Epileptic Disorders
MENUShort-term effectiveness of a condensed series of standard EEG lectures for adult neurology residents Volume 24, issue 2, April 2022
Electroencephalography (EEG) plays a central role in the care of patients with seizure and epilepsy. Accurate EEG interpretation, therefore, is mandatory for optimal care of this patient population. Since a major portion of those who read EEG are general neurologists without additional, post-residency training in clinical neurophysiology and/or epilepsy [1], ensuring successful neurology resident EEG education is of paramount importance. Evidence suggests, however, that an alarming portion of graduating adult neurology residents in the United States does not feel confident reading EEGs independently [2].
A recent survey-based study involving adult neurology program directors in the United States showed that EEG education barriers are pervasive and include insufficient EEG exposure and ineffective didactics [3]. Despite didactics being reported as ineffective, this study identified that the most utilized EEG teaching methods are didactic-based [3]. Herein, we investigated (i) the short-term effectiveness of a series of traditional didactic EEG lectures in an adult neurology resident cohort and (ii) whether the educational benefit of such lectures correlates with residents’ prior formal EEG exposure.
Methods
We evaluated the short-term effectiveness of traditional EEG lectures by testing the EEG knowledge of a group of adult neurology residents with the use of a quiz before (pre-test) and after (post-test) a series of four lectures. Only those residents who underwent both pre- and post-tests and attended at least two of the four lectures were included. Moreover, we divided participants based on whether they had at least one EEG rotation during or prior to the study (Group A) or not (Group B). Each EEG rotation in our institution corresponds to a four-week period devoted to learning EEG. Notably, the EEG quiz as well as a portion of the data pertaining to participants included in this study, were published previously [4].
Residents’ EEG knowledge was measured with a quiz, which consisted of two parts: normal and abnormal EEG. These sections were composed of 27 and 10 EEG questions, respectively, all of which were obtained from the authors’ personal collections and were deemed to be highly informative. Residents were given 30 minutes to complete the quiz, which was scored based on one point for each correct answer; neither <one point nor negative points were given. A list of all the EEG features present in the quiz and the original test were previously published [4] and are summarized in table 1. The pre-test was completed immediately before the first lecture whereas the post-test was completed between 40 and 75 days after the pre-test. Residents did not receive their scores or the correct answers until the end of the study (i.e. after the post-test). Data are presented as mean±SEM, and normality condition was analyzed by the Shapiro-Wilk test. Two-tailed paired t-tests were used to compare pre- and post-test scores. A p value of less than 0.05 was considered to indicate statistical significance. Statistical analyses were performed using IBM (SPSS) Statistics Version 28.0 software.
The series of four lectures focused on the following topics: introduction to EEG and artifacts, normal and abnormal EEG, intensive care unit EEG, and ictal and interictal EEG findings; each lasting, on average, 60 minutes. All lectures were live/face-to-face and given by clinical neurophysiology-trained attending physicians (Drs. Jay Gavvala and Atul Maheshwari) within eight days of the pre-test. The learning objectives of the lectures are listed in table 2. The study was approved by the Baylor College of Medicine Institutional Review Board (IRB) and was performed in August 2019. All data are available upon request.
Results
Twelve residents met the inclusion criteria and were, therefore, included in this study: two PGY1 (one-year postgraduate), four PGY2, one PGY3, and five PGY4 residents. One of these residents (PGY3) failed to complete the abnormal EEG section of the pre- and post-test; therefore, this participant was not included in all analyses of the study. The time interval between the pre- and post-test ranged from 40 to 75 days, and six participants had not undergone any EEG rotation prior to or during the study. These data are summarized in table 3.
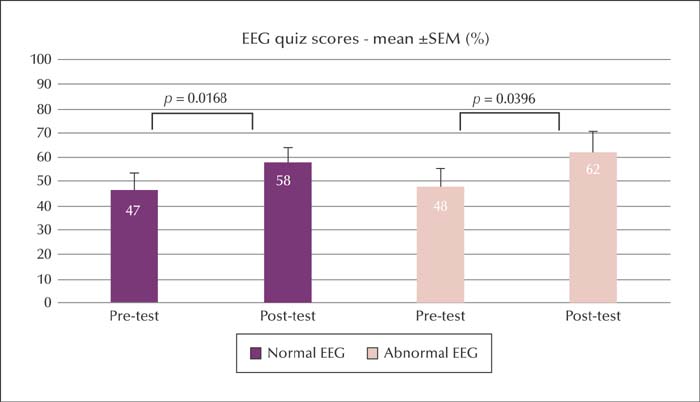
The overall pre-test scores (mean±SEM) for the normal (n=12) and abnormal (n=11) EEG sections of the test were 47±6.1% and 48±7.2%, respectively. The overall post-test scores (mean±SEM) for the normal (n=12) and abnormal (n=11) sections were 58±5.5% and 62±8.6%, respectively. There was a statically significant increase in overall score for both normal (p=0.0168) and abnormal (p=0.0396) EEG sections before and after the lecture series. These results are shown in figure 1.
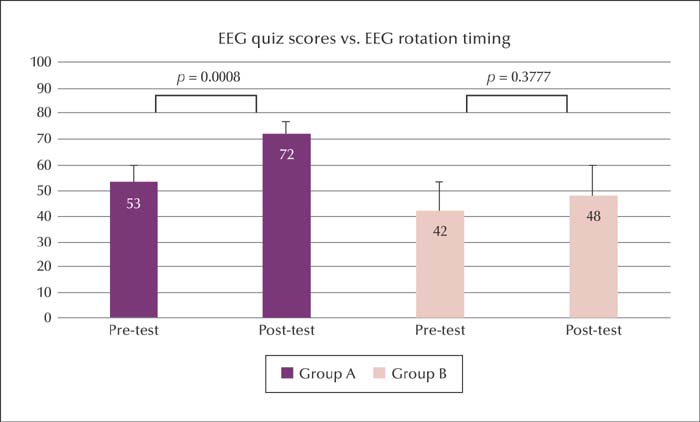
We further analyzed pre- and post-test scores (collectively including both normal and abnormal EEG sections; i.e., score = mean score for normal EEG section + mean score for abnormal EEG section/2) based on whether participants had (Group A) or had not (Group B) undergone EEG rotation(s) before or during the study (figure 2). One participant was excluded from this analysis because of a lack of data for the abnormal EEG sections of the test. Group A (n=6) pre- and post-test scores (mean±SEM) were 53±6.7% and 72±4.6%, respectively, and this score increase reached statistical significance (p=0.0008). Group B (n=5) pre- and post-test scores (mean±SEM) were 42±11.4% and 48±11.7%, respectively, however, this score increase did not reach statistical significance (p=0.3777).
Discussion
Our study shows that a series of four EEG lectures given by epilepsy attending physicians over a period of less than two weeks targeted at a cohort of adult neurology residents generates a statistically significant increase in residents’ measured EEG knowledge. Additionally, our results reveal that such a series of lectures is effective exclusively in residents who already have some degree of formal in-residency EEG exposure.
A better understanding of the benefits of various different EEG teaching methods is important in light of the high percentage of residents who do not feel confident reading EEG despite in-residency training [2, 4]. This issue was the impetus behind a survey involving adult neurology residency program directors in the United States focused on further defining the current state of residency EEG education [3]. Barriers to EEG education were reported by most program directors; the two most commonly mentioned were insufficient EEG exposure and ineffective didactics [3]. While increasing EEG exposure relies more on systematic changes to residency curricula, improving didactics requires a more in-depth characterization of the effectiveness of different EEG teaching methods – such as standard lectures.
Standard lectures have been reported as the most commonly used EEG teaching avenue in adult neurology residencies in the United States [3]. These lectures are most often delivered throughout the year (95%) and, less frequently, concentrated in a one to two-month protected course (30%) [3]. In our institution, the latter method has been the traditional way residents receive EEG education. From a resident standpoint, trainees in our institution have elected a combination of didactic lectures and reading EEGs with supervision as the most efficient way to teach EEG [4].
In addition to emphasizing the suboptimal overall resident EEG knowledge, which has been published extensively [4-6], our results provide a better understanding of the effects of delivering a condensed series of four EEG lectures given by epilepsy attending physicians. First, we show that these lectures generated a statistically significant increase in residents’ EEG knowledge – both related to normal (47±6.1% to 58±5.5%; p=0.0168) and abnormal (48±7.2% to 62±8.6%; p=0.0396) EEG - when tested one to two months thereafter. Upon subanalysis of these results, we identified an overall improvement in residents’ EEG knowledge following lectures, primarily based on better post-test scores of those residents who already had at least some degree of formal in-residency EEG exposure (53±6.7% to 72±4.6%; p=0.0008) compared to those who did not have any prior EEG exposure (42±11.4% to 48±11.7%; p=0.3777).
Despite the relatively low number of participants in our study, which was a major limitation, our data suggest that delivering condensed EEG lectures by epilepsy attending physicians is effective for short-term knowledge retention particularly among adult neurology residents with some degree of prior formal EEG exposure during training. This observation, to the best of our knowledge, has not been reported in relation to resident EEG learning. However, neither the duration of in-residency EEG training (three or four months) nor the time since completion of training were shown to statistically affect residents’ EEG interpretation skills [6]. Similarly, neither the presence or absence of epilepsy rotation nor its duration statistically affected adult neurology residents’ abilities to recognize seizures based on the EEG of critically ill patients [7].
The discrepancy in effectiveness of EEG lectures depending on whether residents had prior EEG exposure may be explained in light of a recently proposed multi-theory learning model [8]. This model comprises five phases in learning experience, including dissonance, refinement, organization, feedback, and consolidation. We hypothesize that standard EEG lectures would only introduce new facts/concepts (thereby demonstrating that learners have an incomplete existing knowledge; dissonance) in residents naïve to EEG. However, for those residents with prior EEG exposure, these lectures would also serve to refine and, to a certain extent, aid in organizing knowledge, as well as possibly allowing feedback (residents had the opportunity to ask questions and receive feedback during lectures). Consequently, lectures would provide greater educational benefit in the latter group because multiple phases within the learning process would be addressed.
Based on the medical education literature [9], we also suggest that teachers consider incorporating the principles of adult learning theory into formulating and delivering EEG lectures. Considerations include shortening lecture duration (given learners’ limited attention spans), focusing on the highest-yield content, optimizing lecture organization, and ensuring that active learning strategies are involved.
Additional weaknesses in our study include a lack of information regarding residents’ potential EEG knowledge acquired prior to the beginning of residency – for example, one of the PGY1 residents included in this study had been exposed to EEG prior to residency. Further, the pre- and post-tests included the same questions, which might have given residents an advantage if they had memorized the test questions. We tried to mitigate this bias by not giving residents their scores or the correct answers until the very end of the study. We acknowledge that the normal and abnormal EEG findings included in the test may not represent the knowledge an adult neurology resident must have prior to graduation. Moreover, we only assessed short-term knowledge, hence it is unclear whether residents retained the acquired knowledge longer after the intervention. Lastly, one should be cautious in extrapolating the success of our lectures since their effectiveness highly depends on the lecturers themselves and their ability to transmit knowledge [10].
In the pursuit of improving resident EEG education, we would like to highlight that a condensed series of standard lectures may still be an invaluable asset for teaching trainees how to read EEGs – especially those with at least some degree of EEG knowledge. Based on our results, it would be advisable to ensure that residents undergo hands-on EEG exposure through formal rotations either prior to or during standard lectures in order to allow this teaching avenue to generate maximal educational benefits. Other methods, such as supervised EEG reading and e-learning programs – for example, those promoted by the International League Against Epilepsy (ILAE) [11] – should complement didactic-based education. Future studies should investigate the short- and long-term effectiveness of standard lectures in larger cohorts of residents as well as the effectiveness of formal EEG rotation(s) in isolation.
Acknowledgements and disclosures
We would like thank Dr. Hang Lee for his assistance in performing the statistical analysis in this study.
FAN is a member of the Epileptic Disorders Editorial Board. MM, MO, and JRG report no disclosures relevant to the manuscript.
* This study's data was partially presented at the 34th American Epilepsy Society meeting as an abstract.