Hépato-Gastro & Oncologie Digestive
MENUCirrhosis, liver transplantation and pregnancy Volume 27, issue 4, Avril 2020
- Key words: cirrhosis, pregnancy, portal hypertension, liver transplantation, contraception
- DOI : 10.1684/hpg.2020.1946
- Page(s) : 375-85
- Published in: 2020
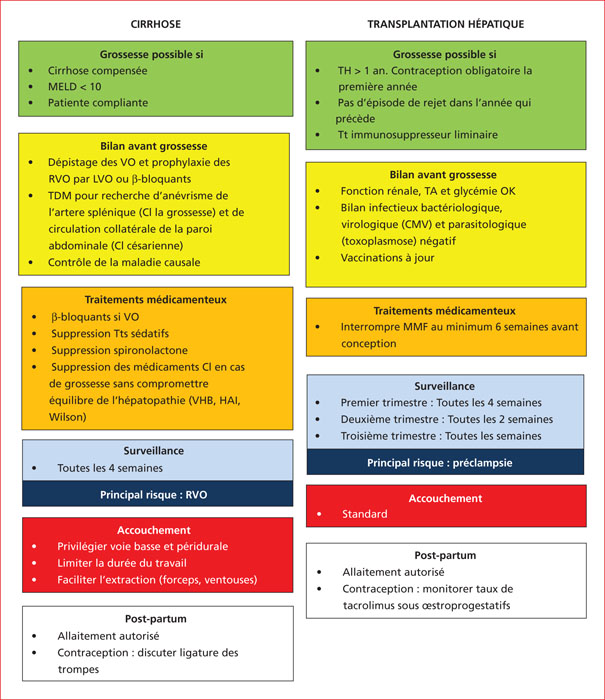
Due to hormonal disorders induced by cirrhosis, pregnancy is a rare event in women with cirrhosis. When it occurs, it is at risk for the mother and the fetus, especially when the MELD score is high at the time of conception. The risks for the mother concern the occurrence of hepatic complications, the most frequent being variceal bleeding (30 to 50% of cases depending on whether or not there is preexistent portal hypertension), but also the more frequent occurrence of pregnancy-related complications, especially anemia, hemorrhages and postpartum infections. For the fetus, there is a greater risk of stillbirth, premature birth, cesarean delivery, and low birth weight. Pregnancy is therefore only possible in the event of stable, compensated cirrhosis, with portal hypertension being optimally controlled; and if the patient agrees to a very close specialized follow-up. Fertility is quickly restored after liver transplantation in most women, which requires discussing the initiation of effective contraception in all liver transplant women of childbearing age. During pregnancy, the most common complications observed in the mother are related with to the use of immunosuppressant agents and involve gestational diabetes, hypertension, and pre-eclampsia. The rates of preterm delivery and cesarean birth are also higher. Immunosuppressive therapy should be adapted before pregnancy, mainly by withdrawing mycophenolate mofetil and mycophenolate sodium, and then closely monitored during pregnancy. There is a higher risk of rejection, but the long-term prognostic impact remains controversial. Pregnancy is therefore possible in a woman with a liver transplant at least 1 year (or even 2 years) after the transplant, when graft function is optimal with the lowest doses of immunosuppressant agents, and no episode of rejection recorded within the previous year.