been reported to be effective for PG associated with IBD.