Epileptic Disorders
MENUConvulsive syncope: a condition to be differentiated from epilepsy Volume 11, issue 4, December 2009
Auteur(s) : Cigdem Ozkara1, Baris Metin1, Serdar Kucukoglu2
1Department of Neurology, Cerrahpasa Medical
School
2Institute of Cardiology, University
of Istanbul, Turkey
Article reçu le 16 Juin 2009, accepté le 12 Octobre 2009
In clinical practice, the differential diagnosis between epilepsy and syncope is not always easy. Although the aetiologies of the two entities are completely different, their clinical presentation may be quite similar and even totally indistinguishable when based on clinical history taking. The term “convulsive syncope” was first used by Marcus Gerbezius (1658-1718) to describe a patient with “slow pulse, dizziness and slight epileptic attacks” (Acierno, 1994). This phenomenon was later described as a Stokes-Adams attack. In this report, we present a patient with unexplained episodes of loss of consciousness, elucidated only after video-EEG and cardiac evaluations.
Case study
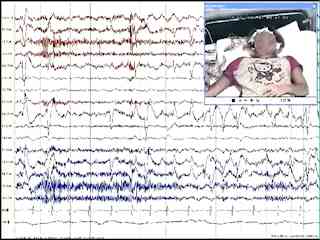
A 22-year-old young lady presented with episodes of loss of consciousness. The first episode occurred at the age of nine during blood drawing. The second episode was triggered by a sudden unexpected fall and subsequent episodes occurred as a reaction to a painful stimulus. The witnesses reported that the patient was staring without expression and irregular tonic postures and sometimes diffuse jerks occurred. The episodes were reported to last about 1-5 minutes and the patient always regained consciousness without confusion soon afterwards. The patient described a feeling of falling down before the episodes. Her routine EEG and cranial MRI were normal. Medical history was not significant. Her father and uncle experienced some episodes of fainting in reaction to seeing blood, although the family history was otherwise normal. She was admitted to our video-EEG unit to draw blood from her for another medical condition. The recorded parameters were 16 channel EEG (standard international electrodes), one channel ECG, EMG and simultaneous video recordings. During the procedure, we withdrew blood from the right antecubital fossa. Soon after the blood withdrawal was complete, she reported that she felt dizzy and heart rate began to slow down (figure 1). About 20 seconds later, complete asystole ensued and she lost her consciousness, with an expressionless stare. At first, her head and eyes turned to the right side with brief automatisms on the left arm, followed by head and eye deviation to the opposite side with an asymmetric dystonic posture of the upper extremities (figure 2). Hyperventilation and profuse sweating were observed. These dystonic postures subsided after about 40 seconds as the heart rhythm reappeared. After a silent period of 10 seconds, generalized irregular clonic jerks of the body were observed for 15 seconds. She finally began to snore and regained consciousness after a brief state of confusion. As she recovered, she cried and reported that she was feeling poorly.On EEG recordings, there was diffuse slowing when the heart rate began to slow down. When the patient lost her consciousness and heart beating stopped, diffuse generalized slow delta waves with high amplitude appeared, followed by complete suppression of cerebral activity. During 40 seconds of the asystolia period, head and eye deviation, brief automatisms and dystonic extremity movements were observed whereas the EEG was masked by muscle artefacts. After a silent period of 10 seconds (figure 3), body jerks started at the same time as diffuse high amplitude delta discharges on EEG. As these movements ceased, an irregular slow rhythm reappeared.
In the first part of the episode with bradycardia and asystolia, the clinical semiology was very much similar to an epileptic event with head/eye deviations, automatism and dystonic posture. In particular, the second phase of massive body jerks implied a convulsive episode, although this was induced by cerebral hypoxia with diffuse delta discharges without any epileptiform activity on EEG.
The patient was subsequently evaluated by the cardiology department and was re-admitted to be evaluated for cardiac parameters. The same procedure that caused the episode was reproduced. During the blood withdrawal, sinus bradycardia was followed by complete sinus arrest. In addition, the blood pressure dropped markedly but no convulsive movements were seen. According to these findings, she was diagnosed with sinus arrest mediated by vasovagal mechanisms.
Discussion
It is well known that cardiac diseases and syncope may strongly resemble seizures. The studies investigating the similarities between these conditions date back to the 1970s. It was reported that 20% of those referred to a neurology department with a possible diagnosis of epilepsy were subsequently considered to have cardiac arrhythmia as a cause of their symptoms (Schott et al., 1977).The characteristics of convulsive symptoms occurring during the syncopal episodes were investigated by several studies. In a study with blood donors, the prevalence of the convulsive syncope was found to be 0.03% (Lin et al., 1982). The authors reported that tonic extensor spasm was the most common convulsive movement and other complex phenomena also occurred simulating epileptic seizures. In another study, the videometric analysis of the episodes of the cerebral hypoxia was performed and the most commonly observed activity was myoclonus, occurring either as multifocal myoclonic jerks or generalized myoclonus. Additional motor activities observed in this report were: head turns, oral automatisms and righting movements (Lempert et al., 1994).
The cerebral electrical activity during the convulsive syncopes was also investigated. Background slowing evolving into loss of cerebral activity was reported in patients with malignant ventricular arrhythmias (Aminoff et al., 1988). Later studies also confirmed that the ictal patterns consisted of diffuse slowing without paroxysmal activity (Fernandez Sanmartin et al., 2003). Gelisse et al. (2007) conducted a video-EEG study of a 14-year-old boy misdiagnosed with epilepsy. They proved clinically and neurophysiologically that the patient actually experienced syncopal episodes. The video-EEG demonstrated a syncopal episode due to cardiac asystole triggered by ocular compression. During the episode, the EEG showed generalized slowing evolving into complete cessation of cerebral electrical activity.
In order to relieve diagnostic confusion, the utility of some diagnostic tests has been investigated. In one study, 24-hour electrocardiographic recordings were not found to be useful (Gibson and Heitzman, 1984). The authors reported that arrhythmia was a useful diagnostic symptom for only 2% of the patients and argued against the diagnostic utility of this method for syncope. Zaidi et al., (2000) investigated patients who were previously diagnosed with epilepsy and unresponsive to drug treatment. The patients were subjected to a head-up tilt test and carotis sinus massage during continuous electrocardiography, EEG and blood pressure recordings. For 41% of the patients, an alternative diagnosis other than epilepsy was given to explain their condition. The authors concluded that many patients with unexplained convulsive black-outs have a cardiovascular problem and suggested a non-invasive cardiovascular examination for such patients. Other studies suggest the tilt table test to be a reliable method to differentiate between epilepsy and syncope (Grubb et al., 1992; Sabri et al., 2006).
In agreement with previous reports, the observations of our patient demonstrate that cardiovascular diseases may impose a great diagnostic difficulty in the evaluation of the patients with presumed epilepsy. To overcome this, a diligent and elaborate investigation is needed. The interpretation of seizure semiology in such paroxysmal events may also be misleading and other parameters, such as ECG, should also be included during the recording and meticulously checked during the review. When there is a doubt, the neurologist should not hesitate to call for further cardiological investigation.
Legend for video sequence
Disclosure
None of the authors has any conflict of interest to disclose.This work was not supported by a grant or any other means and has not been presented anywhere before.