Epileptic Disorders
MENUMoCA as a cognitive assessment tool for absence status epilepticus Volume 22, issue 2, April 2020
Figures
Absence status epilepticus (SE) is clinically characterized by the presence of a prolonged confusional syndrome that can be accompanied by subtle automatisms or autonomic phenomena.
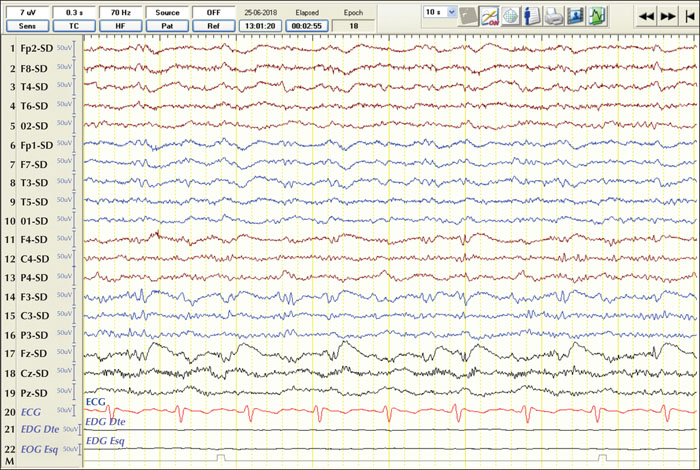
In addition, periodic spike-and-wave and/or polyspike-and-wave discharges on EEG are neurophysiological biomarkers (Genton et al., 2008). When appropriate treatment is started, both clinical and EEG improvement usually occurs (Thomas et al., 1993). Continuous EEG is the gold standard to monitor the response, but this is not available in all centres. Furthermore, cognitive symptoms associated with this entity can be very subtle and difficult to detect, and no consensus exists on how their improvement can or should be clinically monitored.
In the present case study, we describe the use of a cognitive test - Montreal Cognitive Assessment (Nasreddine et al., 2005)- for the evaluation of therapy efficacy in a patient with absence status epilepticus.
The usage of cognitive tests to quantify and monitor cognitive impairment is not widespread, and literature on this topic is indeed limited. In a previous study (Profitlich, 2008), formal neuropsychological evaluations were performed for focal convulsive SE patients and different cognitive domain alterations were found, although patients mostly presented with impairment of consciousness and impairment of executive and higher-order functions. Nevertheless, is not possible to perform a formal and complete neuropsychological evaluation on all these patients. We describe the use of the MoCA to monitor cognitive improvement in parallel with neurophysiological improvement.
Case study
A 73-year-old man, with angioimmunoblastic T lymphoma, under chemotherapy, was admitted to our hospital and medicated with piperacillin/tazobactam and vancomycin, for a respiratory infection. This patient had no history of epilepsy and he was medicated with alprazolam for anxiety which was continued during admission. On the third day of hospitalization, he suffered a tonic-clonic generalized seizure and a neurological evaluation was requested. At neurological examination, he was confused with a marked attention deficit and disoriented to time. His speech was divergent and contradictory, and he had a recent memory defect. He scored 9 on the MoCA. Routine laboratory tests and cranial CT were unremarkable. His EEG (figure 1) showed repetitive spike-and-wave and polyspike-and-wave discharges, with a frequency of 1-2 Hz, with maximal projection in midline and bifrontal regions. A diagnosis of absence SE was assumed, and intravenous clonazepam was started. On the next day, he seemed less confused on neurological examination and scored 14 on the MoCA with significant decrease in epileptic activity on EEG. On the third day, he scored 23 on the MoCA and his EEG showed no epileptiform activity. The main improvements in MOCA were seen in attention, abstraction and orientation domains.
A lumbar puncture was not performed as the patient improved with antiepileptic therapy.
Discussion
De novo absence SE is included in the differential diagnosis for confusional syndromes and can occur in patients with no previous history of epilepsy. Several drugs, mainly psychotropic drugs, as well as benzodiazepine withdrawal have been associated with this entity (Thomas et al., 1993; Fernández-Torre, 2001;). The treatment requires correction of any possible trigger or precipitant factor, and therapy includes benzodiazepines and broad-spectrum antiseizure drugs. Although less common, recurrences may occur in some individuals (Baykan et al., 2002).
As Kaplan (Kaplan, 1996) observed, a diagnostic delay is frequent in these patients which is frequently due to the subtlety of cognitive disfunction. In our patient, a generalized seizure led us to request an EEG that was essential for the diagnosis. In fact, Andermann and Robb in 1972(Andermann and Robb, 1972), described that generalized tonic-clonic seizures can terminate or, more rarely, precede an absence status episode. EEG patterns in absence SE show large heterogeneity ranging from spike-and-wave discharges to asymmetric irregular sharp-and-slow-wave complexes with anterior predominance(Fernández-Torre, 2001).
In this patient, it is difficult to clearly identify the absence SE trigger. On the one hand, he was previously medicated with a benzodiazepine that was not suspended or changed during admission; nevertheless, we cannot be certain about this on the days preceding hospitalization. On the other hand, he was under antibiotherapy which has been associated with this entity. However, so far, only some cephalosporins that cross the haematoencephalic barrier have been described to induce absence status epilepticus(Thomas et al., 1992). Finally, the respiratory infection itself may have precipitated absence status epilepticus involving several different mechanisms.
Our working hypothesis was that a cognitive assessment test, such as the MoCA, could be useful to monitor this patient's improvement, therefore we decided to perform this assessment at three different times: first before initiating treatment, second during EEG improvement, and third after EEG normalization. A significant improvement in MoCA was seen as a sign of clinical recovery, with a total score ranging from 9 before treatment to 23 when EEG normalised. A learning effect may have accounted for the improvement, however, our patient had a serious memory impairment that certainly compromised learning capacity. Although the validity of the MoCA as a tool to monitor status epilepticus remains unproven, we chose this test because it constitutes a systematic and standardized way to access mental status, allowing comparison between patients and in the same patient at different times.
This concept of quantifying clinical and cognitive impairment as a therapy monitoring tool for absence status epilepticus is, to our knowledge, an original one. The use of cognitive tests to evaluate and monitor cognitive function in absence SE is not generalized and the literature on this subject is scarce. However, Profitlich et al. (Profitlich, 2008) evaluated ictal neuropsychological findings in six patients with focal convulsive SE based on formal neuropsychological evaluations and found that, although heterogeneous domains were affected between patients, some degree of impairment of consciousness and impairment of executive functions, higher-order functions such as speech and calculus, and emotional instability was found. The MoCA is used to evaluate orientation to time and place, language, attention, concentration, short-term memory and working memory, visuospatial abilities, and multiple aspects of executive functions, covering the main cognitive domains affected in absence status (Nasreddine et al., 2005; Profitlich, 2008). Moreover, it is a test we use routinely in our clinical practice, and from our extensive experience, we consider it an easy and practical tool.
Since it is impossible within a clinical setting to perform a formal and complete neuropsychological evaluation for all patients, we propose the MoCA as a tool for simple and fast cognitive assessment, in order to monitor patients’ clinical improvement.
Conclusion
Although it has not been validated in this context, the MoCA was a good method to evaluate clinical improvement in our patient with absence SE and showed a positive correlation with neurophysiological improvement.
Very limited conclusions can be extracted from a single case report, bringing the need for larger prospective studies to validate the use of cognitive tests to evaluate absence SE.
Disclosures
None of the authors have any conflict of interest to declare.