Néphrologie & Thérapeutique
MENUBilateral renal infarction after discontinuation of anticoagulant therapy Volume 12, issue 4, Juillet 2016
- Key words: Anticoagulant therapy, Renal infarction
- DOI : 10.1016/j.nephro.2016.01.014
- Page(s) : 234-6
- Published in: 2016
Peritoneal dialysis (PD) is often avoided for patients with polycystic kidney disease (PKD) because of increased risk of complications and technique failure due to limited intra-abdominal space. In this study, we have aimed to determine clinical outcomes, patient and technique survivals in patients with PKD performing PD and to define whether PD is appropriate for these patients.
Totally 99 patients: 33 with PKD and 66 with diseases other than PKD were included in this retrospective study. All patients started PD between 2001 and 2015 years and have been matched by time of PD therapy initiation. Socio-demographic characteristics, clinical data and complications during the specified period were evaluated. The factors associated with mortality and patient and technique survival were investigated for all patients.
The two groups were similar in terms of demographic, baseline and last visit clinical and laboratory parameters, additional systemic diseases, with the exception of higher pretreatment and last visit serum albumin levels in PKD patients (P=0.03 and 0.01 respectively) and younger age of non-PKD patients (P=0.002). Incidence of peritonitis and catheter exit-site/tunnel infections were similar among the two groups (P=0.26 and 0.12 respectively). The two groups were similar in terms of leak and hernia developments (P=0.07 and 0.57, respectively). By the end of the study period; in PKD group, 10 patients had been transferred to HD and had kidney transplantation and only 6 patients had died. In non-PKD group, 19 patients had been transferred to HD, 11 patients had kidney transplantation and 23 patients had died. Mortality was lower in PKD group (log rank=0.034). The two groups were similar regarding death and HD transfer reasons (P=0.35 and 0.36 respectively). The technique survival rates were similar among the two groups (log rank=0.37).
Peritoneal dialysis may be a suitable renal replacement therapy option for PKD patients. PKD is not an additional risk factor in patients treated by PD. Mortality is similar with non-diabetic PD patients. Peritoneal dialysis in PKD patients is associated with a similar overall rate of technique survival, incidences of hernia, leak and infectious complications as in non-PKD patients.
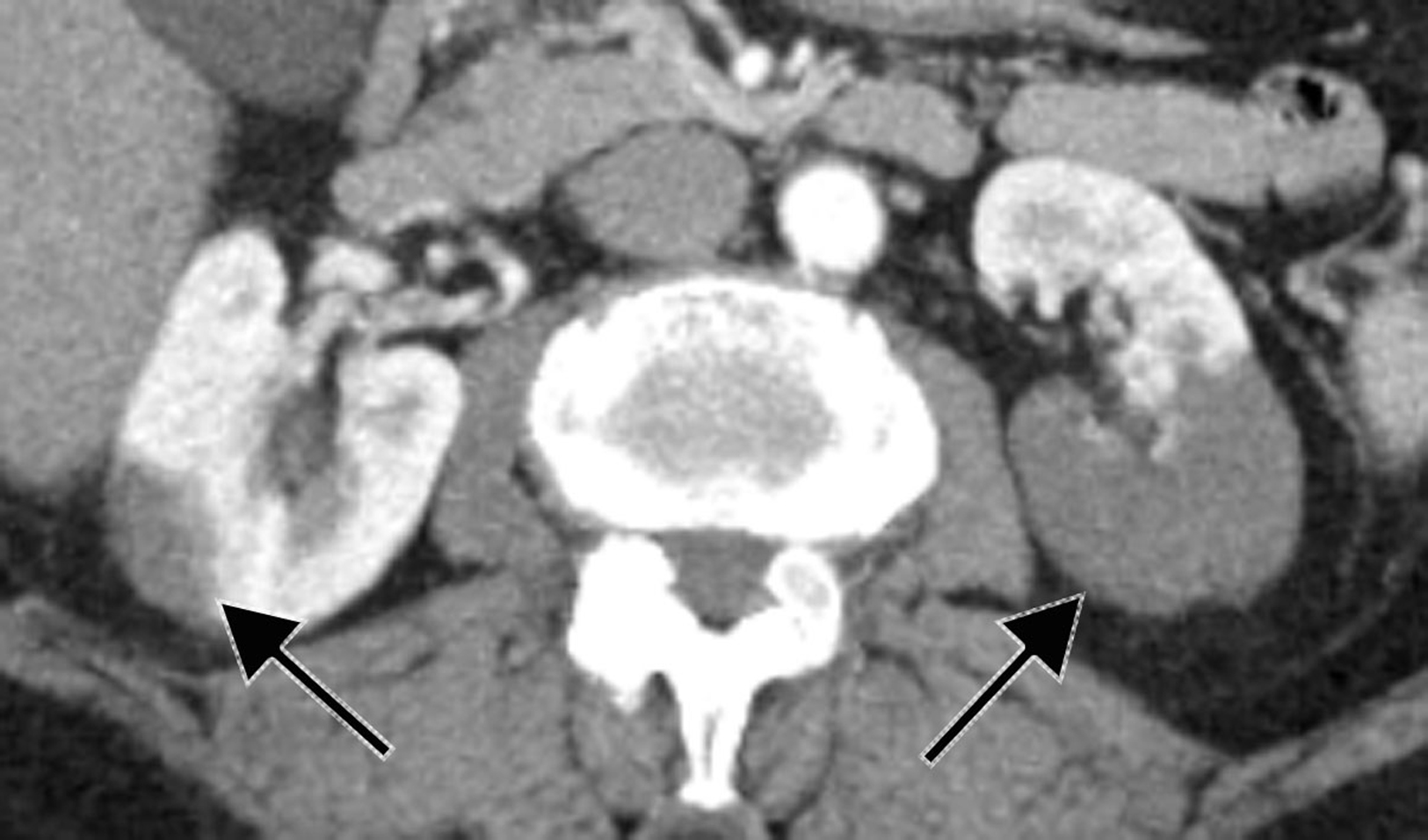
L’ischémie aiguë rénale est une pathologie rare et sous-diagnostiquée. L’expression clinique peu spécifique et les nombreux diagnostics différentiels rendent son diagnostic difficile pour le clinicien. L’origine cardio-embolique est la cause la plus fréquente. Le scanner abdominal injecté est l’examen de choix qui permet le diagnostic. Le pronostic global de cette pathologie est bon, malgré la gravité rénale potentielle de l’affection. La rapidité de la prise en charge initiale conditionne le pronostic ultérieur. Il n’existe actuellement pas de véritable consensus pour la prise en charge de cette pathologie. Une anticoagulation efficace constitue la base du traitement médical, la place de la thrombolyse est encore discutée. Nous présentons ici le cas d’une patiente âgée de 73 ans présentant un infarctus rénal bilatéral à l’arrêt d’un traitement anticoagulant.
Acute renal infarction is an uncommon and often under diagnosed condition mostly because of misleading symptoms. Accurate data regarding clinical presentation, laboratory tests, diagnostic and treatment are lacking. Detection is often delayed or missed because of non-specific clinical presentation. The mechanisms of acute renal infarction are various, mainly embolic or thrombotic. Abdominal CT scan remains the most valuable exam to confirm the diagnosis. Therapeutic guidelines for the treatment of renal embolism have not been well established. The standard treatment strategy includes anticoagulation with or without thrombolysis. Despite the uncertainty regarding management, the renal outcome remains favorable. Some patients do develop some degree of renal insufficiency during the acute episode. We report here the case of a 73-year-old woman with bilateral acute renal infarction after discontinuation of anticoagulant therapy.