Epileptic Disorders
MENUThe aetiology of psychogenic non-epileptic seizures: risk factors and comorbidities Volume 21, issue 6, December 2019
- Key words: dissociative seizures, psychogenic non-epileptic seizures, aetiology, risk factors, comorbidity
- DOI : 10.1684/epd.2019.1107
- Page(s) : 529-47
- Published in: 2019
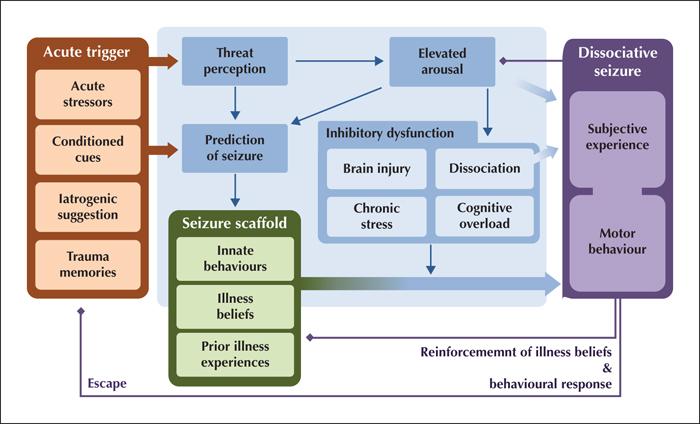
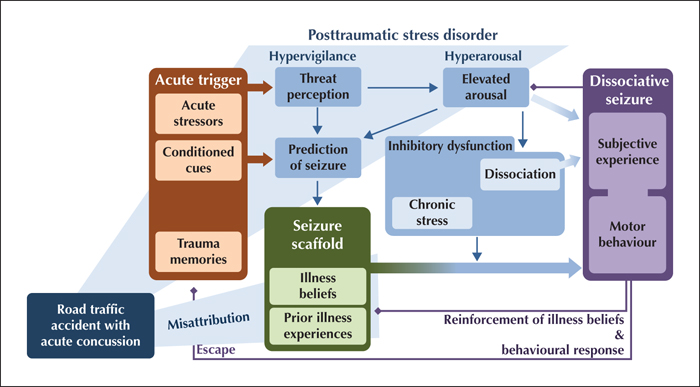
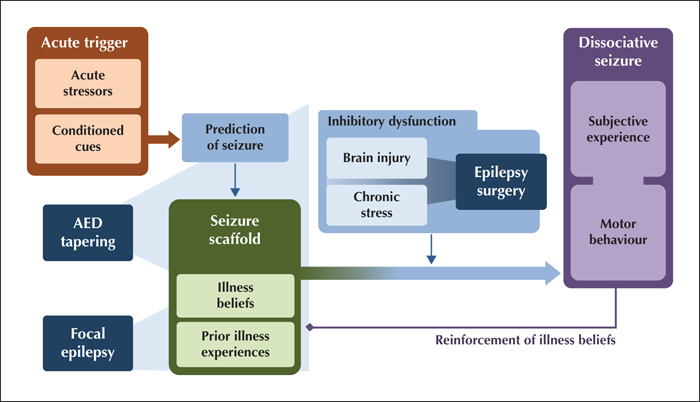
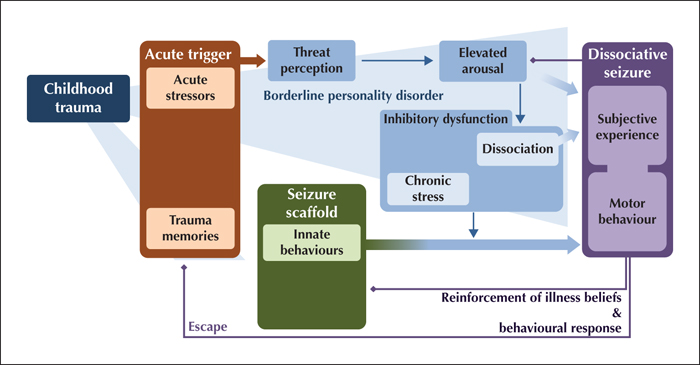
Psychogenic non-epileptic seizures (PNES), also known as dissociative seizures, are paroxysms of altered subjective experience, involuntary movements and reduced self-control that can resemble epileptic seizures, but have distinct clinical characteristics and a complex neuropsychiatric aetiology. They are common, accounting for over 10% of seizure emergencies and around 30% of cases in tertiary epilepsy units, but the diagnosis is often missed or delayed. The recently proposed “integrative cognitive model” accommodates current research on experiential, psychological and biological risk factors for the development of PNES, but in view of the considerable heterogeneity of presentations and medical context, it is not certain that a universal model can capture the full range of PNES manifestations. This narrative review addresses key learning objectives of the ILAE curriculum by describing the demographic profile, common risk factors (such as trauma or acute stress) and comorbid disorders (such as other dissociative and functional disorders, post-traumatic stress disorder, depressive and anxiety disorders, personality disorders, comorbid epilepsy, head injury, cognitive and sleep problems, migraine, pain, and asthma). The clinical implications of demographic and aetiological factors for diagnosis and treatment planning are addressed.