Hépato-Gastro & Oncologie Digestive
MENUEnteral nutrition in medical oncology: Clinical situation Volume 27, issue 10, Décembre 2020
- Key words: Enteral nutrition, digestive cancer, malnutrition, gastrostomy, nasogastric tube
- DOI : 10.1684/hpg.2020.2076
- Page(s) : 1005-12
- Published in: 2020
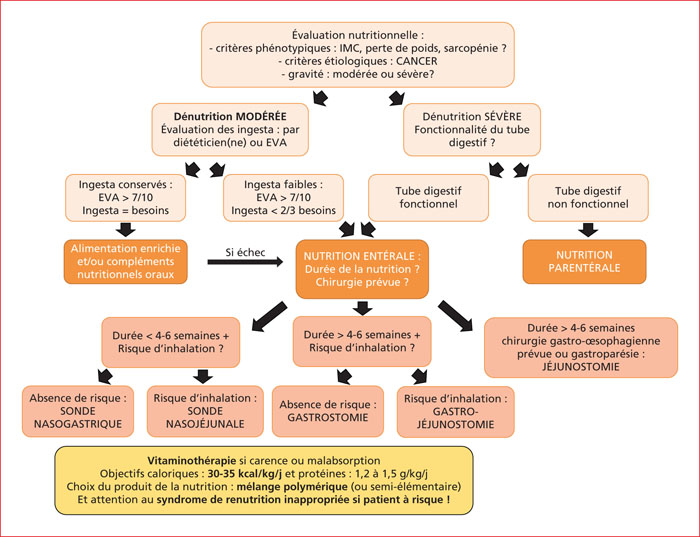
Protein-energy malnutrition, is estimated between 35 and 67% depending on digestive tumor locations, significantly worsens the morbidity and mortality. Nutritional status should be assessed regularly during hospitalization and at each visit. If the diagnosis of undernutrition is retained according to HAS criteria, adapted and personalized nutritional support is essential for an optimal oncological management. The nutritional prescription is often approximate. The evaluation of ingesta, by a dietician or a visual analogical scale, is a necessary prerequisite. Thus, in case of moderate undernutrition with a low intake or in case of severe undernutrition with a functional digestive tract, enteral nutrition appears as the optimal support. This enteral nutrition can be administered through a nasogastric tube, gastrostomy or even jejunostomy depending on the duration of nutrition, the need for upper gastrointestinal surgery or gastroparesis. Nutritional intake, with a standard solution as first line, must be done with caution if the patient is at risk of refeeding syndrome until a target of 30 to 35 kcal/kg/d is reached with 1.2 to 1.5 g/kg/d of protein. Nutrition should be re-evaluated regularly and continued until the nutritional goals set with the patient are achieved.