Hépato-Gastro & Oncologie Digestive
MENUDysmetabolic cirrhosis: the next challenge for liver transplant teams? Volume 26, issue 3, Mars 2019
- Key words: liver transplantation, dysmetabolic cirrhosis, metabolic syndrome, obesity, survival, recurrence
- DOI : 10.1684/hpg.2019.1760
- Page(s) : 310-8
- Published in: 2019
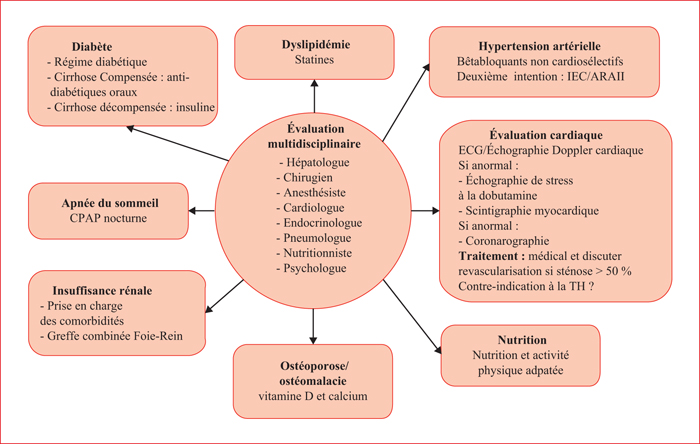
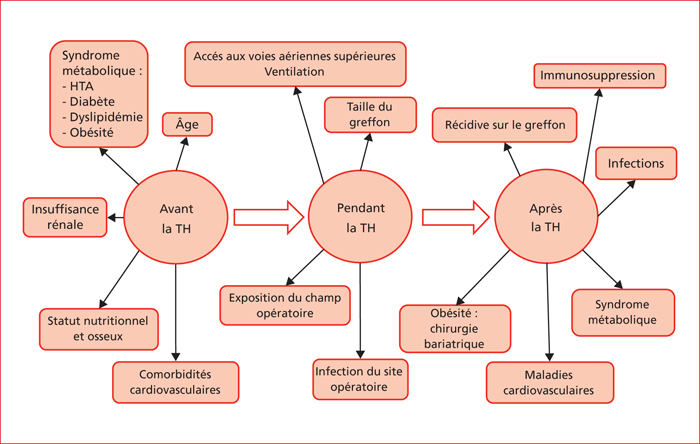
Liver steatosis is the hepatic manifestation of the metabolic syndrome, and is one of the leading causes of chronic liver disease. The treatment of dysmetabolic cirrhosis with liver failure and/or hepatocellular carcinoma is liver transplantation (LT). With an increase of 170% in 10 years, it is now the second indication of listing for LT in the United States. At listing, patients with dysmetabolic cirrhosis are older, with numerous cardiovascular (CV) and renal comorbidities, and this requires multidisciplinary pre-transplant assessment. After LT, 5-year survival is similar to other indications, despite an increased immediate CV mortality. The leading causes of death are infectious, cancers and CV. Obesity is an independent factor of increasing morbidity and mortality after LT. The recurrence of the initial disease is frequent: 30% to 90% of the patients present recurrent liver steatosis at 5 years, and 30% progress towards cirrhosis. No specific immunosuppressive regimen is recommended, but the toxicity profiles must probably be taken into account. In these patients, the only etiological treatment is that of obesity, in the absence of specific therapy for non-alcoholic steatohepatitis. The place of bariatric surgery has to be defined, probably sleeve gastrectomy, in a stable patient, 6 to 12 months after LT.
![]() This work is licensed under a
Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License
This work is licensed under a
Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License