Médecine de la Reproduction
MENUThe impact of female infertility on the occurrence of congenital malformations after assisted reproduction Volume 24, issue 1, Janvier-Février-Mars 2022
- Key words: ART, children, birth defects, health
- DOI : 10.1684/mte.2022.0880
- Page(s) : 91-9
- Published in: 2022
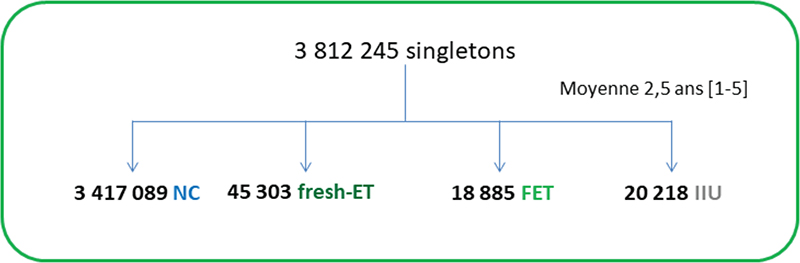
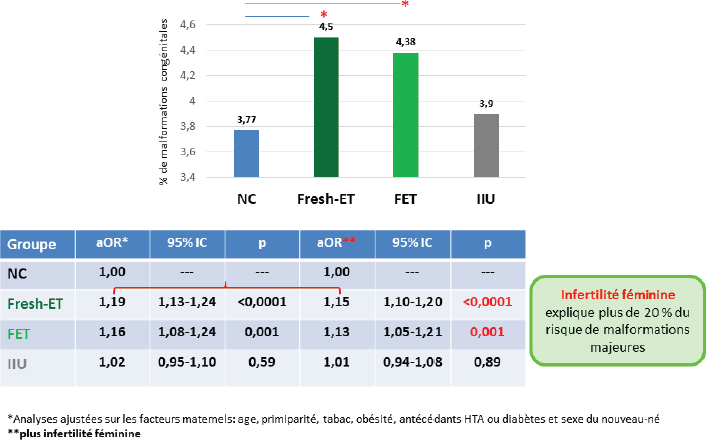
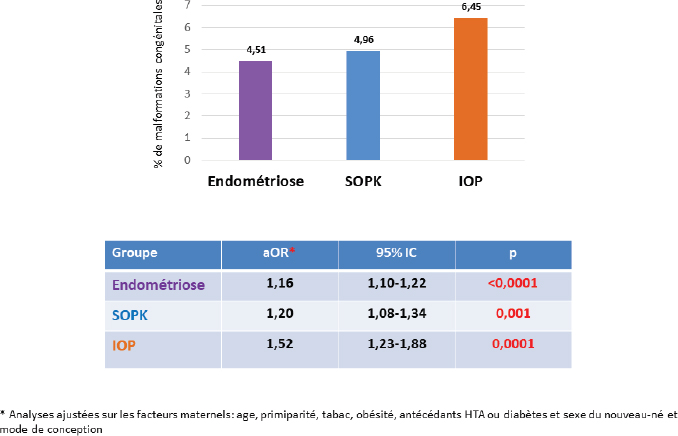
Do in vitro fertilisation (IVF) and intrauterine insemination (IUI) induce an increased risk of congenital anomalies? This is a major question, to which most of the available epidemiological studies unfortunately seem to answer positively. However, these results are based on data obtained at birth or during the neonatal period, on small populations, and above all without taking into account the possible role of underlying female infertility, a potential confounding factor. Using the French National Health System database, we performed a comparative analysisof all singleton births in France over a five-year period (2013-2017), by natural conception (NC), embryo transfer (ET) or IVF. A total of 3,501,496 singleton births were included (3,417,089 NC, 20,218 IUI and 64,188 ET). The risks of major congenital malformations (ICD-10) were investigated according to mode of conception in multivariate analyses using multiple logistic regression models adjusted for maternal age, primiparity, obesity, smoking, history of hypertensionor diabetes and female infertility. The prevalence of malformations after ET was significantly higher than after CN, with adjusted odds ratios (aOR) of 1.15 and 1.13. The overall risk was similar in the IUI and NC groups (aOR of 1.01). An independent and overall increase in risk was observed in the presence of endometriosis (aOR of 1.16), polycystic ovary syndrome (1.20) or premature ovarian failure (1.52). This study therefore shows that causes of maternal infertility are associated with an increased risk of congenital anomalies, in addition to that associated with IVF.