Epileptic Disorders
MENUEpileptic ictal strabismus: a case report and review of the literature Volume 20, issue 4, August 2018
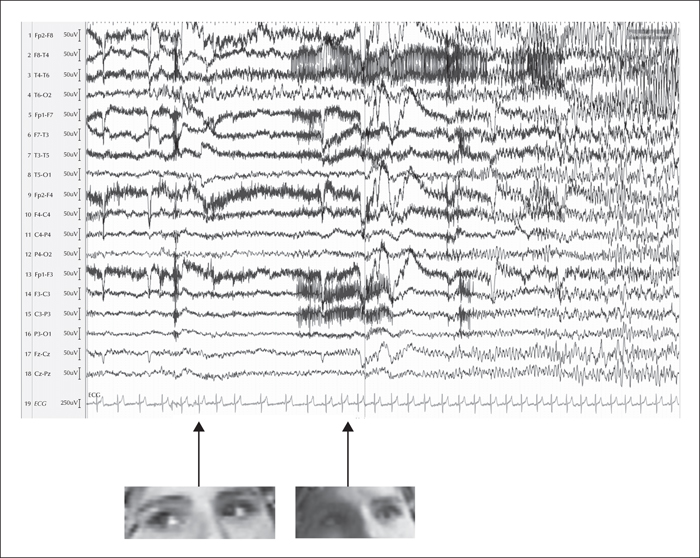
Figure 1
At seizure onset (left arrow), the patient has a rightward horizontal conjugate eye deviation; the EEG shows rhythmic theta activity over the right posterior temporal region and rhythmic epileptic activity from the right temporal to right fronto-central regions, concomitant with the appearance of convergent strabismus due to adduction of the right eye without conjugate left eye abduction (right arrow). The patient's blinking (see blink artefact over frontal regions indicated by the right arrow) could be a semiconscious reaction to the sudden onset of diplopia due to ictal strabismus (when questioned postictally, the patient did not recall any symptom of double vision occurring immediately before loss of consciousness). Ictal tachycardia starts just after the blink. Sensitivity: 7 μV; LF: 0.53 Hz; HF: 70 Hz; speed: 30 sec/page.
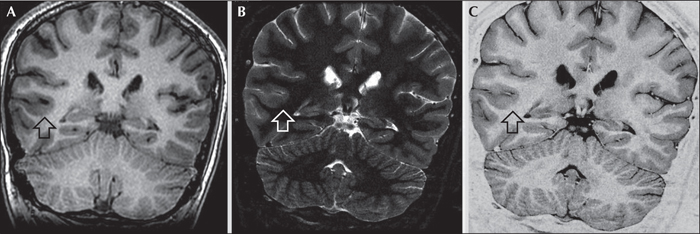
Figure 2
(A) Coronal T1-weighted peri-ictal MRI multiplanar (MPR) reconstruction, (B) coronal thin-slice inversion recovery (IR), and (C) coronal thin-slice FSE T2 image of the patient whose previous MRI had been considered normal. Note the focal area of slightly thickened cortex and blurred cortical-subcortical junction in the posterior section of the right temporal lobe; 1-mm thin sections are suggestive of cortical dysplasia.
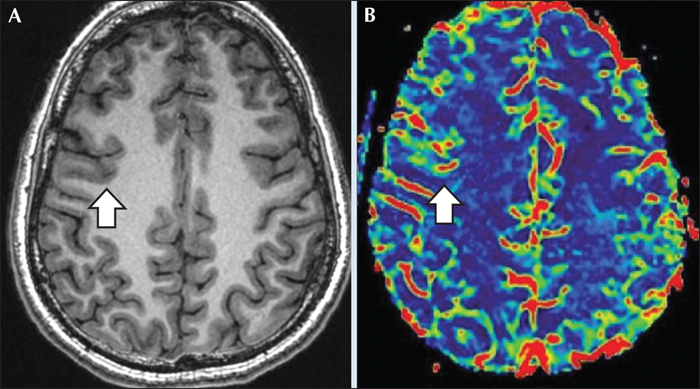
Figure 3
(A) Peri-ictal axial T1-weighted MRI multiplanar (MPR) reconstruction, and (B) axial DSC PWI image. Perfusion-weighted imaging clearly shows focal cortical-subcortical cerebral blood flow increase in the right frontal eye field area, correlating with the ictal epileptic activity.

