Hépato-Gastro & Oncologie Digestive
MENUDiagnosis, causes and prognosis of acute renal failure during cirrhosis Volume 26, issue 2, Février 2019
- Key words: acute renal failure, acute tubular necrosis, hepatorenal syndrome
- DOI : 10.1684/hpg.2019.1738
- Page(s) : 192-9
- Published in: 2019
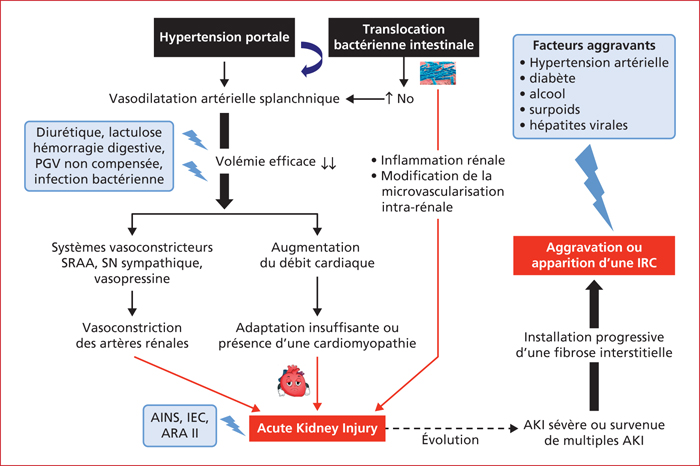
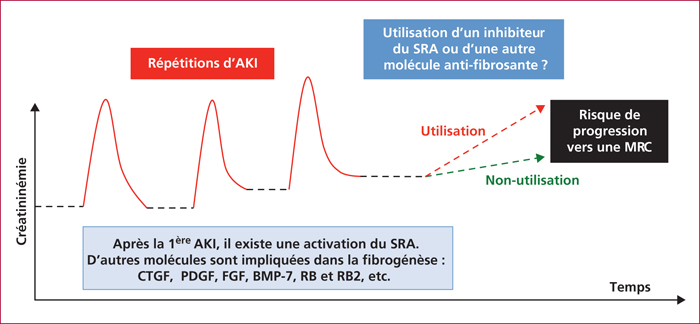
Acute renal failure, recently renamed acute kidney injury (AKI), occurs frequently in cirrhosis. The susceptibility to AKI is due to both severe splanchnic arterial vasodilatation and systemic inflammation. The presence of a cardiomyopathy associated with cirrhosis may contribute to the renal hypoperfusion. The main causes of AKI include prerenal azotemia, acute tubular necrosis (ATN), and hepatorenal syndrome (HRS). AKI is usually triggered by an acute event, such as excess circulatory volume loss from large doses of diuretics or lactulose, gastrointestinal bleeding, large volume paracentesis without volume replacement with albumin, and bacterial infection. AKI criteria are now defined as either an absolute increase in serum creatinine ≥ 26.4 μmol/L in less than 48 h, or by a percentage increase ≥50% in less than seven days. Based on a staging of AKI, a new algorithm has been proposed for a prompt management of these patients. Prognosis differs also according to AKI etiology; patients with HRS-AKI or ATN have a worse prognosis than those with prerenal azotemia. The severity, frequency and duration of AKI have been recognized to favor occurrence of ensuing chronic renal failure. Preventing the development of AKI and early treating AKI are therefore a priority for hepatologists.
![]() This work is licensed under a
Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License
This work is licensed under a
Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License