Epileptic Disorders
MENUEyelid myoclonia with absences related to epileptic negative myoclonus Volume 23, issue 6, December 2021
Eyelid myoclonia with absences (EMA) is an epileptic syndrome characterised by eyelid myoclonia with or without absences, eye closure-induced paroxysms, and photosensitivity [1]. Seizures develop between 2 and 14 years of age (peak: 6–8 years). The hallmark of the syndrome is eyelid myoclonia with rapid (4-5-Hz) myoclonic jerks of the eyelids that are brief (
Case study
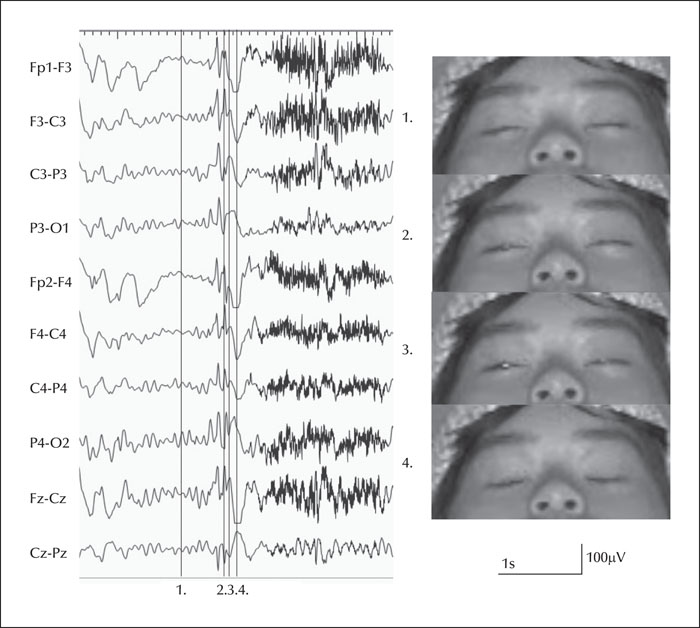
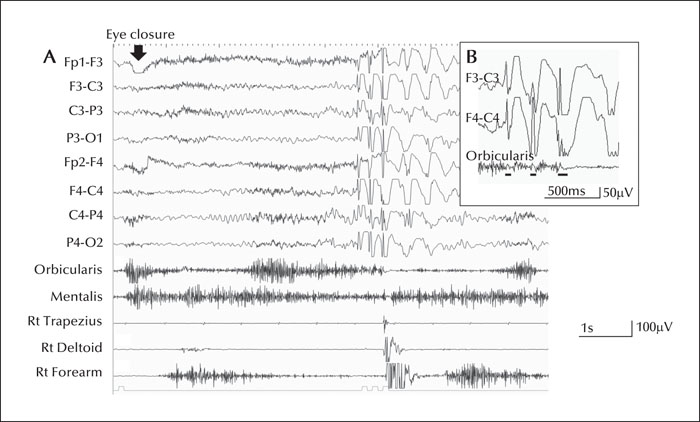
The female patient was born via normal delivery. There was no family history of epilepsy or any neurological disorders. At age six, she started exhibiting rapid fluttering of the eyelids when waking up from a sleeping state. These episodes occasionally accompanied a massive jerk of the shoulders and upper extremities and mild loss of consciousness. At age 10, she visited our clinic with chief complaints of a tick and brief reduction of consciousness. There were no abnormal neurological findings. EEG depicted an eye-opening seizure during eye closure, which was accompanied by diffuse polyspikes and waves (figure 1, video séquence 1). Simultaneous EEG-EMG recording demonstrated an eye closure-induced 3.0-4.5-Hz diffuse polyspike-and-wave complex accompanied by eye fluttering for 2–3 seconds after eye closure; this finding was compatible with the diagnosis of EMA (figure 2A). Eye fluttering was accompanied by generalised myoclonus (see video séquence 2). Upon replay of the EEG recording from 3 to 6 cm/seconds (figure 2B), EMG of the orbicularis oculi muscle depicted a cluster of brief interruption of tonic contraction with a duration of 60-140 mseconds, which was associated with the polyspike-and-wave complex. It was apparent that the brief decrease in tonus on EMG coincided with the negative component of the polyspike-and-wave discharge. Similar EEG findings were induced by photic stimulation (supplementary figure 1A). Furthermore, the relationship between spikes and decrease in tonus were confirmed by back averaging (supplementary figure 1B). Averaged spikes at the bilateral occipital area, with some extension to the central area, preceded the decrease in tonus of the orbicularis oculi muscle. Interestingly, it was noted that an eye closure-induced seizure was also evoked in total darkness, which is an atypical feature of EMA. These findings were not induced in other situations such as hyperventilation. Sleep EEG depicted a decrease in polyspikes and waves predominantly in the frontocentral areas. MRI and somatosensory evoked potential did not indicate any abnormalities. Based on the psychological test (WISC-IV), total IQ score was normal at 104, however, she had communication difficulties with a strange way of speaking.
After the diagnosis of EMA, she was started on clobazam, and the seizures disappeared in two weeks. However, due to drowsiness, clobazam was discontinued, and valproate acid was started from 600 mg/day to 1,200 mg/day, which effectively suppressed her seizures for two years. At age 13, seizures relapsed due to skipping medication, and EEG depicted eye closure-induced eyelid fluttering, as seen before. Add-on therapy with levetiracetam at 1,000 mg/day was effective, and her seizures resolved completely.
Discussion
EMA was first reported by Jeavons in 1977 as a separate type of epilepsy syndrome [2]. Jeavons initially reported that ‘Eyelid myoclonia and absences show a marked jerking of the eyelid immediately after eye closure and there is an associated brief spike-and-wave activity.’ EMA was originally recognised as myoclonic epilepsy rather than a primary absence epilepsy [3, 4]. To the best of our knowledge, no study has performed an EMG analysis of the orbicularis oculi muscle. The present study indicates that EMG involving the orbicularis oculi muscle may be useful for detecting ENM in some patients with EMA.
In the present case, the patient was diagnosed with ENM located in the orbicularis oculi muscle based on ictal EEG and EMG findings. ENM is defined as an interruption of tonic muscle activity for < 500 mseconds [5], which is time-locked to an epileptic EEG abnormality. The pathophysiology of ENM remains debatable, but a relationship with the frontal area of the brain has been reported, and enhanced inhibition of the primary motor cortex is suspected based on EEG findings [6]. Moreover, intracerebral electric stimulation of premotor, primary sensory, and supplementary motor areas may also evoke ENM [5].
Several recent studies have investigated the pathophysiology of EMA. Based on interictal EEG, about half of the patients showed spiky posterior-dominant alfa waves after eye closure, and ictal EEG frequently showed occipital-dominant ictal spikes preceding the generalised spikes and waves [7]. EEG network analysis using low-resolution brain electromagnetic tomography revealed an abnormal cortical activity in the frontal and occipital brain areas [8]. Studies using functional MRI revealed that eye closure sensitivity in EMA patients was accompanied by an increase in a blood oxygenation level-dependent signal within a complex circuit, encompassing the visual cortex, parietal cortex, thalamic pulvinar, and frontal lobe networks, involving the premotor area for eye closure control and the cingulate cortex for blinking movements [9]. Furthermore, the back averaging procedure in the present case demonstrated preceding bilateral occipital-dominant polyspikes extending to the central area before the decrease in tonus of the orbicularis oculi muscle. Together, these findings support the hypotheses that the occipital area is the generator and subsequent activity in the frontal area may induce eyelid myoclonus [3, 7].
Regarding seizure manifestation in EMA, eyelid fluttering or blinking of the eyelid is a prominent and unique symptom. In the literature, there are two types of eyelid fluttering in EMA [10]. One is accompanied by rapid eyelid fluttering with a sequence of 9-14-Hz polyspikes with intermixed rare slow waves, prominent over the frontal or parieto-occipital region on EEG without associated absences [4, 11]. The other type shows 3-6-Hz diffuse polyspikes and waves on EEG lasting for 1.5-6.0 seconds with/without upward eyeball deviations or absences [4]. The latter seizure type was concordant with the ictal EEG findings observed in the present case. The ictal EEG with diffuse polyspikes and waves is occasionally associated with massive myoclonic seizures [4, 10]. In addition, a few EMA patients reportedly exhibited atonic components in the arm and head, with an ictal EEG with diffuse polyspikes and waves [12]. Our patient showed ENM of the mentalis and orbicularis oculi muscles and a generalised myoclonic seizure at the same time with ictal EEG predominating in the fronto-central area or the occipital area. Therefore, eye fluttering seizures in our case may have involved the frontal lobe system, producing positive myoclonus and ENM, triggered by eye closure via the visual cortex, parietal cortex, and thalamic pulvinar. This eye closure-induced eyelid epileptic negative myoclonus may therefore be an intermediate between eyelid myoclonia and epileptic negative myoclonus.
Of interest, our patient exhibited eye closure-induced eyelid fluttering as a result of both light and total darkness, which is atypical for EMA. This was considered to be eye closure sensitivity, which was occasionally reported in generalised seizures such as EMA and juvenile myoclonic epilepsy [13]. Although this might be a characteristic of fixation-off [4], the duration of diffuse spikes is atypical on EEG, as the epileptic discharge usually persists for the entire duration of eye closure [14]. Nonetheless, further studies are needed to discriminate the frequency of each feature in EMA.
Our patient's seizures were controlled with a combination of valproate and levetiracetam, which has previously been reported to be effective [15]. However, because the patient is female, valproate will have to be withdrawn in the future due to its pregnancy-related complications.
In conclusion, we describe the first case of EMA with eye closure-induced eyelid blinking appearing as a cluster of ENM localized to the orbicularis oculi muscle. This case suggests that intermittent ENM during eye closure might be seen in some patients with EMA.
Supplementary material
Summary slides and supplementary figure accompanying the manuscript are available at www.epilepticdisorders.com.
Acknowledgements and disclosures
We are grateful to the patient and her family for their participation in this study.
None of the authors have any conflicts of interest to disclose.