Hépato-Gastro & Oncologie Digestive
MENUColorectal serrated lesions: what does this mean for the pathologist, gastroenterologist and patient? Volume 22, issue 9, Novembre 2015
Hôpital Saint-Antoine,
Faculté de Médecine Pierre et Marie Curie,
service d’anatomie et cytologie pathologiques,
184 rue du Faubourg Saint-Antoine,
75571 Paris cedex 12,
France
- Key words: serrated polyp, hyperplastic polyp, sessile serrated adenoma/polyp, traditional serrated adenoma, serrated polyposis
- DOI : 10.1684/hpg.2015.1216
- Page(s) : 803-11
- Published in: 2015
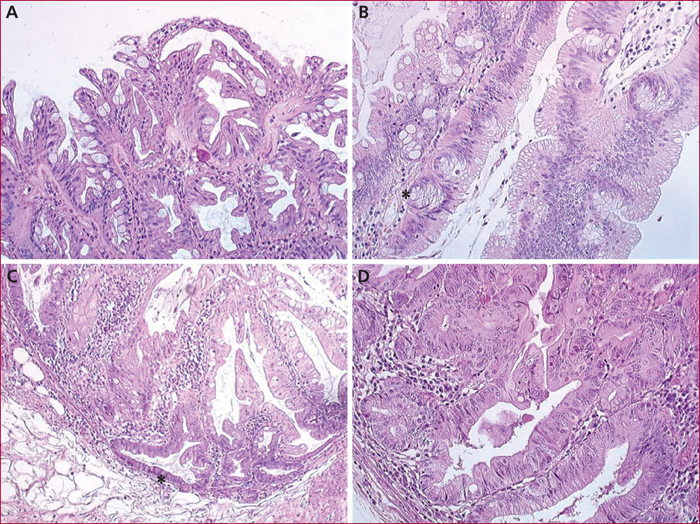
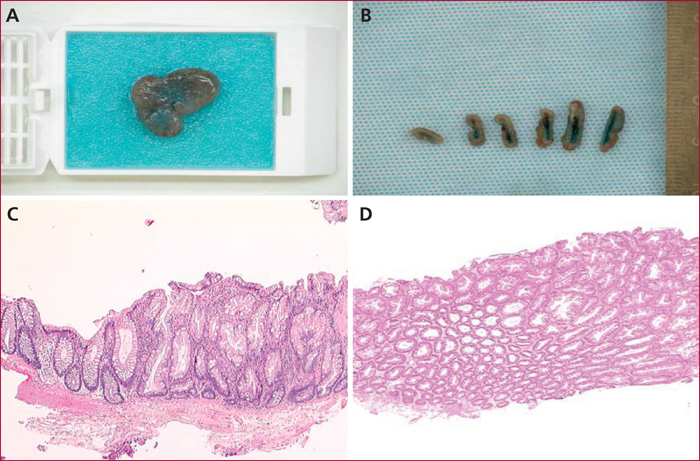
Approximately 30% of colorectal cancers (CRC) develop from serrated lesions. Serrated lesions constitute a heterogeneous group characterized, from a molecular point of view, by frequent BRAF mutation and a CIMP phenotype. The last WHO classification (2010) individualizes 3 types of serrated lesions: (i) hyperplastic polyp ; (ii) sessile serrated adenoma/polyp (SSA/P), with or without dysplasia; (iii) traditional serrated adenoma (TSA). The malignant potential of SSA/Ps and TSAs has been clearly demonstrated. These lesions, particularly SSA/P, are still underdiagnosed by pathologists, notably due to a lack of standardization and to the evolution of their diagnostic criteria. SSA/P, are more challenging to detect by colonoscopy and are likely to account for some interval carcinomas of the proximal colon. The current guidelines for the management of these lesions are close to those of “conventional” adenomas, despite a low level of evidence. A better understanding of serrated lesions from a clinical, pathological and molecular point of view will permit to better diagnose them and to better manage the patients.