Hépato-Gastro & Oncologie Digestive
MENUPancreatitis and hypertriglyceridemia: From physiopathology to management Volume 25, issue 10, Décembre 2018
- Key words: pancreatitis, hypertriglyceridemia, pancreatic necrosis, lipoprotein lipase deficiency, familial chylomicronemia syndrome
- DOI : 10.1684/hpg.2018.1709
- Page(s) : 1013-20
- Published in: 2018
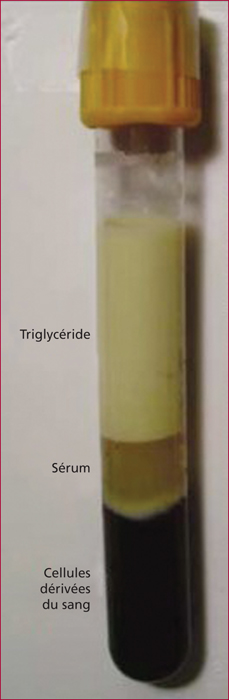
The exact incidence of hypertriglyceridemia-induced pancreatitis is not clearly known but increased regularly and is probably under-estimated due to diagnosis bias. Hypertriglyceridemia is mainly associated with chronic alcoholism abuse and is not systematically investigated in every-day practice. Acute pancreatitis and complications management has to be the same as for other pancreatitis. However, hypertriglyceridemia-induced pancreatitis are more severe, necrotizing and patients have usually numerous co-morbidities, i.e. diabetes, pregnancy, chronic kidney failure, obesity, metabolic syndrome, leading to organ failures. In case of hypertriglyceridemia, the risk of pancreatitis and the severity are correlated with the triglycerides levels. To limit recurrent pancreatitis, a pluri-disciplinary management has to be organized with dietician and endocrinologists, especially.
![]() This work is licensed under a
Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License
This work is licensed under a
Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License