Néphrologie & Thérapeutique
MENUPerspectives for future development of the kidney paired donation programme in France Volume 18, issue 4, Juillet 2022
- Key words: Bioethics law, Kidney exchange programme, Kidney paired donation, Living donor chain, Living donor kidney transplantation
- DOI : 10.1016/j.nephro.2022.02.001
- Page(s) : 270-7
- Published in: 2022
Nutrition in hemodialysis patients is important in decreasing complications, improving quality of life, and preventing of malnutrition. Recommendations of the guidelines are taken into consideration while prescribing a nutrition therapy plan for patients. However, the recommendations may differ between the guidelines. It was aimed to compare the newly published National Kidney Foundation Kidney Disease Outcomes Quality Initiative (NKF KDOQI) guideline with previous reported two guideline recommendations and protein energy wasting criteria in this study.
Fifty-five maintenance hemodialysis patients between the ages of 18–65 were included in the study. Daily energy intake and daily protein intake of these patients were evaluated by three different nutrition guidelines; NKF KDOQI-2000, 2020 and European Best Practice Guidelines-2007. In addition, protein energy wasting was determined by using anthropometric measurements, biochemical findings and food intake of the patients.
When the inadequacy rate in dietary daily energy intake and daily protein intake of the patients evaluated by NKF KDOQI-2000 recommendations, it was found to be higher than the rates in other two recommendations (P<0.05). Based on criteria, protein energy wasting was detected in 29.1% of the patients. While the NKF KDOQI-2020 daily energy intake recommendation was not consistent with other guideline recommendations, it seems highly compatible with protein energy wasting recommendations such as albumin, body mass index, mid-upper arm circumference, energy, and protein intake. While NKF KDOQI-2020 daily protein intake recommendation complies with European Best Practice Guidelines-2007 recommendations, the level of agreement with protein energy wasting criteria is very low.
Inadequate protein intake is still an ongoing problem in hemodialysis patients. NKF KDOQI-2020 guidelines provide a more suitable and applicable daily energy intake recommendation for patients compared to the previous guidelines.
Chronic kidney disease is a chronic non-transmittable disease of increasing incidence. The advanced stages are complicated by high morbidity and mortality, and individual management is complex due to the various treatments required at stage 5 including renal replacement. For the healthcare system, this disease also requires complex care organization. National registers of patients on renal replacement therapy have been developed to improve patient management and care arrangements. The purpose of our review was to report on the history of the French registry, its organization, the information collected and its evolution in response to the stage 5 problem. We successively detail the information system with its inclusion criteria, architecture and tools developed, its security rules, mode and type of information collected, its quality controls and, finally, the glossary of data available within the registry.
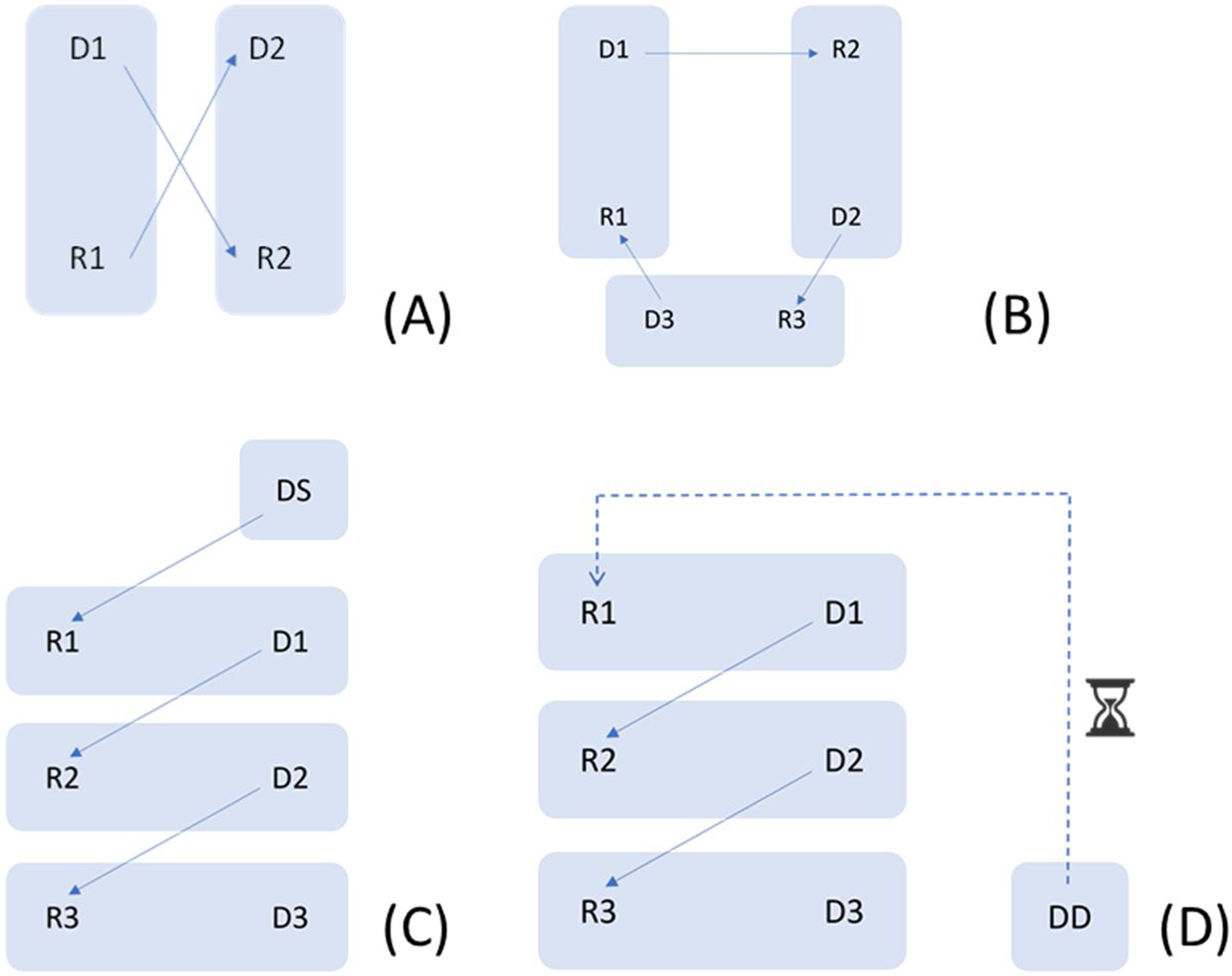
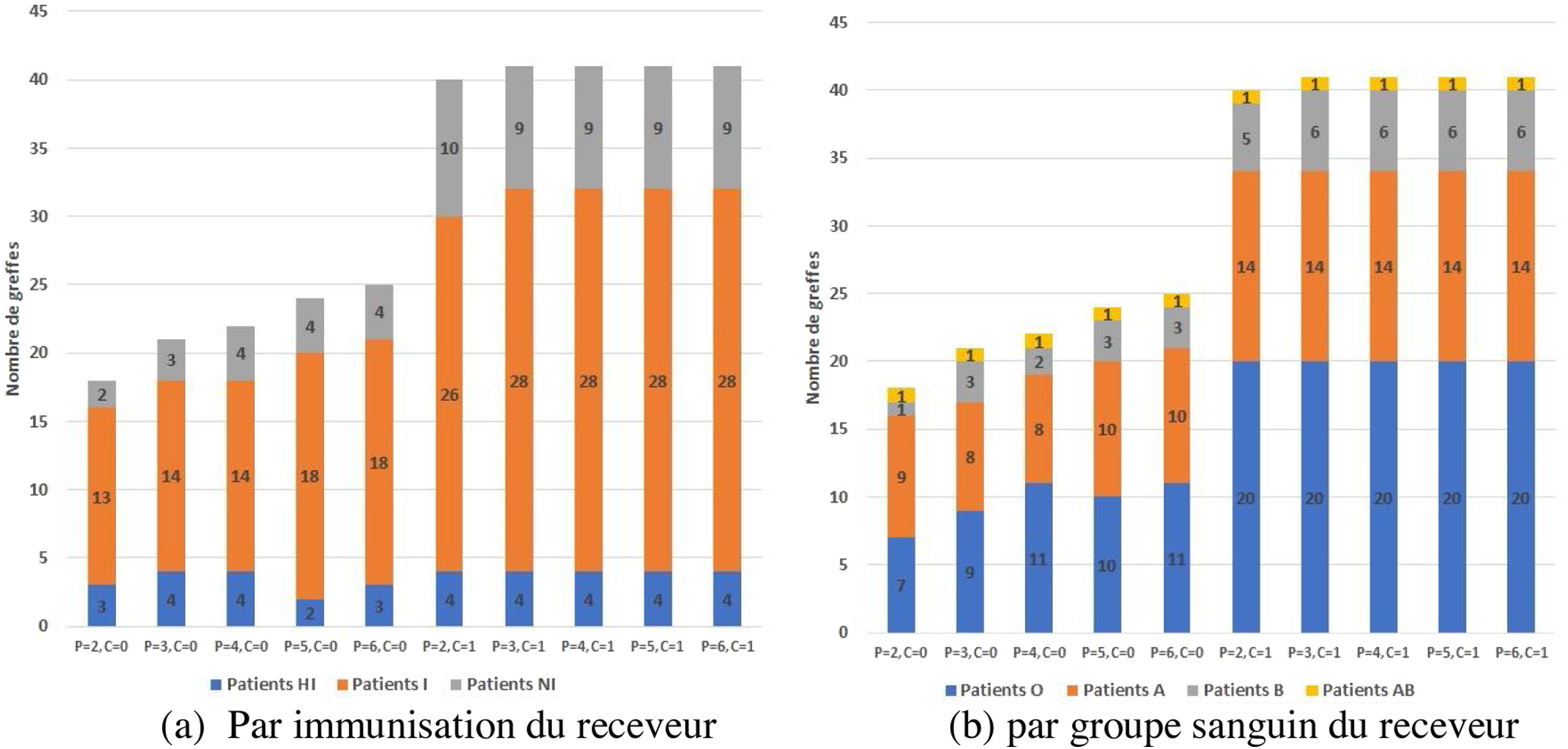
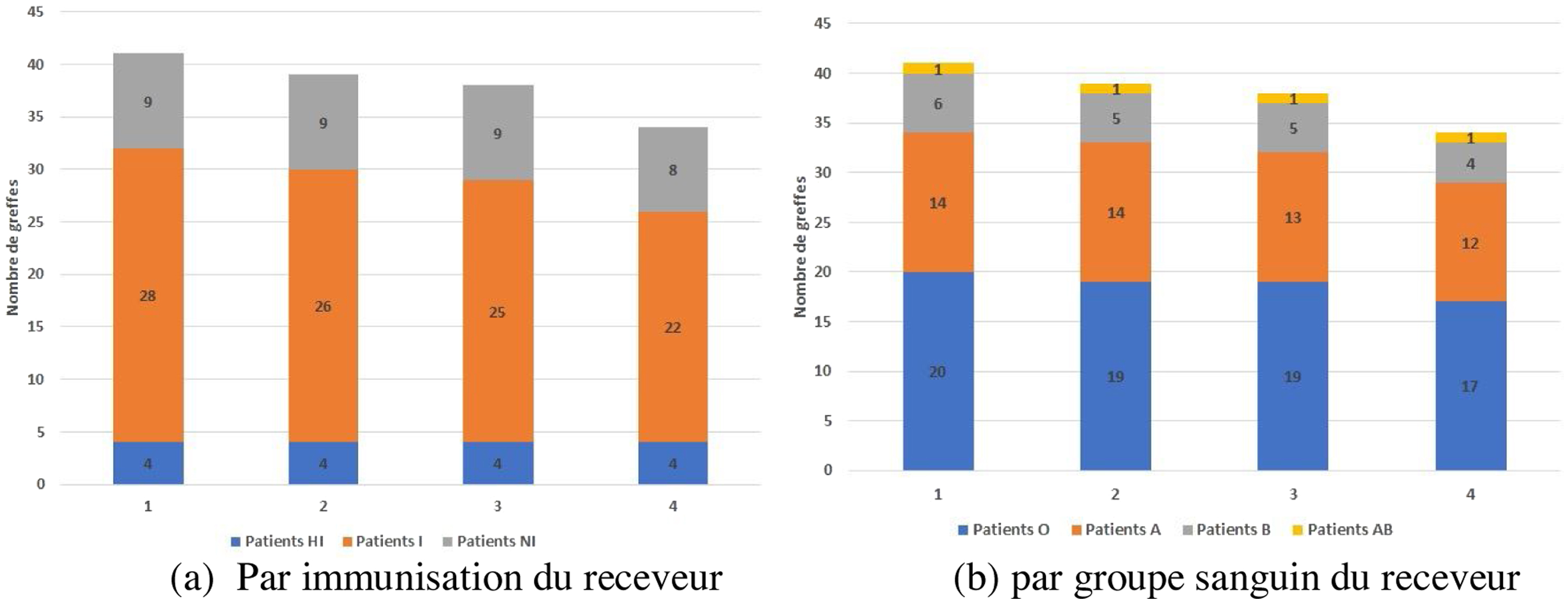
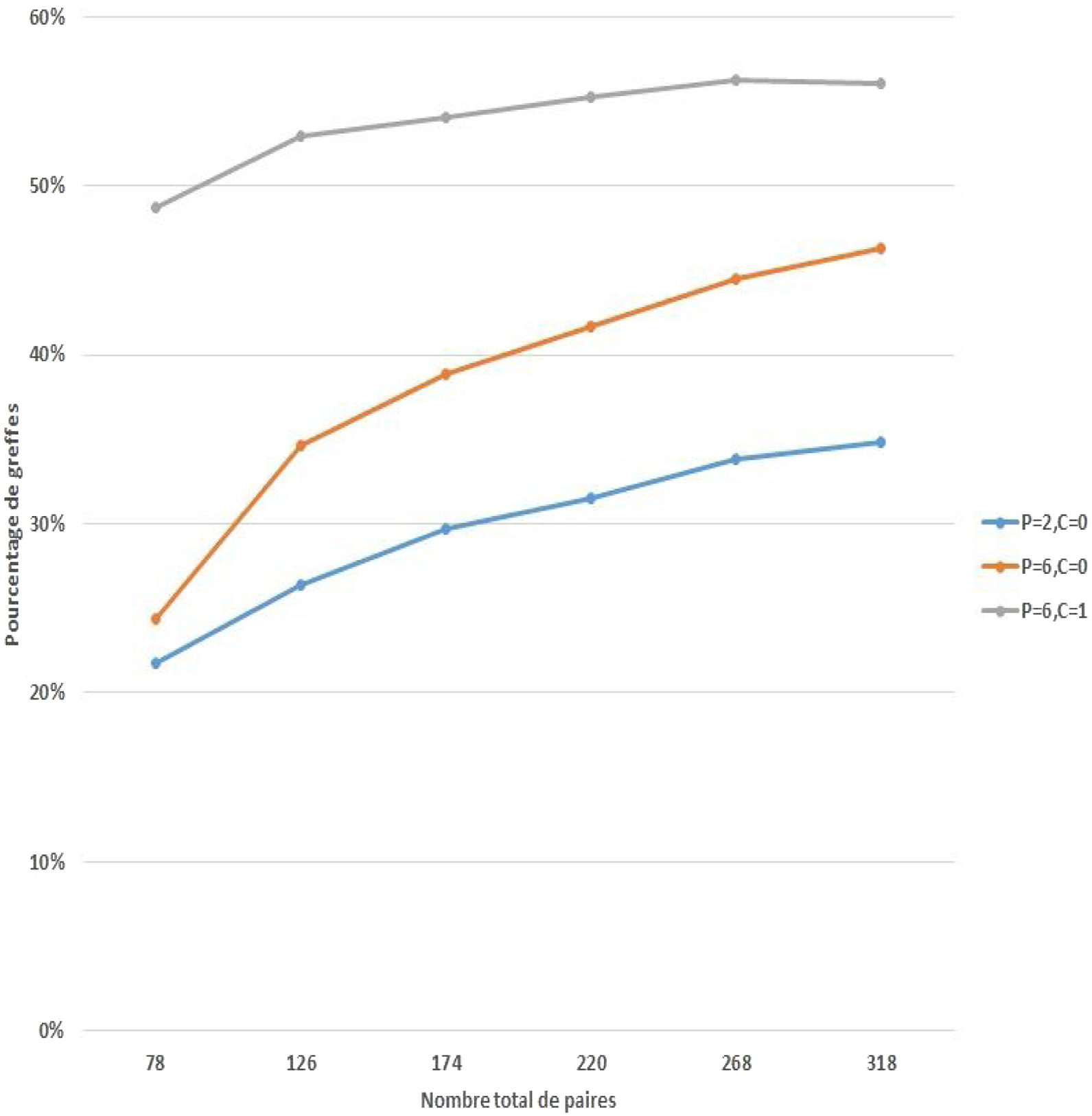
Près d’un tiers des candidats au don de rein présente une incompatibilité (HLA et/ou ABO) avec le receveur pour lequel il s’engage. Le don croisé permet d’échanger des donneurs potentiels et donne l’accès à une greffe rénale compatible. La loi de bioéthique de 2011 a autorisé le don croisé en France avec une réciprocité entre 2 paires « donneur-receveur » incompatibles. Un faible nombre de greffes a été réalisé du fait d’une autorisation trop limitée en comparaison à d’autres pratiques européennes. Cette étude présente les perspectives de la nouvelle loi de bioéthique, promulguée en 2021, qui élargit les pratiques autorisées pour le don croisé en France. Les deux évolutions simulées sont l’augmentation du nombre de paires engagées dans un échange croisé à 6 (contre 2 paires actuellement) et le recours à un donneur décédé en substitution à l’un des donneurs vivants. Différents scénarii sont simulés à partir des données de l’Agence de la biomédecine ; les paires incompatibles inscrites dans le programme de don croisé en France entre décembre 2013 et février 2018 (78 paires incompatibles), les greffes incompatibles réalisées au cours de la même période (476 paires incompatibles) et les caractéristiques des donneurs décédés ainsi que les propositions faites sur cette période. L’augmentation du nombre de paires a un effet limité sur le nombre de greffes, qui passe de 18 (23 % des receveurs) dans le système actuel à 25 (32 % des receveurs) lorsque 6 paires peuvent être engagées dans un échange croisé. Le recours à un donneur décédé augmente significativement le nombre de greffes, qui passe à 41 (52 % des receveurs). Cette étude permet d’évaluer l’augmentation des possibilités de greffes rénales par don croisé suite à la nouvelle loi de bioéthique. Un groupe de travail et une campagne d’information des professionnels et des patients seront nécessaires pour sa mise en œuvre, dont les résultats seront d’autant plus importants que la participation sera élevée.
Almost one third of kidney donation candidates are incompatible (HLA and/or ABO) with their directed recipient. Kidney paired donation allows potential donors to be exchanged and gives access to a compatible kidney transplant. The Bioethics Law of 2011 authorised kidney paired donation in France with reciprocity between 2 incompatible “donor-recipient” pairs. A limited number of transplants have been performed due to a too restricted authorization compared to other European practices. This study presents the perspectives of the new Bioethics Law, enacted in 2021, which increases the authorised practices for kidney paired donation in France. The two simulated evolutions are the increase of the number of pairs involved in a kidney paired donation to 6 (against 2 currently) and the use of a deceased donor as a substitution to one of living donor. Different scenarios are simulated using data from the Agence de la Biomedecine; incompatible pairs registered in the kidney paired donation programme in France between December 2013 and February 2018 (78 incompatible pairs), incompatible transplants performed during the same period (476 incompatible pairs) and characteristics of deceased donors as well as proposals made over this period. Increasing the number of pairs has a limited effect on the number of transplants, which increases from 18 (23% of recipients) in the current system to 25 (32% of recipients) when 6 pairs can be involved. The use of a deceased donor significantly increases the number of transplants to 41 (52% of recipients). This study makes it possible to evaluate the increase in possibilities of kidney transplants by kidney paired donation following the new bioethics law. A working group and an information campaign for professionals and patients will be necessary for its implementation.