Hépato-Gastro & Oncologie Digestive
MENUAnal incontinence, how to treat? Volume 27, issue 3, Mars 2020
Figures
Tables
- Key words: anal incontinence, pelvic floor rehabilitation, biofeedback, ventral rectopexy, sphincter repair, sacral nerve modulation
- DOI : 10.1684/hpg.2020.1937
- Page(s) : 308-19
- Published in: 2020
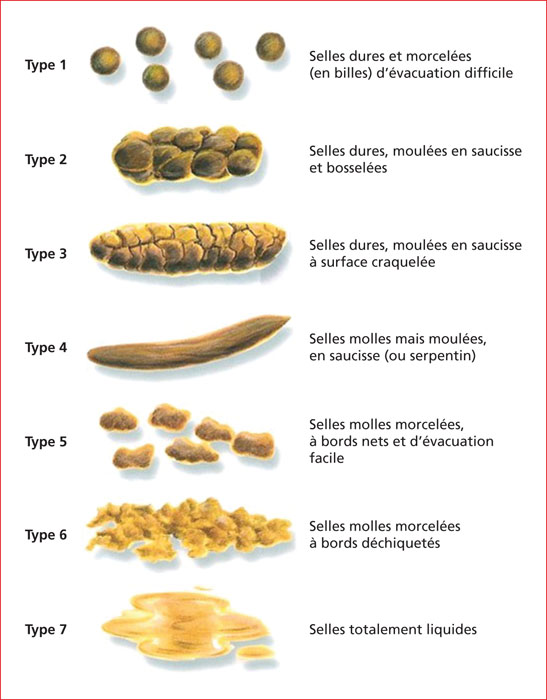
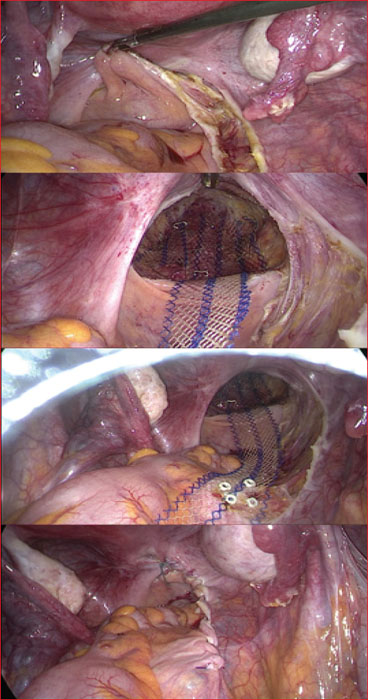
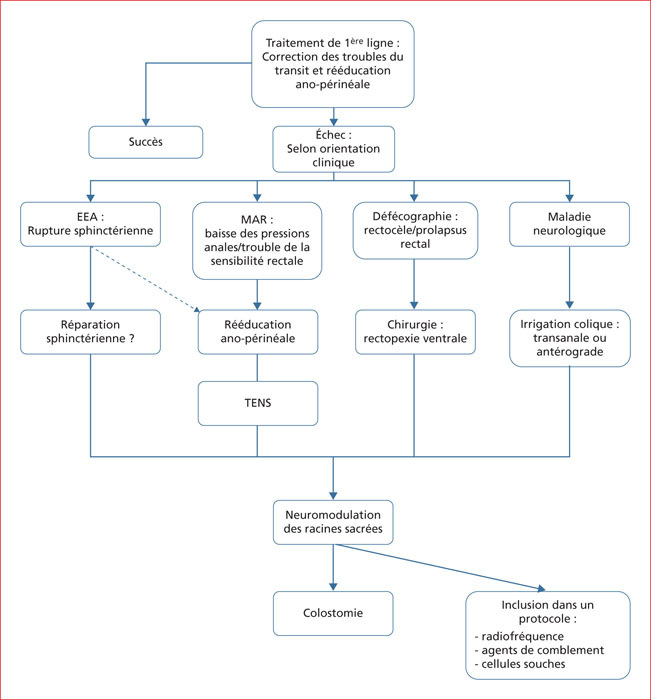
Anal incontinence (IA) is a public health issue because of its high prevalence, between 5 and 17% according to the definition of incontinence, the significant impact on the quality of life and the high economic cost of treatments. Transit disorders are major risk factors for AI whose etiology is most often multifactorial. The management of AI must be global and multidisciplinary. It is based primarily on the regulation of transit and stool consistency and perineal rehabilitation. In case of failure of first line treatment, further explorations will be requested to guide second line treatment. Second-line treatment is mainly based on the surgical correction of a rectal static disorder, sphincter repair in case of external anal sphincter injury and more rarely on colonic irrigation techniques. Sphincter repair is limited to high-grade perineal tears after childbirth. It tends to be replaced by sacral nerve stimulation, which has revolutionized the management of patients with severe AI. There are various indications for sacral nerve modulation. However, it is estimated that only 1 out of 2 patients eligible for treatment benefits in the long term. Now, question is how to treat patients who failed, for whom currently the last hope is colostomy. Other treatments are under study. It is mainly anal radiofrequency, bulking agents and autologous stem cells. The first positive results must be confirmed before being able to recommend these treatments.