Epileptic Disorders
MENUSurgery for drug-resistant tuberous sclerosis complex-associated epilepsy: who, when, and what Volume 23, issue 1, February 2021
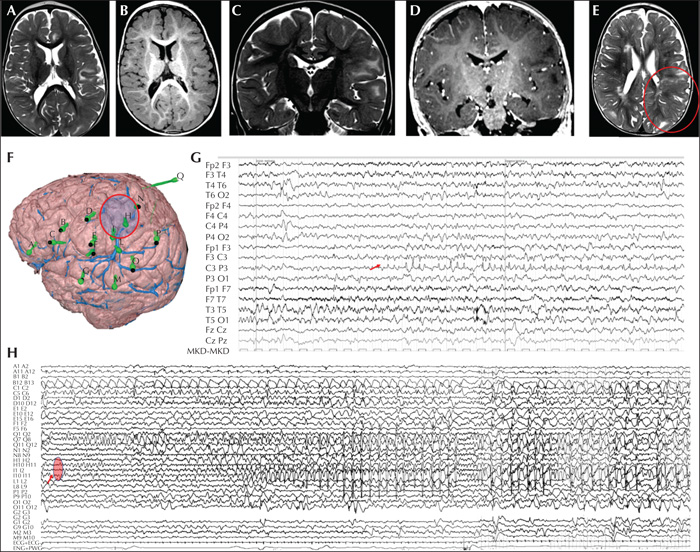
Figure 1
Presurgical evaluation of a two-year-old patient with a TSC2 genetic variant and drug-resistant epilepsy. Seizures started at the age of two months. Neurological examination revealed right hemiparesis and cognitive delay. The patient presented with both focal right hemiclonic seizures and focal asymmetric epileptic spasms with right arm prevalence. (A-E) Brain MRI at the age of 20 months. (A-D) Axial and coronal T2 and T1-weighted sequences showing multiple hyperintense areas on T2-weighted sequences and hypointense on T1-weighted sequences for bilateral tubers. (E) Parietal postcentral tuber marked with a circle, showing blurring of the grey-white matter, which was explored using intracranial electrodes (N, H, I) and involved the seizure onset. (F) Intracranial SEEG exploration of the left hemisphere using 15 electrodes: eight electrodes (D, E, F, N, H, I, L, Q) were used to explore the perirolandic tuberal area; three electrodes (A, B, C) for the anterior frontal region; two electrodes (G, M) for the superior temporal gyrus; and two (O, P) for the posterior parietal region. (G) Video-EEG recording showing a focal seizure, with paroxysmal rhythmic discharge of spikes and sharp waves with phase reversal at electrode C3. Clinically, the patient presented with chin contractions, reduced awareness, inconstantly associated with left eye deviation. (F) SEEG recording showing a focal seizure starting as theta rhythmic activity over electrodes Q, N, H, I, evolving into spike-and-wave complexes, mixed with sequences of fast activity. Clinically, the patient demonstrated a mild reduction in responsiveness during the initial ictal discharge, followed by a brief tonic contraction of the right side during the fast activity.
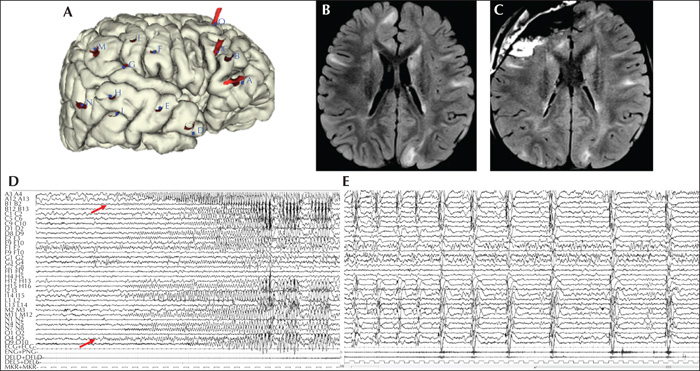
Figure 2
Presurgical evaluation and surgical approach in a five-year-old patient with a TSC1 genetic variant. Epilepsy onset occurred at four months of age, with epileptic spasms without clear-cut clinical lateralization. Afterwards, the patient started to present with focal seizures characterized by right head deviation and diffuse tonic contraction (left>right), followed by subtle epileptic spasms (mild head deviation). Psychomotor development was moderately delayed, language was strongly delayed, and autistic features were evident. Video-EEG showed right multifocal continuous interictal epileptiform abnormalities. (A) Intracranial SEEG exploration of the right hemisphere using 18 electrodes: four electrodes (A, B, C, O) were used to explore the frontal lobe, both basal and dorsal surface; six electrodes (D, E, H, I, N, G) for the temporal lobe; and three electrodes (F, L, M) for the posterior parietal area. (B) Preoperative brain MRI showing multiple bilateral tubers with hyperintensity on FLAIR-weighted sequences. (C) Post-operative brain MRI showing that the resection area corresponded to the right fronto-basal region which was identified by the SEEG study. Three years post-surgery, the patient was seizure-free, with improvement in language and interaction. (D) The SEEG recording showing a focal seizure starting with a low-voltage fast discharge over electrodes B, C, O, followed by rhythmic theta activity at the same electrodes and over electrode A; soon after, the ictal discharge involved temporal electrodes (D, E, H, M, N) with spike and spike-and-wave complexes. (E) The focal seizure was followed by a cluster of epileptic spasms characterized by pseudorhythmic complexes of spikes, followed by a high-voltage slow wave, mixed with fast activity evident at electrodes A3-4. The clinical counterpart was subtle (mild bilateral muscular activation on polygraphic traces).
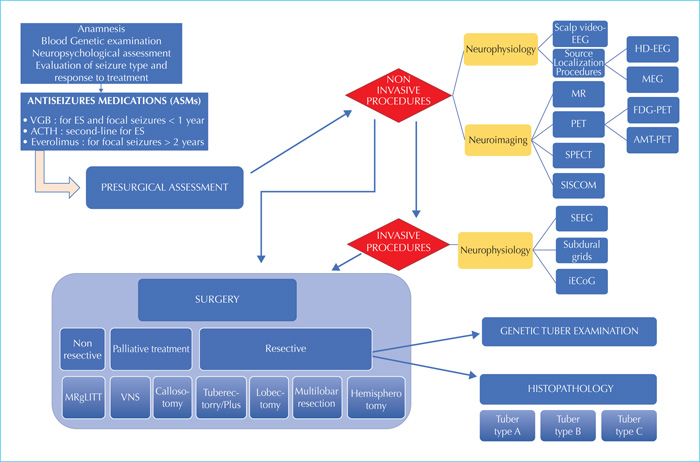
Figure 3
Diagnostic and interventional algorithm for patients with TSC and drug-resistant epilepsy.

