Néphrologie & Thérapeutique
MENUDiagnosis and treatment of catheter-related bloodstream infection in hemodialysis: 10 years later Volume 18, issue 2, Avril 2022
- Key words: Catheter-related bloodstream, Catheter-related infection, Hemodialysis, Microbiological epidemiology
- DOI : 10.1016/j.nephro.2021.08.010
- Page(s) : 80-8
- Published in: 2022
The use of traditional immunosuppressive medicines for the treatment of membranous nephropathy is being challenged, owing to its limited efficacy and tolerability. Research on M-type phospholipase A2 receptor antibodies has provided a new way for evaluating the efficiency and prognosis of treatment of membranous nephropathy. However, the relationship between rituximab, a monoclonal antibody against CD20, and antiphospholipase A2 receptor antibodies and the drug regimen of rituximab for membranous nephropathy is uncertain. We conducted a meta-analysis to evaluate the efficacy of rituximab treatments in membranous nephropathy and compared the clinical effects of first-line and second-line rituximab therapies.
PubMed, Embase, Web of Science, Scopus, the Cochrane Central Register of Controlled Trials, and ClinicalTrials.gov were searched to find articles about rituximab treatment of patients with membranous nephropathy between January 2000 and August 2020. The outcomes included remission, antiphospholipase A2 receptor antibodies, relapse, and adverse events. The Grading of Recommendations Assessment Development and Evaluation criteria were used to evaluate the strength of evidence.
A total of 723 participants from 11 trials were included in this meta-analysis. The other treatments included cyclosporine, cyclophosphamide, steroids, and non-immunosuppressive antiproteinuric treatment. Rituximab significantly improved cumulative remission (P=0.007; Odds Ratio [OR]=3.06; 95% confidence interval [CI]=1.35–6.94) compared with other treatments. It significantly reduced relapse (P<0.00001; OR=0.06; 95% CI=0.02–0.19), antiphospholipase A2 receptor antibody levels (P=0.0009; SMD=−0.52; 95% CI=−0.83 to −0.21), and the proportion of patients positive for anti-PLA2R antibodies (P=0.003; OR=6.11; 95% CI=1.85–20.24) compared with other treatments. Compared with the second-line, first-line rituximab therapy achieved a higher rate of cumulative remission (P=0.03; OR=0.32, 95% CI=0.11–0.91).
Rituximab can improve the rate of clinical remission in patients with membranous nephropathy. Rituximab was more effective than other treatments in reducing relapse, antiphospholipase A2 receptor antibody levels, and the proportion of patients positive for antiphospholipase A2 receptor antibodies. The clinical remission rate following first-line rituximab therapy was better than that of second-line rituximab therapy for membranous nephropathy.
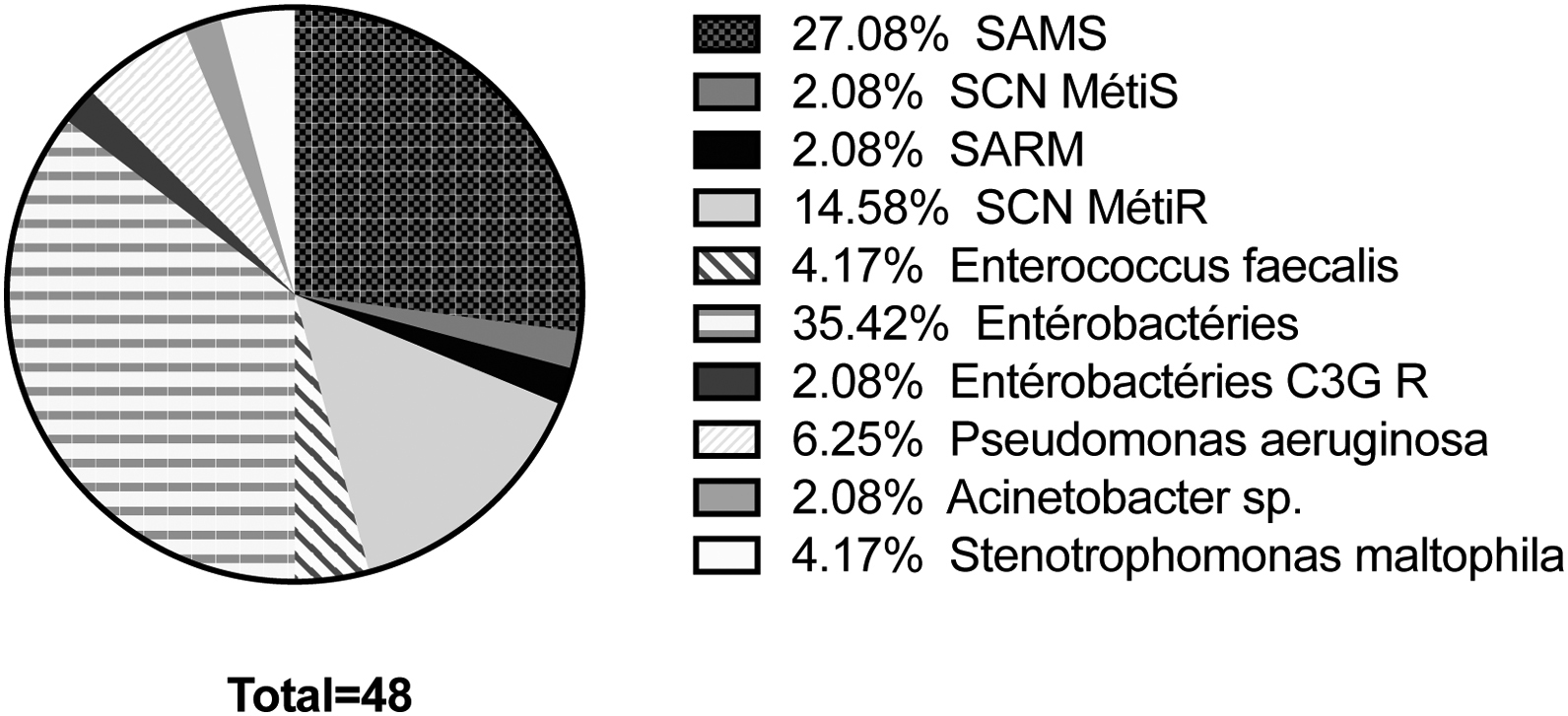
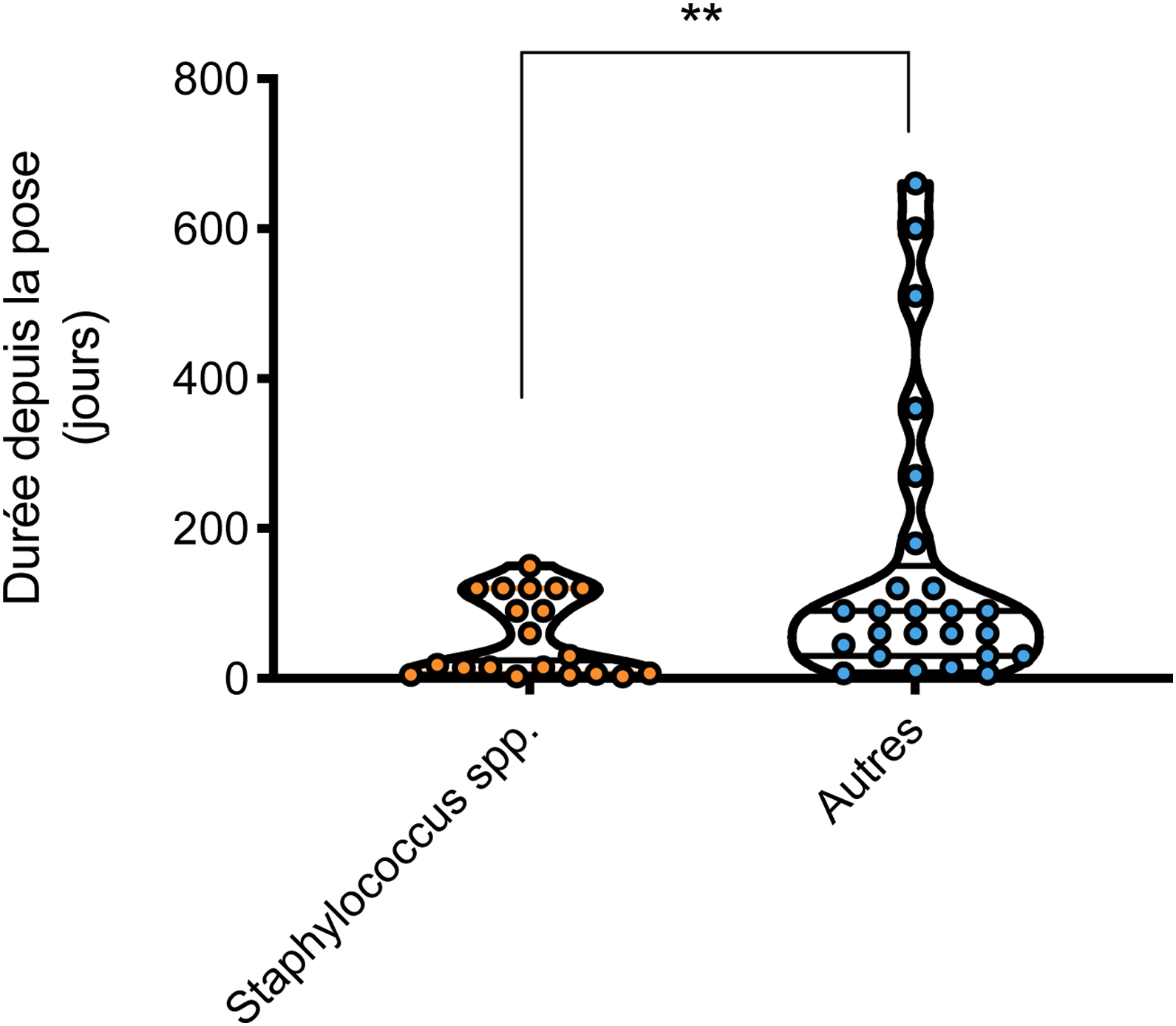
La population de patients traités par hémodialyse sur cathéter est fragile, à risque infectieux important. La bactériémie liée au cathéter d’hémodialyse est l’une des complications les plus graves, dont l’incidence augmente chaque année, en lien avec une hausse de l’utilisation des cathéters comme abord vasculaire. Cependant, le diagnostic clinique et microbiologique reste difficile. La mise en place de l’antibiothérapie probabiliste se base sur des recommandations anciennes qui préconisent d’associer une molécule visant le Staphylococcus aureus méticillino-résistant, ainsi qu’une bêtalactamine active sur P. aeruginosa, mais également d’adapter ce traitement probabiliste en réalisant un recueil microbiologique à l’échelle locale, ce qui est rarement réalisé. Dans notre centre d’hémodialyse du CHU de Bordeaux, une analyse de la répartition bactériologique des bactériémies liées au cathéter d’hémodialyse sur la période 2018–2020 a permis de proposer, en accord avec les infectiologues, un protocole d’antibiothérapie probabiliste adaptée. Cette démarche nous a permis de constater une incidence faible de méticillino-résistance des Staphylocoques, une incidence nulle de Staphylocoque après un délai de pose du cathéter de plus de 6 mois, aucun Pseudomonas multirésistant et un très faible pourcentage d’entérobactérie résistant aux céphalosporines. La mise à jour régulière de l’épidémiologie microbiologique des bactériémies liées aux cathéters d’hémodialyse, associée à un partenariat avec l’équipe d’infectiologie dans son centre d’hémodialyse, permettant une adaptation de l’antibiothérapie probabiliste, paraît avoir une bonne faisabilité et, à long terme, favoriser la préservation de l’écologie microbienne à l’échelle individuelle et collective pour la population de patients traités par hémodialyse.
Patients in hemodialysis on central venous catheter as vascular access are at risk of infections. Catheter-related bloodstream infection is one of the most serious catheter-complications in hemodialysis patients. Its clinical and microbiological diagnosis is challenging. The implementation of empiric antibiotic therapy is based on old recommendations proposing the combination of a molecule targeting methicillin-resistant Staphylococcus aureus and a betalactamin active on P. aeruginosa, and also adapting this probabilistic treatment by carrying out a microbiological register on a local scale, which is rarely done. In our hemodialysis center at Bordeaux University Hospital, an analysis of the microorganisms causing all catheter-related bloodstream infection over the period 2018–2020 enabled us to propose, in agreement with the infectious disease specialists, an adapted probabilistic antibiotic therapy protocol. This approach allowed us to observe a low incidence of meticillinoresistance of Staphylococcus. For catheters inserted more than 6 months ago, we observed no Staphylococcus, no multi-resistant Pseudomonas, and only 2% of Enterobacteria resistant to cephalosporins. A frequent updating of the microbiological epidemiology of catheter-related bloodstream infection, in partnership with the infectious diseases team in each hemodialysis center, allowing an adaptation of the probabilistic antibiotic therapy, and seems to have a good feasibility. This strategy might favor the preservation of microbial ecology on an individual and collective scale in maintenance hemodialysis patients.