Néphrologie & Thérapeutique
MENUDevenir des greffons rénaux refusés : expérience du centre de transplantation du CHU de Rennes Volume 19, issue 3, June 2023
- Key words: transplantation, survival, epidemiology, discard
- DOI : 10.1684/ndt.2023.23
- Page(s) : 187-200
- Published in: 2023
Introduction
In a context of tension on the number of available kidney transplants compared to the number needed, the practices of refusal of transplants in the Rennes transplantation center were evaluated.
Materials and methods
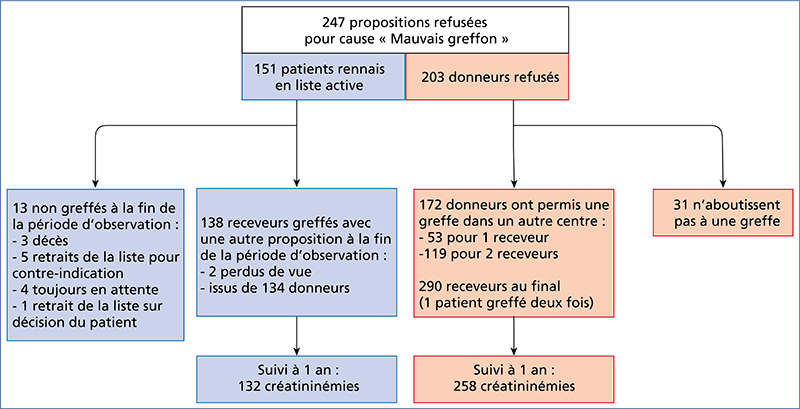
The donors completely refused by our team (no kidney accepted for any Rennes recipient) between January 1st 2012 and December 31st 2015 were identified from the national CRISTAL registry. The outcome of these refused transplants (possible transplantation in another center), the data of the recipients (from Rennes and other centers) and the data of the donors (refused and then finally accepted) were extracted.
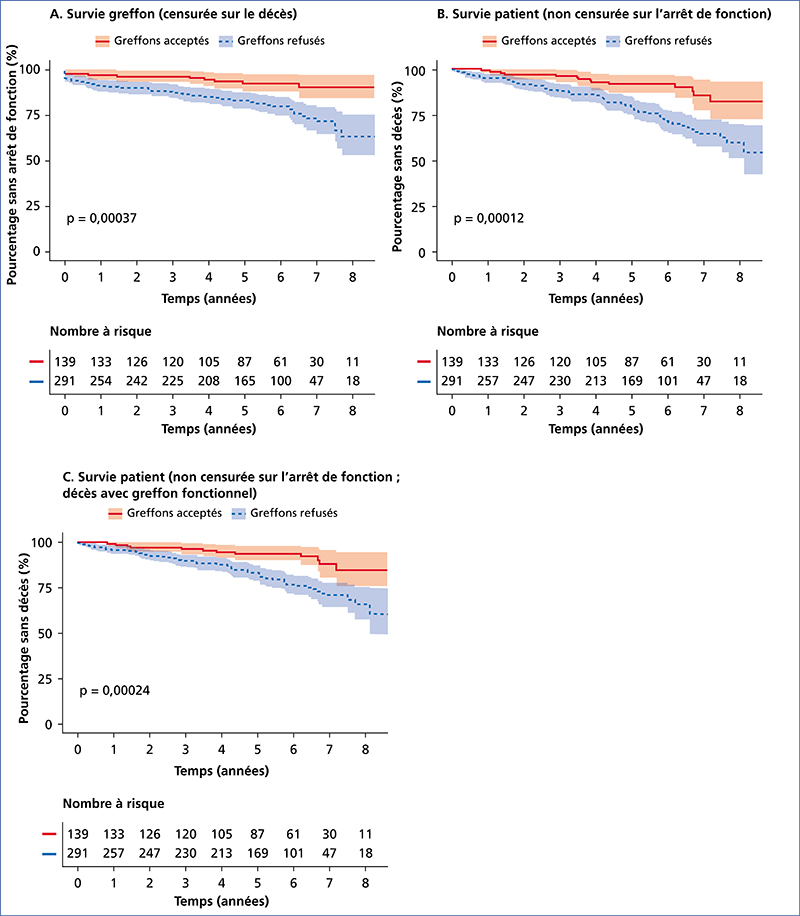
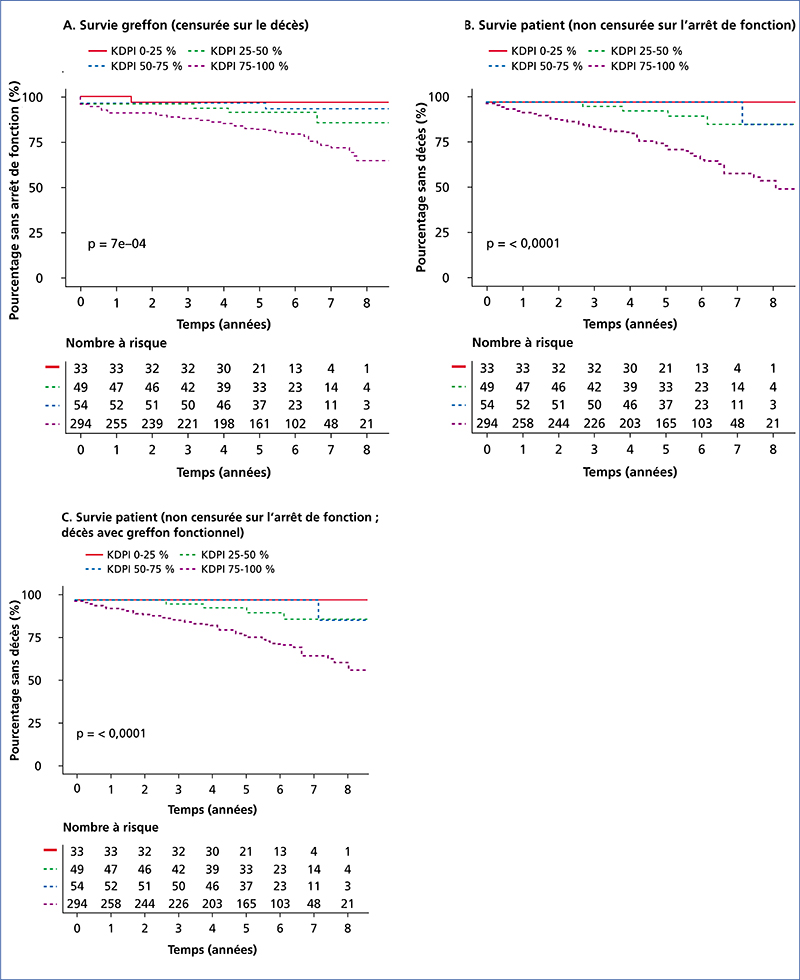
The outcome of recipients (from Rennes and other centers) was compared: graft survival (censored on death) and patient survival (not censored on cessation of function). The Kidney Donor Profile Index (KDPI) score was calculated and its usefulness studied.
Results
Among the 203 rejected donors, 172 (85 %) were accepted for transplantation in another center; 89% of these grafts were functional at one year. In univariate analysis, Rennes recipients transplanted after a refusal had a better graft survival (censored on death) than recipients transplanted in another center with the refused graft (p < 0.001). The main limitation of this analysis is the non-comparability of the groups. The KDPI score was significantly associated with graft survival (censored on death).
Of the 151 Rennes patients who had a refusal, 3 % were still on the waiting list at the end of the observation period, the others spent a median additional time on dialysis of 220 days (Q1-Q3 81-483).
Conclusion
Rennes recipients transplanted after a first refusal seem to have a better graft survival (censored on death) than recipients from other centers transplanted with refused grafts. This is to be weighed against the additional time on dialysis and even the risk of non-transplantation.