Hépato-Gastro & Oncologie Digestive
MENURadiation proctitis Volume 22, issue 6, Juin 2015
Institut Léopold Bellan,
service de proctologie médico-chirurgicale,
185, rue Raymond Losserand,
75014 Paris, France
service de chirurgie digestive,
185, rue Raymond Losserand,
75014 Paris, France
- Key words: radiation proctitis, chronic hemorrhagic radiation proctitis, topical formalin, argon plasma coagulation, hyperbaric oxygen therapy
- DOI : 10.1684/hpg.2015.1164
- Page(s) : 488-99
- Published in: 2015
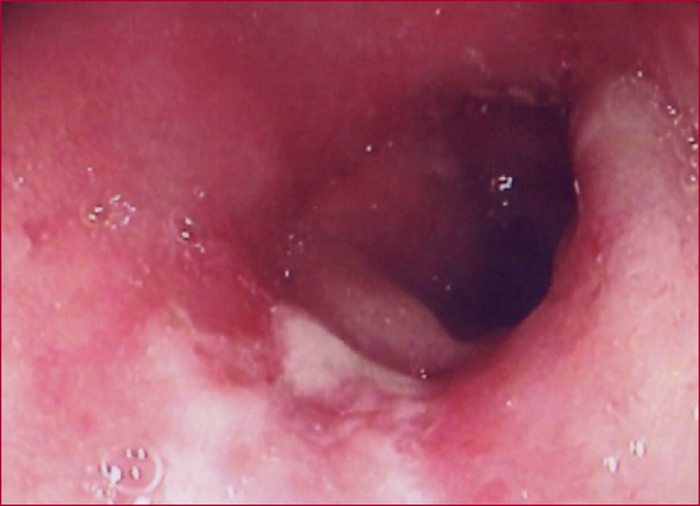
When selecting the best therapeutic strategy for radiation proctitis, several observations should be kept in mind: their natural history is poorly known, individual predictive factors of chronic manifestations (severe bleeding, fecal incontinence) have not been identified, available treatments (argon plasma, formalin) can induce adverse events and all surgical procedures (including fecal diversion) have their own morbidity and mortality rates. In the case of rectal bleeding, a colonoscopy is required to detect associated radiation-induced hemorrhagic lesions that will balance the importance of rectal bleeding, and other upstream colonic lesions. Mild to moderate rectal bleeding can be treated with sucralfate enemas. For severe rectal bleeding, argon plasma coagulation is the preferred option given an efficacy similar to that of formalin application and a slightly lower complication rate. Formalin is particularly effective for the treatment of diffuse and severe hemorrhagic proctitis, especially of distal location. In case argon plasma coagulation and/or formalin application fail to improve clinical symptoms, hyperbaric oxygen therapy has a demonstrated efficacy (Evidence Based Medicine). Hyperbaric oxygen therapy is also useful for the treatment of severe hemorrhagic combinations of proctitis and cystitis, in the case of severe and late anorectal and bladder functional disorders. The prevention of radiation proctitis depends on optimization of radiotherapy parameters.