Hépato-Gastro & Oncologie Digestive
MENUIBD and obesity: the vicious cycle Volume 31, issue 1, January 2024
- Key words: obesity, IBD, biotherapy, surgery, nutrition
- DOI : 10.1684/hpg.2023.2697
- Page(s) : 33-42
- Published in: 2024
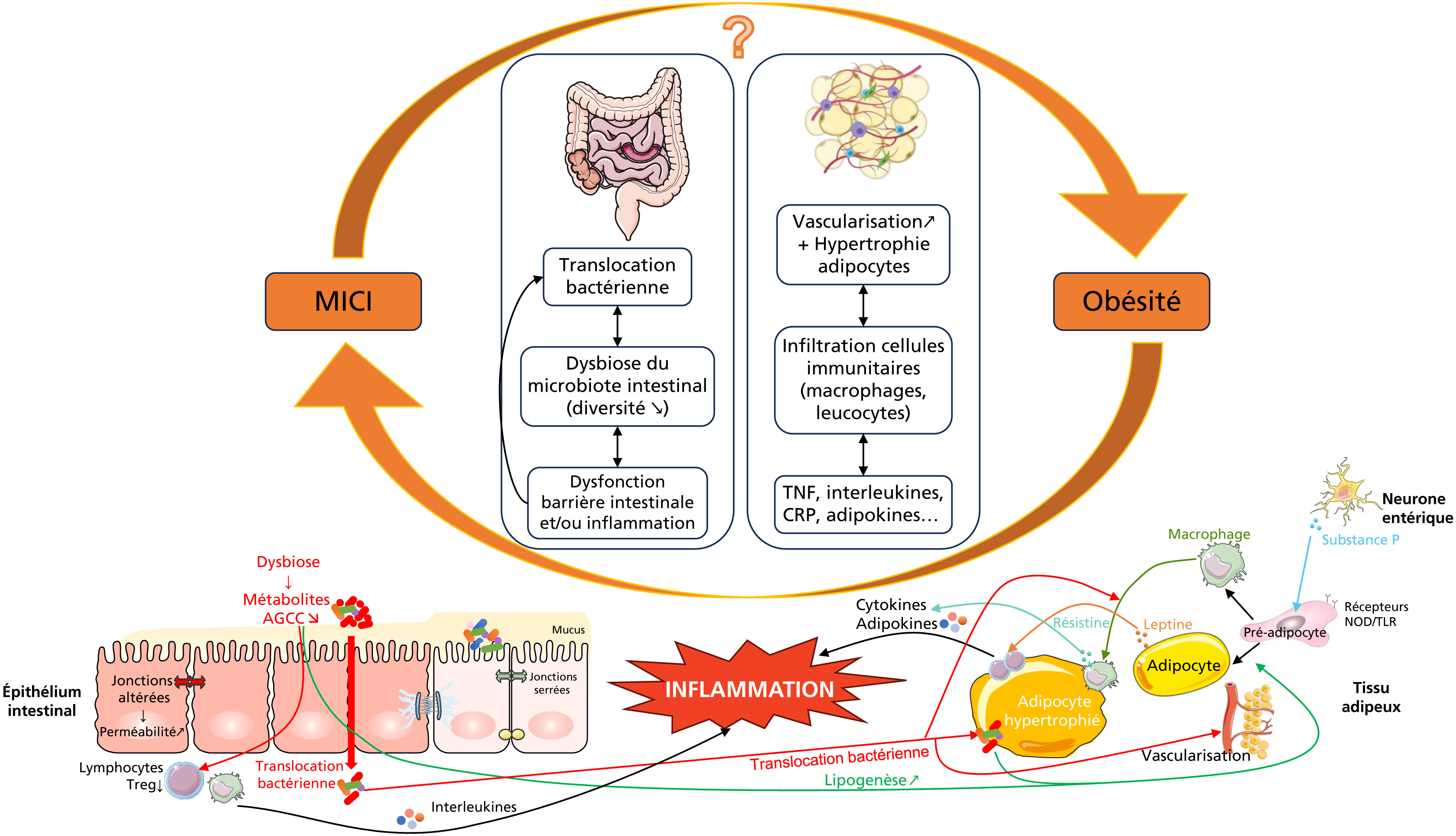
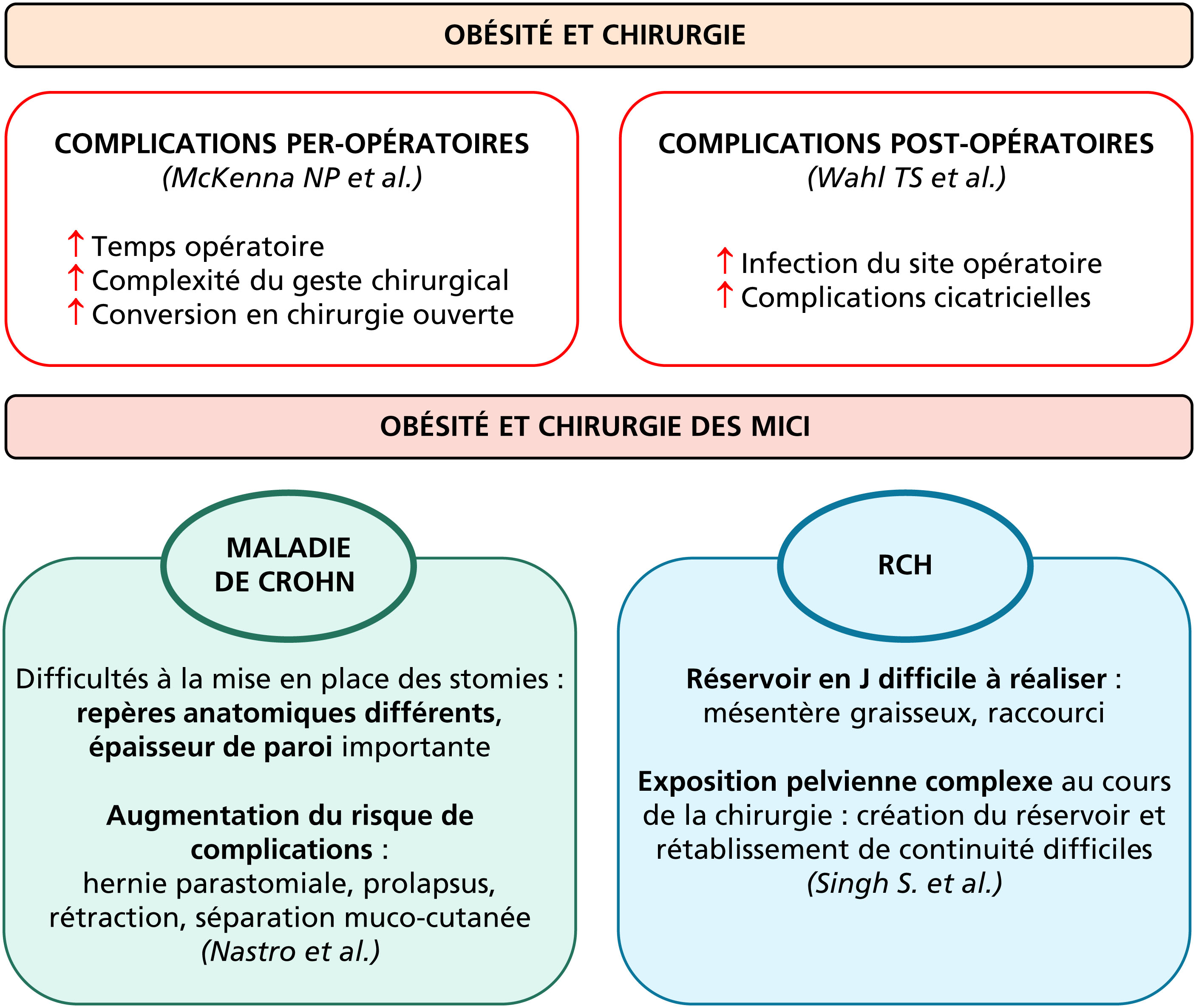
The growing proportion of patients with IBD and obesity (15 to 40%) makes their management a critical therapeutic challenge. Obesity has a negative impact on the natural course of the disease, leads to an attenuated response to biotherapies and favors surgical complications. A nutritional assessment is therefore essential, and physicians should be aware of screening patients for malnutrition (even in the presence of obesity), sarcopenia and obesity-related complications. A multidisciplinary approach must be proposed to the patients: supervised changes in eating habits to avoid causing or worsen deficiencies, especially during inflammatory flare-ups, as well as practicing regular physical activity. Drug treatments for obesity, particularly GLP-1 analogs, can be proposed, although their impact on the evolution of inflammatory bowel disease has yet to be demonstrated. Bariatric surgery, when indicated, should be proposed to patients, as it has a demonstrated benefit on post-operative evolution in IBD.