European Cytokine Network
MENUMetabolic link between obesity and autoimmune diseases Volume 32, issue 4, December 2021
- Key words: obesity, autoimmunity, immunometabolism, lymphocyte metabolism, cytokines
- DOI : 10.1684/ecn.2021.0474
- Page(s) : 64-72
- Published in: 2021
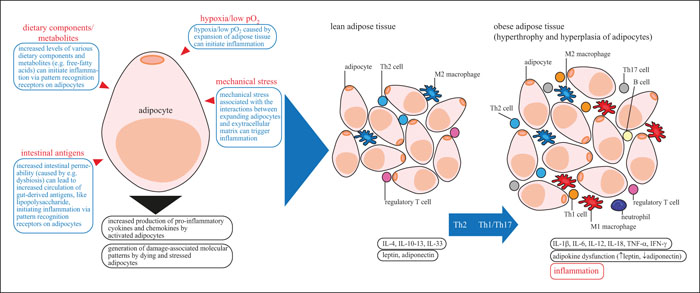
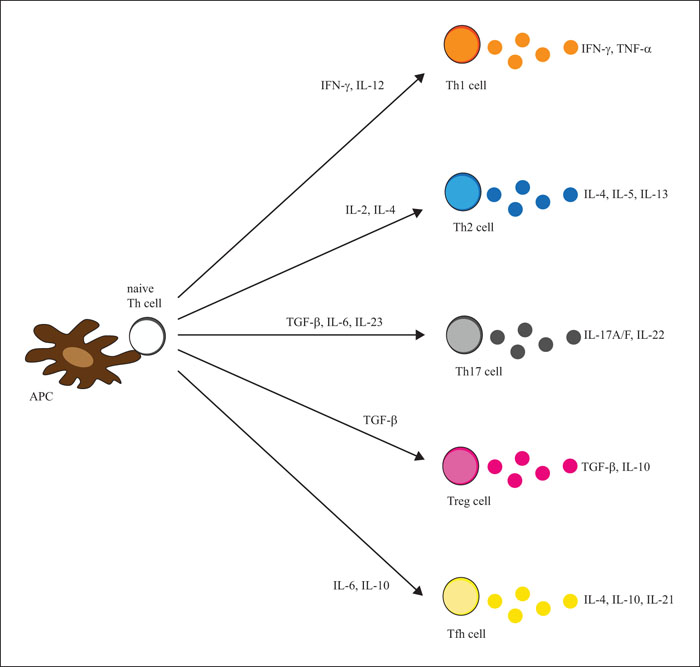
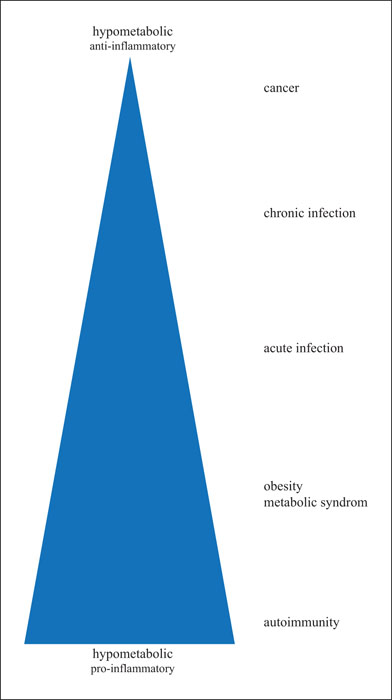
The abnormal accumulation of visceral adipose tissue in obesity is associated with metabolic changes that include altered glucose tolerance, insulin resistance, hyperlipidemia, and metabolic syndrome. Obesity also coincides with increased incidence of autoimmune diseases. Accumulating evidence suggest that prolonged metabolic overload related to overnutrition, influenced by genetic and epigenetic factors, might affect immunologic self-tolerance through changes in the energy metabolism of immune cells, particularly regulatory T (Treg) cells. A strong activation of nutrient-energy signaling pathways blocks the induction of the transcription factor forkhead P3 (FOXP3), a master regulator of Treg cells, consequently inhibiting their generation and proliferation, thereby promoting proinflammatory response. Expanding our knowledge on the topic, particularly on metabolic T cell flexibility in vivo will provide new insights that can be used to develop therapeutic strategies for various inflammatory diseases, including obesity and autoimmune diseases. Targeting specific metabolic pathways is emerging as an important approach to control immune response and maintain immunological homeostasis.