Hépato-Gastro & Oncologie Digestive
MENUManagement of anal fistulas in 2015 Volume 22, issue 9, Novembre 2015
Figures
Tables
Institut Léopold Bellan,
Service de proctologie médico-chirurgicale,
185, rue Raymond Losserand,
75014 Paris, France
service de gastroentérologie,
20, rue Leblanc,
75015 Paris, France
- Key words: anal fistula, sphincter, fistulotomy, sphincter preserving techniques, fibrin glue, ligation of the intersphincteric fistula track, FiLaC
- DOI : 10.1684/hpg.2015.1209
- Page(s) : 816-27
- Published in: 2015
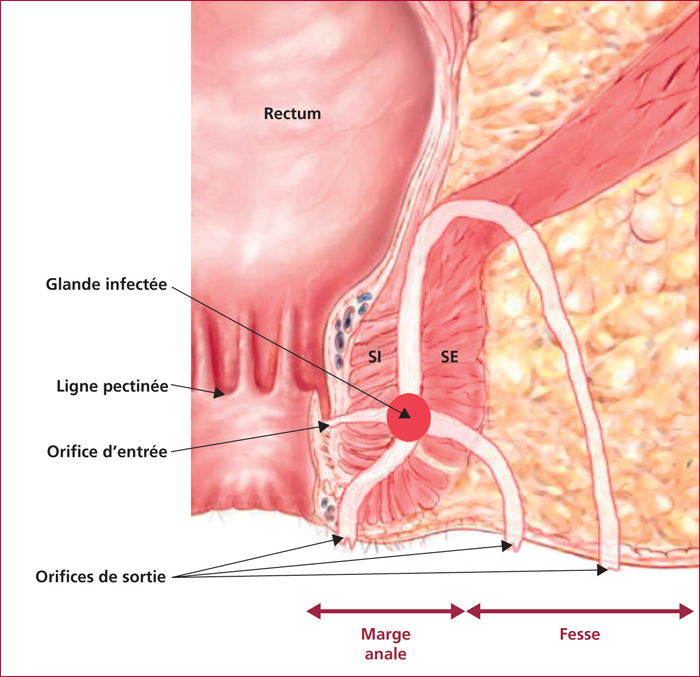
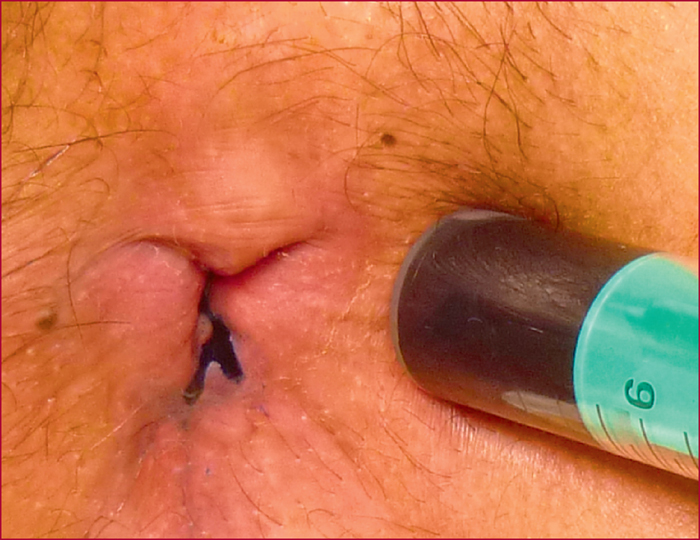
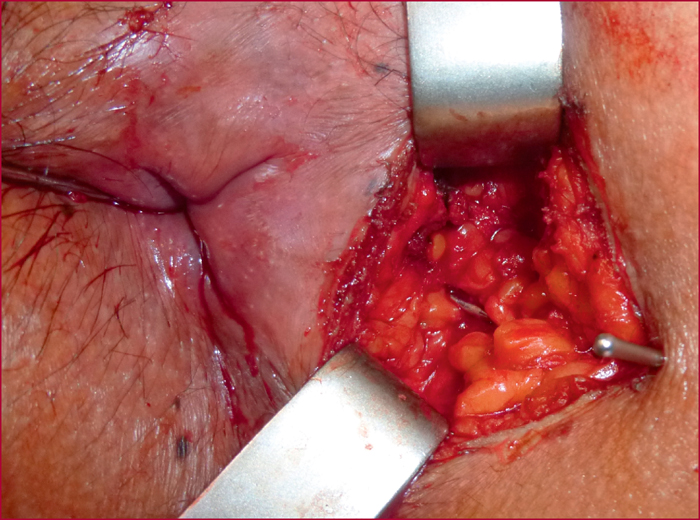
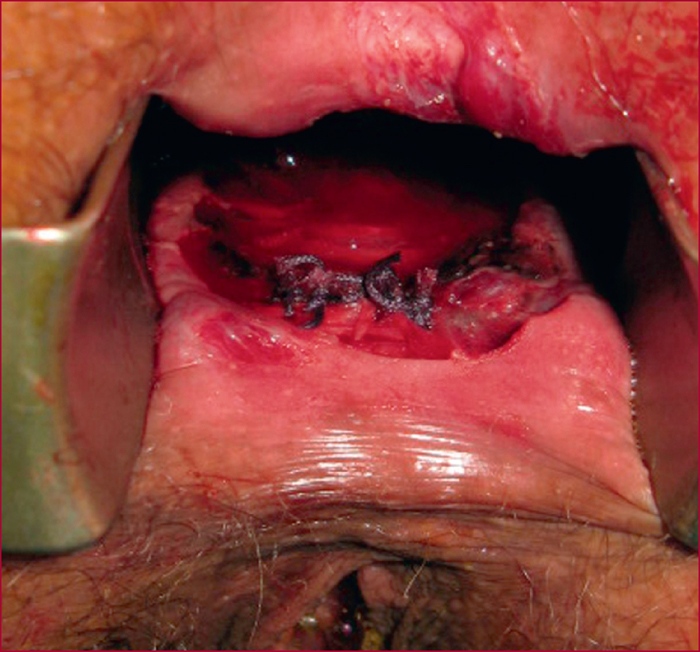
Anal fistula is the most common form of perianal sepsis. The etiology includes idiopathic fistulas, caused by cryptoglandular infection and fistulas secondary to other causes (Crohn's disease, iatrogenic, specific infections). Typically, a fistula includes an internal opening, a track, and an external opening. The treatment of anal fistula is a real challenge because of a risk of recurrence and anal incontinence. Fistulotomy is the gold standard: it is effective in terms of eradication of the fistula tract but it carries a risk of incontinence. Because of this risk, particularly for complex fistulas, sphincter-preserving techniques have been evaluated. Otherwise, success rate are lower than fistulotomy. Recents tecniques have interessant results (ligation of the intersphincteric fistula track, laser) but the lack of consistent results, level evidence and long-term follow-up, as well as the heterogeneity of fistula pathology avoid a definitive treatment algorithm.