Néphrologie & Thérapeutique
MENUCarfilzomib-induced haemolytic and uremic syndrome: Favorable outcome with eculizumab Volume 16, issue 4, Juillet 2020
Figures
- Key words: Carfilzomib, Eculizumab, Hemolytic-uremic syndrome, Proteasome inhibitors, Thrombotic microangiopathy
- DOI : 10.1016/j.nephro.2020.03.006
- Page(s) : 221-4
- Published in: 2020
Self-care education can play an important role in improving the quality of life in hemodialysis patients.
The purpose of this study was to determine the effect of self-care education with teach back method on the quality of life in hemodialysis patients.
In this pre- and post-test clinical trial, 45 patients with end-stage renal disease undergoing hemodialysis at Sina hospital in Tehran were included. Patient education was done with teach back method. The duration of training were 3 sessions and the time of each session lasted from 45 minutes to one hour. To collect data from patients, a demographic questionnaire was used and to assess the quality of life of patients, kidney disease quality of life-short form before and after education was used. A significant level of 5% was determined.
The mean age of patients was 58.49±9.97 years. Among the dimensions of quality of life before education, the highest score was for physical role (64.24±7.68) and the lowest was related to job status (28.33±11.06). After training, the most score was related to emotional role (71.15±2.84) and the least was related to job status (43.87±11.54). A significant difference between the quality of life at before and after education was seen (P=0.000).
This study showed that self-care education through teach back method improves the quality of life in hemodialysis patients. Therefore, it is recommended that nurses in the hemodialysis unit implement self-care education through teach back method as an important task.
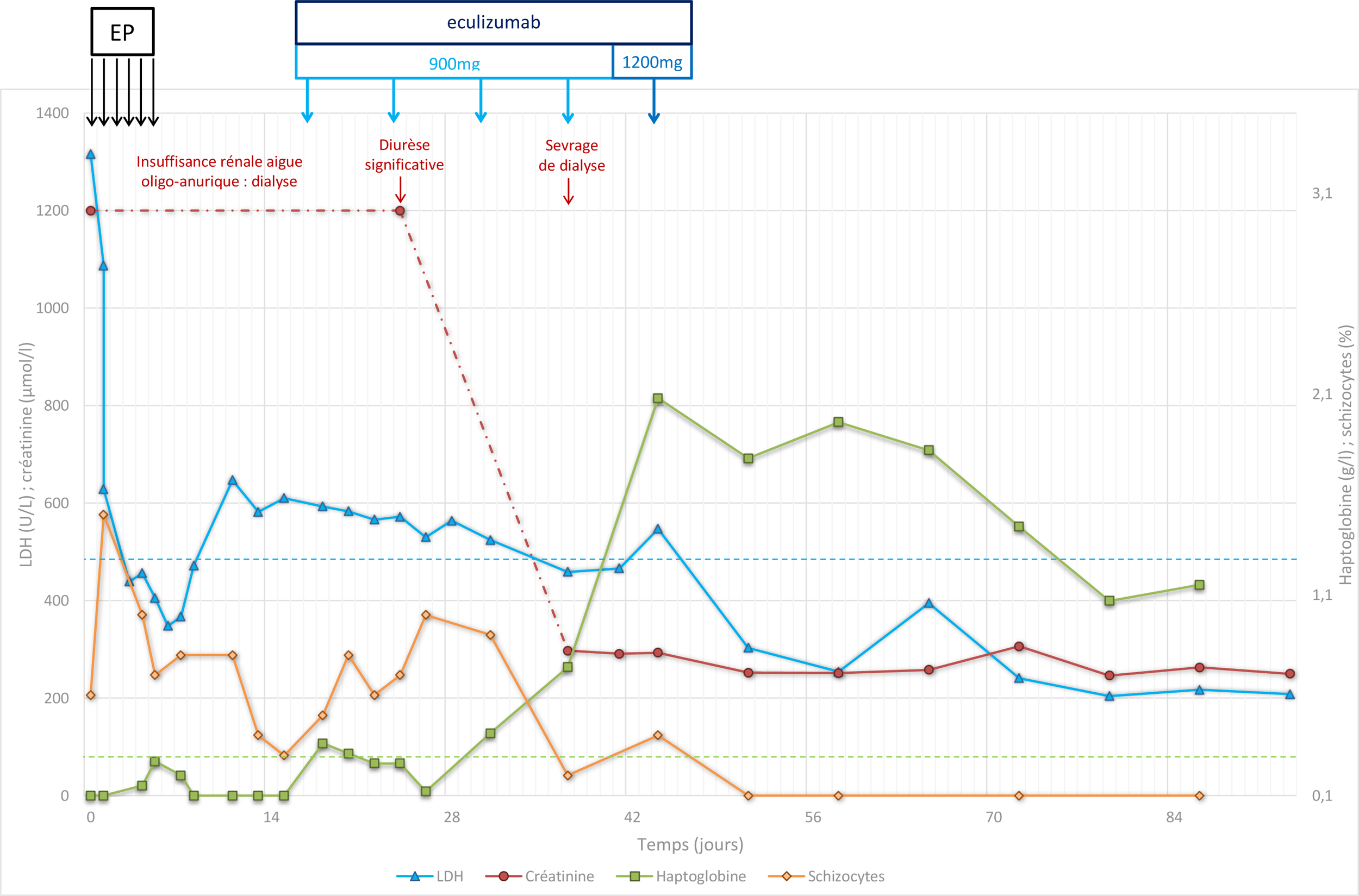
Les microangiopathies thrombotiques sont des pathologies rares, caractérisées par une lésion endothéliale initiale et la formation de thrombi dans la microcirculation. On distingue le purpura thrombotique thrombocytopénique, le syndrome hémolytique et urémique, notamment le syndrome hémolytique et urémique « typique » dû à une infection à Escherichia coli producteur de shiga toxine, ou le syndrome hémolytique et urémique atypique dû à un défaut de régulation de la voie alterne du complément, et les microangiopathies thrombotiques « secondaires ». Les médicaments constituent une cause fréquente de cette catégorie de microangiopathie thrombotique, dont la prise en charge passe essentiellement par l’arrêt du médicament incriminé. Nous rapportons le cas d’un patient ayant développé un syndrome hémolytique et urémique « secondaire » lié au carfilzomib, médicament inhibiteur du protéasome, dans le cadre du traitement d’un myélome multiple. À distance de l’arrêt du médicament, le patient gardait des signes d’hémolyse et une insuffisance rénale anurique nécessitant un traitement par hémodialyse. Nous avons alors introduit un traitement par éculizumab. L’évolution a finalement été favorable avec négativation du bilan d’hémolyse et amélioration de la fonction rénale permettant le sevrage de la dialyse. Nous discutons les mécanismes susceptibles d’activer la voie alterne du complément et l’intérêt potentiel d’une utilisation, même transitoire, de l’éculizumab dans ces cas de syndrome hémolytique et urémique liés aux inhibiteurs du protéasome, notamment au carfilzomib.
Thrombotic microangiopathies are rare diseases characterized by an initial endothelial injury and the formation of thrombi in the microcirculation. Several types of thrombotic microangiopathies can be distinguished: the thrombotic thrombocytopenic purpura; the hemolytic and uremic syndrome, mainly “typical” following a shiga toxin-producing Escherichia coli infection or “atypical” due to a dysregulation of the alternative complement pathway; and “secondary” thrombotic microangiopathies. The use of drug treatments is reported as a frequent cause in this last category and requires stopping the offending drug. We report the case of a patient who developed “secondary” hemolytic and uremic syndrome associated with carfilzomib, a proteasome inhibitor which is used in case of multiple myeloma relapses. Besides stopping the treatment, the patient still showed signs of hemolysis and renal failure with anuria requiring hemodialysis. An eculizumab treatment was therefore initiated. The overall evolution was favorable and an improvement of the renal function promptly allowed the discontinuation of hemodialysis. We discuss the mechanisms that may activate the alternative complement pathway and the potential interest of a transient use of eculizumab in case of carfilzomib-induced hemolytic and uremic syndrome.