Hépato-Gastro & Oncologie Digestive
MENUNutrition in digestive oncology Volume 24, issue 6, Juin 2017
Hôpital de Hautepierre, pôle des pathologies digestives, hépatiques et de la transplantation,
service d’hépato-gastroentérologie et d’assistance nutritive,
67098 Strasbourg Cedex, France
Laboratoire « Voies de signalisation du développement et du stress cellulaire dans les cancers digestifs et urologiques »,
Université de Strasbourg, Faculté de Médecine, 3 avenue Molière,
67200 Strasbourg, France
Université de Strasbourg, Faculté de Médecine,
4 rue Kirschleger, 67085 Strasbourg Cedex, France
- Key words: malnutrition, cancer, immunonutrition, surgery, enteral nutrition
- DOI : 10.1684/hpg.2017.1473
- Page(s) : 595-605
- Published in: 2017
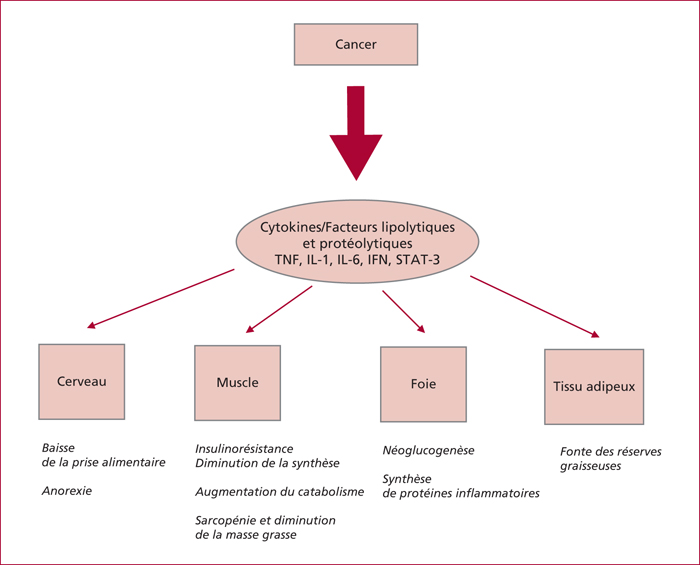
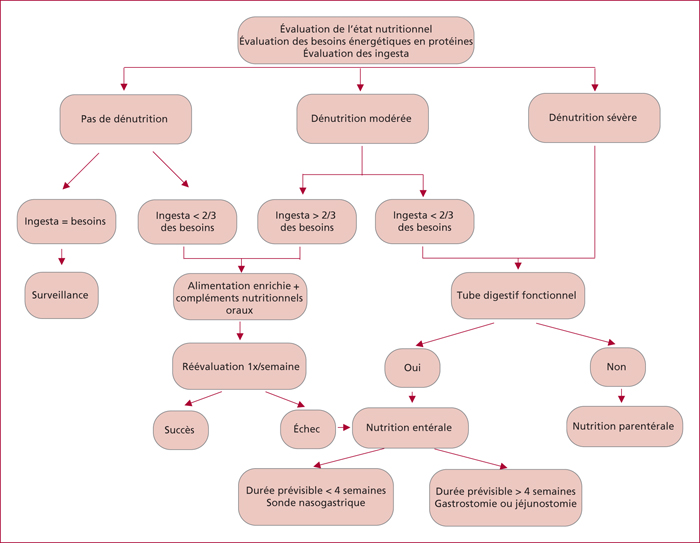
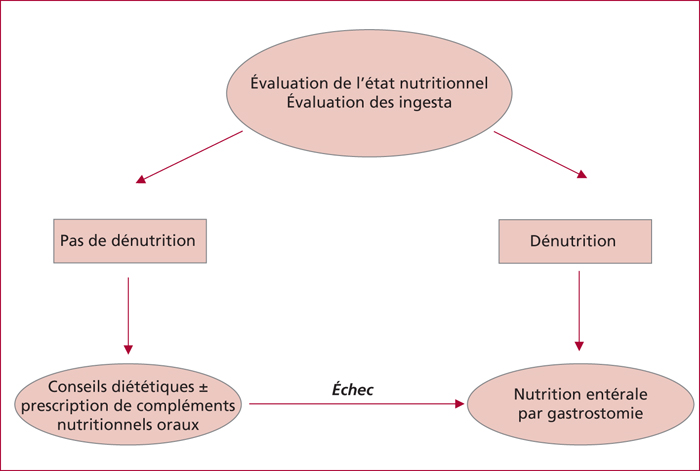
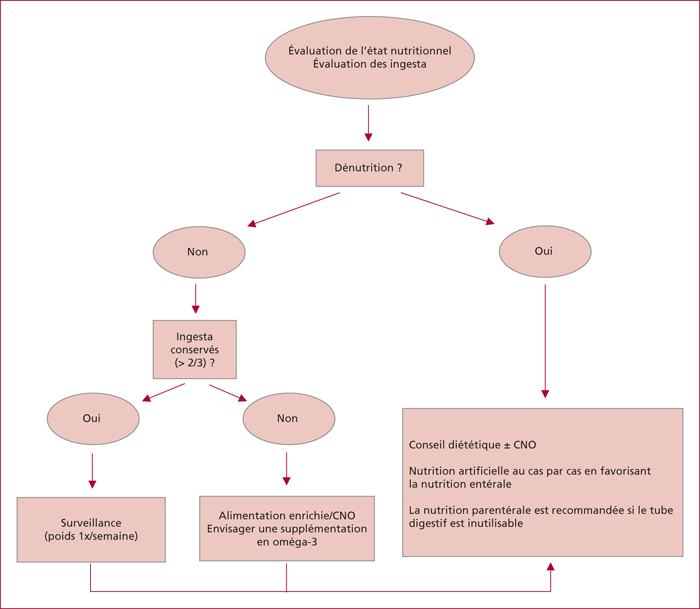
Malnutrition is frequent in patients suffering from digestive cancers, concerning about 50% of them. Malnutrition is multifactorial (anorexia, hypercatabolism, treatments’ side effects, etc.) and is a factor of poor prognosis as well as it decreases treatments’ tolerance. Nevertheless, its detection must still progress since more than 10% of cancer patients suffering from malnutrition did not receive any kind of nutritional support. Its diagnosis is primarily based on simple clinical and biological parameters such as weight and height to calculate the body mass index, the kinetics of weight loss and the measurement of the serum albumin concentration. Methods used for delivering nutritional support depend on malnutrition's severity, functionality of the digestive tract, and patients’ spontaneous caloric intake. It is based on oral nutritional complements, enteral nutrition by nasogastric tube feeding, gastrostomy or jejunostomy, and finally parenteral nutrition only in case of failure of enteral nutrition or if the digestive tract is not working properly. Evaluation of nutritional status has to be performed in the preoperative period and during the whole treatment period in order to guide and adapt the nutritional support. Currently, preoperative pharmaconutrition during 5 to 7 days is considered as a standard procedure in order to reduce the risk of infectious complications. Oral or enteral nutritional support is also indicated as soon as possible in the postoperative period. In patients needing radiochemotherapy the objective of the nutritional support is to avoid undesired treatment interruptions due to poor tolerance. When malnutrition is present, enteral nutrition is usually chosen. In patients on chemotherapy there is no a priori indication for a systematic use of nutritional support if the spontaneous oral intake is maintained. Finally, the use of orexigene drugs should be only discussed in palliative situations, if the importance of the weight loss interferes negatively with the patients’ life projects or if the symptom “hypophagia” is a major complaint expressed by the patient.