Epileptic Disorders
MENUEvolution of concepts in epilepsy surgery Volume 21, issue 5, October 2019
The year 2019 is the 110th anniversary of the International League Against Epilepsy (ILAE), and these past 110 years have witnessed the evolution of surgical treatment for epilepsy from a rarely performed, last resort effort to its present place as standard of care for many patients with pharmaco-resistant seizures. At the time of the first ILAE meeting in Budapest, in September 1909, however, epilepsy surgery had already been accepted as alternative therapy in highly selected cases for several decades (see Engel, 1993a, 2005).
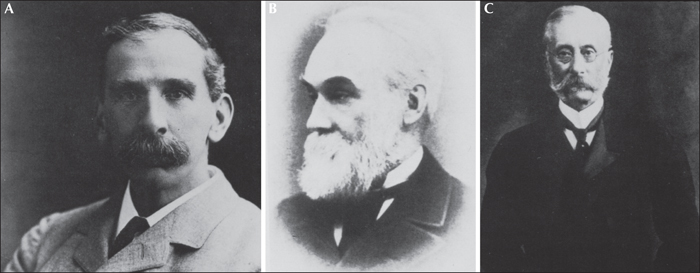
The modern era of epilepsy surgery is generally considered to date from the classic paper of Victor Horsley (figure 1A), published in the British medical journal in 1886 (Horsley, 1886), based on localizing information of ictal semiology determined by Johns Hughlings Jackson (figure 1B) from studies of pathological substrates (Jackson, 1880; Jackson and Colman, 1898; Taylor, 1958) and confirmed by David Ferrier (figure 1C) by stimulation of monkey brains (Ferrier, 1873, 1875, 1883). Horsley's paper described the successful surgical treatment of three patients with focal seizures operated on at London's National Hospital for the Paralysed and Epileptic at Queen Square, earlier that same year. Present in the operating theater for these landmark procedures were Jackson and Ferrier, who, with Horsley, represented neurosurgery, neurology, and clinical neurophysiology - the three disciplines still essential for epilepsy surgery today.
Early epilepsy surgery
Horsley's paper may have served to bring surgical treatment for epilepsy to the attention of mainstream neurologists and neurosurgeons, but was by no means the first surgical intervention designed to correct natural, rather than supernatural, causes of epilepsy. Arguably, the first report of successful surgical treatment of epilepsy was that of Benjamin Winslow Dudley in 1829, who reported five surgical procedures performed between 1818 and 1828 in Lexington, Kentucky, to correct palpable traumatic skull defects that were causing epileptic seizures (Dudley, 1828; Patchell et al., 1987). All five patients survived, three became seizure-free, and two had marked improvement. Dudley commented that similar results might not be possible in unhealthy urban environments that did not have the clean air of Kentucky.
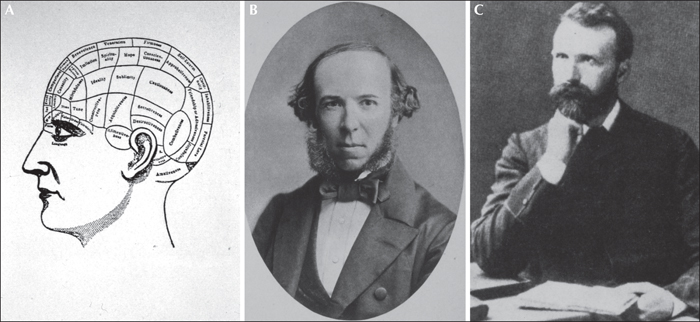
More scientific approaches to epilepsy surgery depended upon neurologists and neuroscientists who elucidated the localization of function in the brain. Franz Joseph Gall, who introduced phrenology (figure 2A) in Vienna at the turn of the 19th century (Gall, 1800), a system that claimed to diagnose personality traits by palpitation of bumps on the head, was so vehemently debunked by the scientific community that the concept of localization of function in the brain was rejected for decades. It was the British philosopher Herbert Spencer (figure 2B) who restored respectability to this view in 1855 with the statement that “localization of function is the law of all organizations whatever: separation of duty is universally accompanied with separateness of structure; and it would be marvelous were an exception to exist in the cerebral hemispheres” (Spencer, 1855). Pierre-Paul Broca (1861), a French surgeon, was the first to use neurological signs and symptoms to operate on an otherwise “invisible” cerebral lesion based on post mortem localization of motor language (Broca's area). An extradural abscess was resected from an aphasic patient; however, the patient died.
Spencer was a major influence on Jackson, who undertook the study of ictal semiology, and correlated these behaviors with structural lesions observed at autopsy (Jackson, 1880; Jackson and Colman, 1898; Taylor, 1958). The resultant maps of cerebral function were later used to localize invisible epileptogenic lesions in the brain. Numerous other prominent neurologists studied focal epileptiform dysfunction prior to Jackson (see Engel, 1993a, 2005), but did not make the connections documented in Jackson's work that eventually led to surgical treatment of epilepsy.
At the same time that Jackson was studying pathological substrates of focal ictal semiology in patients, basic scientists in Germany, Gustav Theodor Fritsch and Eduard Hitzig, were using faradic stimulation to map the function of dog motor cortex (Fritsch and Hitzig, 1870). In London, David Ferrier pursued this technique in several animal species including the monkey, and succeeded in reproducing the ictal behavior described by Jackson in patients (Ferrier, 1873, 1875, 1883). A footnote to this history is that the British anti-vivisectionists viciously attacked Ferrier for his research on monkeys, but it was a crucial confirmatory step in Horsley's decision to operate on the basis of initial ictal behavior. A more bizarre report is that of Robert Bartholow (1874), a Cincinnati physician, who stimulated the exposed motor cortex of his house servant who had a skull defect caused by cancer of the scalp. He was also severely criticized for his ethics.
The advent of antiseptic and anesthetic techniques in the mid to late 1800s made operations on the brain more commonplace in North America and Europe. As a result, William Macewen (figure 2C) was actually the first to publish resection of an invisible lesion to treat epilepsy, based on Jackson's approach to localization, in Glasgow in 1879 (Macewen, 1879). Removal of a frontal meningioma resulted in seizure freedom. Macewen then published a series of neurosurgical procedures in 1881 and 1888 that included several patients with epilepsy who were operated on using ictal semiology for localization, well before Horsley (Macewen, 1881, 1888). There is also evidence that other surgeons in England and in Italy may have performed epilepsy surgery prior to Horsley (see Engel, 1993a, 2005). The fact that Horsley generally receives credit for initiating the modern era of epilepsy surgery is likely a testament to the preeminence of Queen Square and the British Medical Journal in the English-speaking world.
Early epilepsy surgery and the ILAE
By the turn of the 20th century, surgical treatment for epilepsy remained a rarely performed procedure for carefully selected patients, and was most actively pursued by Feodor Krause (Krause, 1909; Krause and Heyman, 1914) in Berlin. At the first ILAE meeting in Budapest, in September 1909, held in association with the International Medical Congress, we have no documentation of specific titles of papers presented, but Macewen, Krause, and Horsley were all present, as was Harvey Cushing from Yale, one of the fathers of American neurosurgery (Shorvon et al., 2009). It is noted that not all of the papers presented related to epilepsy, but that Horsley was the signatory on a letter from the British anti-alcohol association urging members to refuse gift bottles of Tokay wine (Shorvon et al., 2009). At the third meeting of the ILAE in Zurich, in September 1912, held with the International Congress of Psychiatry and Psychology, there was a lecture on “New Experiences with Surgical Treatment in Epilepsy” by Kümmel (Shorvon et al., 2009). In the first series of Epilepsia, published between 1909 and 1915, there appeared to be no papers on surgical treatment for epilepsy.
Stimulation, X-Ray, and EEG
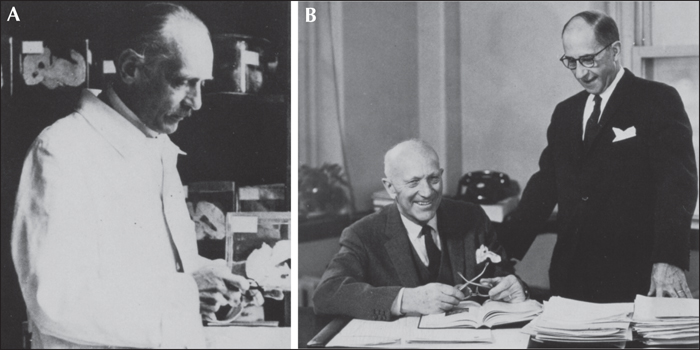
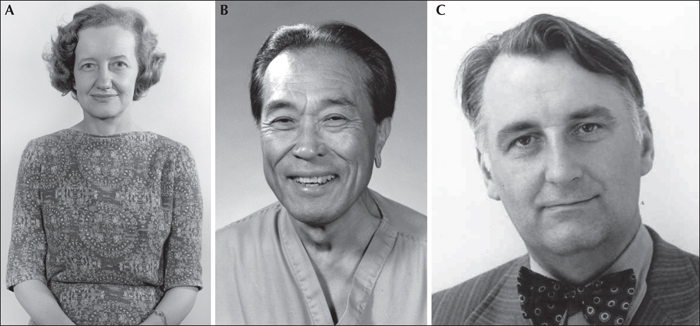
Feodor Krause (1909) and Otfrid Foerster (1925) (figure 3A) were early 20th century German neurosurgeons who used Jacksonian localization concepts and electrical stimulation to identify and resect epileptogenic lesions, although surgery was always primarily aimed at resecting visible cortical lesions. Foerster is perhaps most recognized for his famous pupil, Wilder Penfield (figure 3B), who carried this approach to epilepsy surgery to Canada, in 1928, and founded the Montreal Neurologic Institute in 1934. Penfield, and his collaborators, particularly Herbert Jasper (figure 3B), utilized intraoperative stimulation not only to localize the epileptogenic lesion, but also to create detailed maps of motor and sensory function in the human brain (Penfield and Jasper, 1954).
The development of roentgenographic techniques, specifically pneumoencephalography by Walter Dandy (Dandy, 1919), and cerebral angiography by Egas Moniz (Moniz, 1934), greatly enhanced the efficacy of lesion-directed epilepsy surgery in the early part of the 20th century, but the most important advancement of modern epilepsy surgery was the discovery of electroencephalography (EEG) by Hans Berger (figure 4A) in 1929 (Berger, 1929). As long ago as 1875, Richard Caton, a physiologist in Liverpool, had demonstrated that electrical activity could be recorded from the brains of animals (Caton, 1875), but when Berger, a psychiatrist, published his paper on human EEG, from Jena, Germany, it was largely met with incredulity. Not until the internationally renowned physiologist, Lord Adrian (Adrian and Matthews, 1934), demonstrated the alpha rhythm live, on stage, during a scientific meeting in 1934, did the medical community eventually accept Berger's discovery. EEG then rapidly gained importance in clinical neurology as the only objective non-invasive measure of brain function.
Prior to the midcentury, when focal neocortical resections of epileptogenic lesions were the common surgical procedures, a few neurologists and neurosurgeons pursued alternative approaches. Of the various interventions that have continued until today, corpus callosotomy was first performed by William van Wagenen and Yorke Herren in 1940 (Van Wagenen and Herren, 1940) in the United States, and hemispherectomy was first performed by Kenneth McKenzie in 1938 (McKenzie, 1938) in Canada. Because McKenzie did not fully publish his work, the credit for popularizing hemispherectomy belongs to Roland Krynauw of South Africa, who documented the effectiveness of this procedure in 1950 (Krynauw, 1950). Since then, several variations have been undertaken with disconnective hemispherotomy, the most common approach today (Binder and Schramm, 2008).
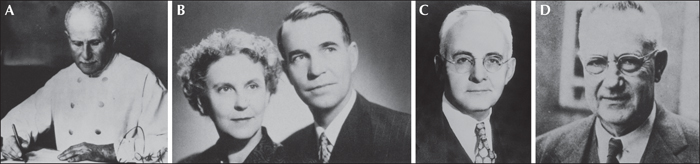
In 1938, pioneer electroencephalographers Frederic and Erna Gibbs (figure 4B), along with the most prominent early American epileptologist, William Lennox (figure 4C), first described EEG patterns that clearly distinguished three specific ictal events: grand mal, petit mal, and pyschomotor seizures (Gibbs et al., 1938). Because the Gibbs used only linked ears, these patterns were initially believed to be generalized until Herbert Jasper and John Kershman, in Montreal, used bipolar montages to demonstrate epileptiform abnormalities could be focal, and found location, as well as pattern, to be of diagnostic importance (Jasper and Kershman, 1941). They were the first to demonstrate the temporal localization of interictal and ictal epileptiform discharges in pyschomotor epilepsy.
Temporal lobe epilepsy
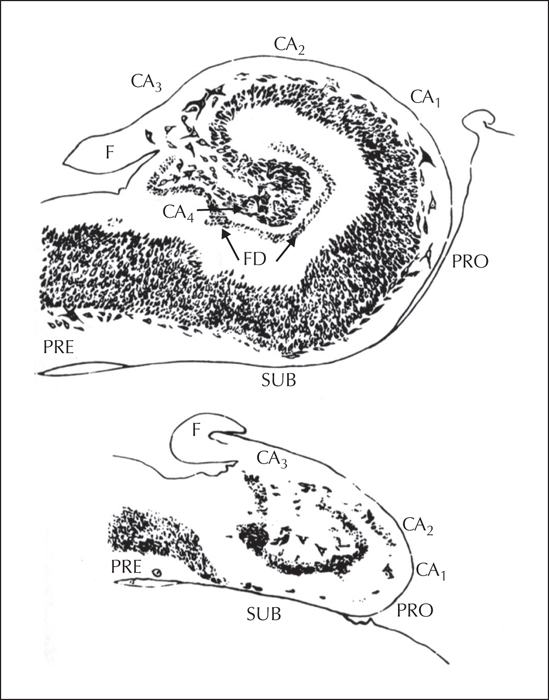
Ammon's horn sclerosis was first described by Bouchet and Cazauvielh in 1885 in Paris, as a common post mortem finding in patients with “mental alienation seizures” (Bouchet and Cazauvielh, 1825). Jackson determined, in the late 1890s, that epilepsy with an “intellectual aura” or “dreamy state” and “tasting movements” was associated with lesions in mesial temporal structures (Jackson, 1880). At about the same time, Sommer (Sommer, 1880) and Bratz (Bratz, 1899) in Germany, independently published papers on the cellular pathology of hippocampal sclerosis (figure 5). At the time, however, it was felt that these changes were the result, and not the cause of epilepsy, and that the hippocampus had nothing to do with epileptogenesis. Even though Jasper demonstrated, in a chapter in a textbook by Penfield and Erickson in 1941, on the basis of his electrophysiological studies, that pyschomotor seizures originated in the temporal lobe (Jasper, 1941), in that same textbook, Penfield stated that the origin of pyschomotor seizures is unknown and, with no evidence of a lesion, “any operative procedure is probably doomed to turn out to be a negative exploration” (Penfield and Erickson, 1941).
The lesion-directed approach to epilepsy surgery abruptly changed with the classic 1951 paper by Frederic Gibbs and Percival Bailey (figure 4D), a neurosurgeon in Chicago, reporting the first series of surgeries for epilepsy based on scalp EEG evidence alone (Bailey and Gibbs, 1951). It is ironic that the field turned on data presented by Frederic Gibbs, who strongly believed in linked ear references, while it was Jasper who promoted bipolar montages for optimal localization. Somehow, Gibbs was able to recognize interictal temporal epileptiform discharges in a series of patients with refractory pyschomotor seizures, and convinced Bailey to operate without evidence of a structural lesion. In 1950, Penfield and Flanigan had published a larger series of patients who underwent temporal lobe resections for epilepsy based on the presence of lesions (Penfield and Flanigin, 1950), and a year later, Jasper and colleagues (Jasper et al., 1951) published the complete electrophysiological findings of these patients, again confirming temporal localization of interictal epileptiform EEG changes. After these unequivocal demonstrations that EEG activity could reliably localize the epileptogenic region in the most common form of drug-resistant epilepsy, there was a modest explosion in surgeries for temporal lobe epilepsy in Europe, the United States, and even Cuba (see Engel, 1993a, 2005). For most of the medical community, however, epilepsy surgery remained experimental and, as such, was banned for several decades after WWII in Germany and Japan.
An interesting aspect of surgical treatment is that the early surgeons, including Bailey and Penfield, did not remove the hippocampus, for fear of serious behavioral consequences. It's not clear how and when the removal of the hippocampus began, but the first documented report is by Arthur A. Morris of Phoenix, Arizona, who presented a series of five patients at a meeting in Washington, D.C. in 1950 (Morris, 1950, 1956). It has been suggested that, had it not been for the placebo effect of the early temporal lobe surgery series, epilepsy surgery might not have been pursued. In any event, once it was demonstrated that it was safe to remove the hippocampus and para-hippocampal structures, which Jasper had in fact already demonstrated to be involved in the ictal event (Jasper et al., 1951), modern anteromesial-temporal resections were performed with much better outcomes. Bilateral hippocampal resection, on the other hand, as performed on the patient known as H.M., by Scoville in 1953, resulted in global amnesia (Eichenbaum, 2013).
Midcentury epilepsy surgery and the ILAE
There were no further lectures given on epilepsy surgery at ILAE meetings until the 7th Congress in Paris in association with the EEG Society in 1949. At this meeting, Jasper gave a paper on EEG in neurosurgery, and Earl Walker gave a paper on surgical treatment of epilepsy. At the 8th International Congress held in Lisbon in September 1953, there was a full-day workshop organized by Henri Gastaut on temporal lobe epilepsy with several papers on surgical treatment. In the second series of Epilepsia, 1937-1950, there were only scattered reports of surgical treatment, entirely referring to procedures other than resection of an epileptogenic lesion. The third series of Epilepsia, 1952-1955, contained only one major paper on epilepsy surgery, “The Surgical Treatment of ‘Focal’ Epilepsy: An Inquiry into Current Premises, Their Implementation, and the Criteria Employed in Reporting Results” by Russell Meyers of Iowa City (Meyers, 1954). In this extensive report of his surgical experiences from 1936 to 1942, Meyers listed the first purpose of his paper “to record the generally disappointing character of the results obtained in the author's series of cases of ‘focal’ epilepsy subjected during a 15-year period to extirpation of cortical regions regarded as epileptogenous zones”. These were all neocortical resections localized primarily by seizure semiology and visible lesions, but with ancillary information from pneumo-encephalography, angiography, and as early as 1938, single-channel intraoperative EEG evolving into multichannel EEG. Eleven percent of patients were seizure-free after five years, 53% were unimproved, and 12% died, 6% due to operative mortality. With this as the sole published report on epilepsy surgery in Epilepsia, over the three years of the second series, it is somewhat surprising that the practice continued. There was, however, another major paper on “So-called ‘Pyschomotor’ Temporal Epilepsy: A Critical Study” by Henri Gastaut of Marseille, France, which included a slightly more optimistic discussion of surgery (Gastaut, 1953). Each year also included a bibliography of the world's literature on epilepsy, including papers on surgical treatment. In 1951 there were 18, in 1952 there were 15, in 1953 there were 24, and in 1954 there were 18. Although surgery was now being done at several centers, few programs published their results.
Temporal lobe epilepsy (continued)
With the focus on temporal lobe epilepsy, Murray Falconer (figure 6A), in 1953, working at Guy's Hospital in London, introduced a standardized en bloc anterior temporal lobe resection that provided intact specimens for pathologists to examine. This revealed that a high percentage of patients had hippocampal sclerosis, and that this lesion predicted a good surgical outcome (Falconer, 1953). Although the concept that hippocampal sclerosis could result from epileptic seizures persisted, and in some patients it was attributed to febrile convulsions in early childhood, Falconer's work convinced most epileptologists that hippocampal sclerosis was also a cause of temporal lobe epilepsy (Falconer, 1974).
With attention increasingly directed at identifying a unilateral mesial temporal epileptogenic region, various non-invasive EEG techniques were introduced, such as naso-pharyngeal, tympanic, and sphenoidal electrodes (see Engel, 1993a, 2005). As the most reliable recordings were those obtained directly from the brain during surgery, EEGers began to pursue approaches to record directly from the brain extraoperatively. The first reported extraoperative depth electrode recording was carried out by Reginald Bickford and Hugh Cairns at Oxford in 1944, when they inserted multi-stranded insulated wires into a cerebral bullet track. Bickford later was the first to record from extraoperative depth electrodes, inserted freehand through the skull, at the Mayo Clinic (Bickford et al., 1953). Stereotactic depth electrode recordings (stereo EEG; SEEG), however, as used today, were initially introduced in Paris by Jean Talairach (figure 6B) and Jean Bancaud (figure 6C) in the late 1950s (Talairach et al., 1958). Because French law only permitted electrodes to remain in place for several hours, localization with this SEEG technique was based on interictal spike activity, as well as ictal activity induced by electrical stimulation and convulsant drugs.
Long-term chronic depth electrode recording was first practiced by Paul Crandall (figure 6D) and colleagues at the University of California, Los Angeles (UCLA), in the early 1960s (Crandall et al., 1963), where electrodes were kept in place for days or weeks if necessary to capture spontaneous ictal events. Crandall combined this approach with Falconer's en bloc resection, permitting detailed electrophysiological correlations with pathological evaluation of resected tissue. Not only did he describe the interictal and ictal electrographic changes associated with hippocampal sclerosis, but with a number of basic scientists, also carried out microelectrode recordings to elucidate microcircuitry, and unit activity, in epileptogenic mesial temporal structures (Babb and Crandall, 1976). This investigative approach has become the foundation of multidisciplinary collaborative research on fundamental mechanisms of human brain function, including epilepsy, carried out early in Paris by Bancaud and Paul Buser (Kahane et al., 2008), and in many other epilepsy surgery programs today.
Crandall also deserves credit for being the first to use EEG telemetry to facilitate ictal recordings. In the 1950s, Ross Adey, a neurophysiologist at UCLA, developed an EEG telemetry system to record from chimpanzees orbiting the Earth as part of the U.S. space program. With Richard Walter, Crandall recognized the potential of this technique to carry out continuous EEG recordings over long periods of time. His electronics engineer, Anthony Dymond, subsequently built the first EEG telemetry unit (Dymond et al., 1971). This was only possible at the time with depth electrodes, which permitted ictal recordings relatively free of muscle artifact. Dymond subsequently founded BioMedical Sciences, the first manufacturer of commercial EEG telemetry equipment, which was eventually sold to Nicolet.
EEG telemetry for presurgical evaluation was accompanied by photography, then cinematography, and finally video for simultaneously monitoring of behavior and second by second electroclinical correlations of ictal onset and propagation (see Engel, 1993a, 2005). With advances in EEG technology that permitted improved artifact reduction, video EEG telemetry was later performed with scalp and often sphenoidal electrodes permitting non-invasive long-term monitoring for presurgical evaluation (Engel et al., 1981; Gotman et al., 1985).
During the 1970s and 80s, several distinct, different approaches arose for the use of invasive EEG in presurgical evaluation (see Engel, 1993a, 2005). One approach continued to rely heavily on intraoperative electrocorticography as originally practiced by Penfield and Jasper, often preceded by non-invasive video-EEG using scalp, and perhaps sphenoidal, electrodes. Other approaches utilized extraoperative invasive EEG recording. The Crandall approach employed somewhat standardized bilateral depth electrode placements designed to sample the structures known to be involved in the initiation and propagation of limbic seizures, while disciples of the Paris group developed a more intricate SEEG approach to provide a predominantly unilateral three-dimensional survey tailored to a variety of potential epileptogenic lesions involving mesio-temporal and neocortical structures (see Engel et al., 2019). A third approach initially involved the introduction of epidural grid electrodes applied over the surface of the brain by Sidney Goldring in St. Louis (Goldring et al., 1987) which evolved into subdural grid and strip electrodes, strongly promoted by the Cleveland Clinic (Lüders et al., 1987). Strips could be inserted bilaterally through burr holes, but grids were generally placed unilaterally, requiring a hemicraniectomy. As these techniques were all designed not only to identify the site of ictal onset, but also to either determine the boundaries of the epileptogenic region, or to justify a standardized anteromesial temporal resections (Spencer et al., 1984), subsequent intraoperative corticography and functional mapping was often not necessary.
Neuroimaging
Although extensive electroclinical correlations, particularly using video-EEG telemetry, became the mainstay of presurgical evaluation, identification of a structural lesion indirectly implied by radiological studies, and direct observation at surgery, remained important. The advent of computerized imaging, however, beginning in the late 1970s, moved epilepsy surgery back towards a lesion-directed strategy, with EEG assuming a more confirmatory role. X-ray computed tomography (CT) was the first approach that permitted visualization of the entire brain in three dimensions. The ability of this technique to reveal localized structural lesions in many patients with focal epilepsy greatly improved the selection of patients for surgery (Gastaut and Gastaut, 1976). The subsequent development of magnetic resonance imaging (MRI), with much improved resolution of structural lesions that might be epileptogenic, permitted identification of more discreet abnormalities than could be identified pre-operatively previously. Early MRI, however, was not able to convincingly identify hippocampal sclerosis, the most common “invisible lesion” encountered in surgical candidates, until the 1990s (Jackson et al., 1994). The first computerized neuroimaging technique to play a major role in the presurgical evaluation for temporal lobe epilepsy, therefore, was positron emission tomography (PET) with 18 F-fludeoxyglucose (FDG), which measures local cerebral glucose metabolism. A series of studies demonstrated that patients with mesial temporal lobe epilepsy had unilateral temporal hypometabolism, highly indicative of the presence of hippocampal sclerosis (Engel et al., 1982a, 1982b, 1982c). Consequently, a characteristic basilar temporal ictal onset on EEG, coupled with ipsilateral temporal hypometabolism, and appropriate ictal semiology, in the absence of other confounding factors, was sufficient to consider standardized temporal resection even if MRI was negative (Risinger et al., 1989; Engel et al., 1990).
FDG-PET also played an important role in the increasing application of epilepsy surgery to the pediatric population, initially through its ability to identify large unilateral areas of cortical dysplasia in infants and small children with apparent refractory secondary generalized epilepsy and a negative MRI (Chugani et al., 1988). This work led to the realization that some so-called catastrophic epilepsies of early childhood that appeared to be generalized could be due to focal lesions that would respond to localized surgical resection (Mathern et al., 1999). These lesions were eventually also demonstrated with higher resolution MRI (Sankar et al., 1995), which increased interest in pursuing surgical treatment for drug-resistant epilepsy in the pediatric population. PET remains an important part of presurgical evaluation, and the search continues for new ligands to supplement FDG, for instance one for a translocator protein (TSPO) that images neuroinflammation (Dickstein et al., 2019).
Other functional imaging approaches have also been introduced such as PET with flumazenil, a benzodiazepine receptor ligand (Savic et al., 1988), and alpha-methyl-tryptophan (AMT) (Chugani et al., 1998), which has been used in patients with tuberous sclerosis and multiple tubers, as only the tuber-causing spontaneous seizures appear to take up AMT. These approaches, however, are not in general use. Single-photon emission computed tomography (SPECT) measures cerebral perfusion but decreased perfusion is not as reliable for localizing the epileptogenic region as decreased metabolism with FDG-PET. Focally increased perfusion with ictal SPECT, compared to an interictal study, is a better indicator of the site of seizure onset, and approaches such as subtraction ictal single-photon CT co-registered to MRI (SISCOM), where the difference between ictal and interictal SPECT studies are superimposed on MRI, have become useful adjuncts to the presurgical evaluation in some patients (O’Brien et al., 1998).
Functional MRI (fMRI) measures natural differences in magnetic properties between oxygenated and deoxygenated hemoglobin to localize activity-related changes in cerebral blood flow with high spatial resolution and second to millisecond temporal resolution. This technique was correlated with EEG to confirm localization of interictal spike discharges and identification of the epileptogenic zone (Warach et al., 1996; Krakow et al., 1999). Although not an imaging technique per se, magnetoencephalography (MEG), superimposed on MRI, has become a highly useful additional tool for localizing interictal EEG spikes, and occasionally ictal onsets (Ebersole et al., 2008). Source localization is also possible with EEG, and may benefit from the use of high-density EEG (HDEEG) (Plummer et al., 2019). The accuracy of dipole source localization remains limited by a number of factors; however, many centers are relying on these techniques to help determine where depth electrodes ought to be targeted, and occasionally to avoid invasive studies altogether.
Behavioral evaluations
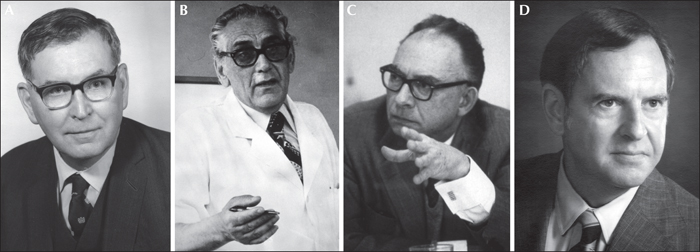
Neurocognitive testing is the third leg of the three-legged stool of presurgical evaluation (Wilson and Engel, 2010). Brenda Milner (figure 7A), working with Penfield at the Montreal Neurological Institute, initially described the material-specific functions of the left and right temporal lobes, which became the foundation for the neuropsychological test batteries that are used to identify focal-cortical dysfunction to support localization of the epileptogenic region (Milner, 1958). Extraoperative determination of hemispheric dominance for language was first demonstrated by Juhn Wada (figure 7B), in Japan, in 1949 (Wada, 1949), who anesthetized half of the forebrain by injecting sodium amobarbital into one carotid artery. The intracarotid amobartibal procedure, also referred to as the Wada test, was not known or accepted in the West, however, until Wada moved to the MNI and published his results from there in 1960 (Wada and Rasmussen, 1960). The Wada test was subsequently modified to permit independent evaluation of memory function of the dominant and non-dominant mesial temporal structures, not only to support localization of the epileptogenic region, but to predict the risk of global amnesia following anteromesial temporal resection (Milner et al., 1962; Klove et al., 1969).
As noted earlier, intraoperative mapping of cortical function by Penfield and Jasper (Penfield and Jasper, 1954) contributed importantly to our understanding of localization of function in the human cortex. Surgery in the mid-20th century was often performed under local anesthesia so that functional mapping could be carried out in order to avoid damage to essential cortical areas during resection of the epileptogenic region. With the advent of chronic subdural grid electrodes and SEEG, it later became possible to carry out functional mapping extraoperatively without the stresses and time limitations introduced by the acute intraoperative setting. Today, motor, sensory, and language areas can also be mapped with functional imaging such as PET, MEG, and most commonly by fMRI (see Engel, 1993a, 2005).
Until the late 20th century, epileptologists were almost all psychiatrists in the United Kingdom, several of the Commonwealth countries, Japan, and elsewhere. This reflected the 19th and early 20th century view that epilepsy was a psychiatric disorder. As a result, British psychiatrists have made important contributions to presurgical evaluation, and particularly, to assessment of post-operative outcome. David Taylor (figure 7C) was the first to publish a comprehensive assessment of surgical outcome when he interviewed 100 patients operated on by Falconer, actually visiting their homes and assessing the impact of seizure freedom or reduction on their life (Falconer and Taylor, 1968). Taylor pointed out that people with epilepsy seek treatment not only to eliminate their epileptic seizures, but to relieve the predicament caused by these recurrent ictal events (Taylor, 1993). He emphasized the need to listen to patients’ reasons for wanting surgical treatment, and to ensure realistic expectations as part of the decision-making process. The work of Taylor and others concerned with the psychological and social consequences of epilepsy led directly to the eventual development, at the end of the 20th century, of quantitative measures of health-related quality of life, specifically adapted to evaluate the results of surgical interventions (Vickrey et al., 1992; Devinsky et al., 1995). Consequently, neuropsychologists, psychiatrists, and health-outcomes researchers have become essential contributors to epilepsy surgery programs today.
Creation of an international epilepsy surgery community
Not only did epilepsy surgery programs around the world rarely publish their protocols or results, but there was also very little exchange among them. The first attempt to create a forum for such an exchange was the establishment of the Temporal Lobe Club at the annual meeting of the American Epilepsy Society in 1981. It and subsequent annual meetings were sufficiently well attended to justify a grant from the U.S. National Institute of Neurological Disorders and Stroke (NINDS), as well as the American ILAE chapter and several pharmaceutical companies, to support the first Palm Desert Conference on Surgical Treatment of the Epilepsies held in 1986 (Engel, 1987a). Representatives attended from 53 epilepsy surgery programs in 17 countries, representing essentially all active epilepsy centers offering surgery as an alternative treatment at the time. The charge of admission to the conference was data from each epilepsy surgery program in a relatively uniform format which, despite the diverse approaches, revealed consistent results for the most commonly performed procedures (Engel, 1987b; 1993c) (table 1).
Epilepsy surgery programs at the time generally preferred a single approach to presurgical evaluation, depending on their lineage. Disciples of Penfield and Jasper, further popularized at the University of Washington, carried out tailored resections based largely on extensive intraoperative electrocorticography, including functional mapping. Programs that derived from the Paris school, practiced predominantly in France and Italy, tailored resections based predominantly on extraoperative SEEG evaluations, with the exception of Zurich, where only amygdala-hippocampectomies were performed (Wieser and Yasargil, 1982). Surgeons who trained with Falconer in London performed standardized en bloc anterior temporal resections in most patients, based on the results of interictal non-invasive EEG recordings and X-ray studies. Although intraoperative electrocorticography was performed, Falconer rarely used these data to alter the temporal resections (Engel et al., 1975). Followers of the UCLA school also performed standardized en bloc anterior temporal lobe resections, but these were based on relatively standardized bilateral chronic depth electrode recordings designed specifically to localize ictal onset and propagation from mesial temporal structures. Later, before the Palm Desert meeting, the UCLA protocol came to rely more heavily on scalp and sphenoidal video-EEG telemetry combined with FDG-PET, and other tests of focal functional deficit (Engel et al., 1981). And other centers began using scalp and sphenoidal video-EEG telemetry as well (Gotman et al., 1985). At Yale, chronic depth electrode recordings continued to be performed on all patients prior to surgery. At the Cleveland Clinic and centers influenced by their approach, tailored resections were based on chronic subdural grid and strip recordings (Lüders et al., 1987). Results of clinical pathological correlations were beginning to emerge from centers who performed en bloc resections, but it could not be obtained where the epileptogenic region was removed by suction.
A major conclusion reached during the deliberations of the first Palm Desert conference was the agreement that none of these approaches was essentially better than another, but each had advantages and disadvantages that made it preferable for certain types of epilepsy and less useful for others. As a result, between the first and second Palm Desert conference, held in 1992 (Engel, 1993b), most epilepsy surgery programs began to also adopt approaches used at other centers for specific purposes. Chronic invasive recordings began to be limited only to patients with particular problems that could not be resolved non-invasively, while those centers that never performed chronic invasive recordings began to do so when indicated. Most centers agreed that some form of depth electrode protocol was necessary for mesial temporal lobe epilepsy and other conditions where three-dimensional evaluation was necessary, and reserved subdural grid and strip electrodes for focal neocortical epilepsy where a tailored resection required not only the localization of the epileptogenic region, but determination of its extent, perhaps including functional mapping.
The first Palm Desert conference coincided with the beginning of application of MRI and PET to presurgical evaluation, a sea change that moved the field back to lesion-directed presurgical evaluation. This was another important topic for discussion, and subsequent universal collaboration on the application of these new diagnostic technologies. Neuropsychologists also began to exchange information on the use and interpretation of various neurocognitive batteries and the intracarotid amobartibal procedure. Finally, a standardized classification for surgical outcome with respect to epileptic seizures was agreed on and continues to be used today (Engel, 1987c; Engel et al., 1993).
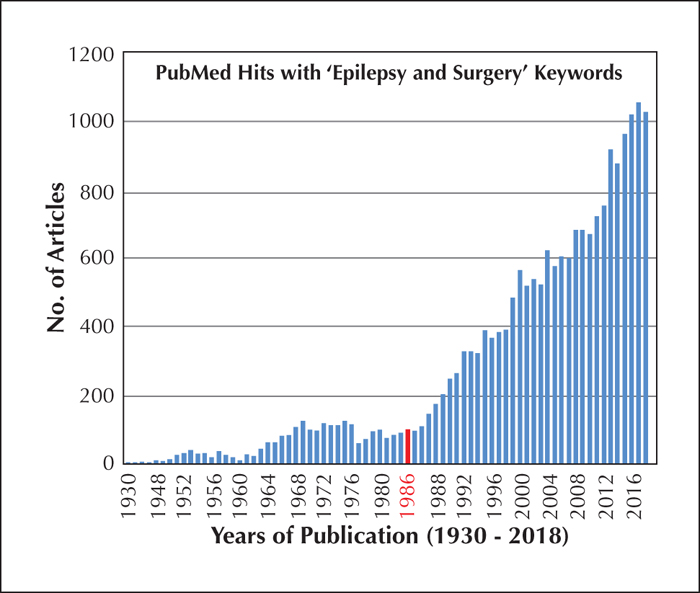
The date of the first Palm Desert conference also coincided with a marked increase in the number of publications on epilepsy surgery (figure 8) and the establishment of many new epilepsy surgery programs. One important result of the increasing interest in surgical treatment for epilepsy as far as the ILAE is concerned, was the establishment of the first Commission on Neurosurgery during the 1985-89 term with Arthur Ward as chair. Major activity of this new commission, however, did not begin until the 1989-93 term with Hans Gregor Wieser and Herbert Silfvenius as co-chairs. Important contributions of this Commission were a report on epilepsy surgery in developing countries (Wieser and Silfvenius, 2000), an alternative outcome classification for surgery (Wieser et al., 2001), and a white paper on mesial temporal lobe epilepsy with hippocampal sclerosis (Wieser et al., 2004). In the decade between 1989 and 1999, epilepsy surgery was one of the major topics in four of the five International Epilepsy Congresses.
The second Palm Desert Conference on Surgical Treatment of the Epilepsies, again sponsored by NINDS and the American ILAE chapter, was held in 1992 and documented the tremendous progress made between 1985-90 (Engel, 1993b). Reflecting the marked increase in the number of epilepsy centers, this conference was attended by representatives from 118 surgery centers in 25 countries, essentially a doubling in the number of active epilepsy programs in six years. Each center again brought its data, which demonstrated marked improvements in outcome for temporal lobe resections, and also neocortical resections, when a lesion was present on imaging (Engel, 1993c) (table 1). An increase in the number of hemispherectomies and corpus callosotomies performed was not accompanied by improved outcome, presumably because more difficult patients were being selected for surgery.
Two conceptual advances can be attributed to discussions at the second Palm Desert conference. The first was the recognition of the concept of surgically remediable epilepsy syndromes (Engel, 1996). Given that the number of antiseizure drugs was increasing to the point where it would take years, and perhaps a lifetime, to prove medical intractability, it was no longer reasonable to consider surgery for epilepsy as treatment of last resort. Rather, early surgery was recommended for specific surgically remediable epilepsy syndromes with well known pathological substrates and a natural history categorized by medical refractoriness after failure of a few appropriate drug trials, but a reasonably high probability of complete control of disabling seizures with surgery. Mesial temporal lobe epilepsy with hippocampal sclerosis was the prototype of a surgically remediable syndrome. The second advance was a clear description of the various functional and structural anatomical zones evaluated during presurgical evaluation: the irritative zone, the area of cortex that generates interictal spikes; the ictal onset zone, the area of cortex where seizures are generated; the epileptogenic lesion, the structural abnormality of the brain that is the direct cause of the epileptic seizures; the symptomatogenic zone, the portion of the brain that produces the initial clinical symptomatology; the functional deficit zone, the cortical area of non-epileptic dysfunction measured by a neurological examination, neuropsychological testing, non-epileptiform EEG, and PET; and the epileptogenic zone, a theoretical construct derived from all the other tests, constituting the area of brain that is necessary and sufficient for initiating seizures, the removal or disconnection of which is the minimum procedure necessary for abolition of seizures (Lüders et al., 1993).
An important development since the second Palm Desert conference has been the increasing application of epilepsy surgery to infants and very young. An international epilepsy surgery symposium held in Bielefeld, Germany, in 1995 was devoted entirely to pediatric epilepsy surgery, resulting in a book on this topic (Tuxhorn et al., 1997). The ILAE then formed a pediatric epilepsy surgery sub-commission in 1998 with the aim of formulating minimal standards for epilepsy surgery in childhood. The intent was also to evaluate the role of palliative procedures, such as corpus callosotomy, multiple subpial transection, and vagus nerve stimulation, in pediatric epilepsy.
21st century advances and challenges
The field of epilepsy surgery has continued to progress in the 21st century with respect to the presurgical evaluation, the surgical procedures offered, and the eligible patient population (Vakharia et al., 2018). This progress was particularly characterized by increasing application of epilepsy surgery to the pediatric patient population, as evidence by several consensus conferences and a textbook (Arzimanoglou et al., 2016). These works all emphasize, as with the adult population, that the key to optimal outcome in children is early appropriate recognition of possible surgical candidates and timely referral. A major contribution was the official ILAE definition of drug-resistant epilepsy as failure of two appropriate drug trials (Kwan et al., 2010), which supplemented the concept of surgically remedial syndromes to facilitate early referral of potential surgical candidates. With respect to presurgical evaluation, non-invasive ictal EEG recordings remain a standard of care, although cogent arguments have been made that ictal recordings may not always be necessary, particularly in countries with limited resources, when interictal EEG, imaging, seizure semiology, and other studies point clearly to a unilateral resectable epileptogenic region (Alvim et al., 2018). When invasive recording is considered necessary, the trend towards utilizing different approaches for different suspected epileptogenic regions, that prevailed after the second Palm Desert conference, has gradually been reversed. This is particularly true in the United States where many of the newly established epilepsy surgery centers depend entirely on subdural grid and strip electrodes, while many European centers continue to use SEEG exclusively (see Engel et al., 2019). More recently, however, SEEG has begun to gain greater popularity beyond southern Europe (Vakharia et al., 2018).
Since the discovery that pathological high-frequency oscillations (pHFOs) recorded directly from the brain appear to identify areas capable of generating spontaneous seizures (Bragin et al., 1999), there has been increasing interest in using these EEG events to localize the epileptogenic region for surgery. HFOs in the frequency range of 80-250 Hz, termed ripples, occur normally in mesial temporal structures, reflect summated inhibitory post-synaptic potentials (IPSPs) that synchronize neuronal activity, and facilitate information transfer (Ylinen et al., 1995). Higher-frequency oscillations, up to 600 Hz, termed fast ripples, are pathological in these structures, and are believed to reflect summated action potentials of synchronously bursting neurons, which characterize epileptogenic tissue (Staba and Bragin, 2011). Further studies have confirmed that some ripple frequency oscillations are also pathological, while HFOs in the fast-ripple range can be physiological, especially in specialized areas of neocortex (Engel et al., 2009). Distinction between pathological and physiological HFOs, therefore, cannot be made solely on the basis of frequency. Whereas most of these early studies were done in animals and patients utilizing microelectrodes, evidence is mounting from patient recordings utilizing clinical depth and subdural electrodes that ripple frequency as well as fast ripple frequency HFOs are useful for identifying the epileptogenic region for surgery (Frauscher et al., 2017; Jiruska et al., 2017). Not only do studies show that these EEG events are more reliable than interictal spikes, but that they may even be more reliable than ictal onsets (Jacobs et al., 2008, 2010).
Whereas most of the early clinical studies of HFOs were carried out during chronic invasive in-patient monitoring, more recent studies have investigated the utility of HFO recording during intraoperative electrocardiography (ECoG). These studies indicate that removal of HFOs that persist following resection is more important than removal of areas that generate HFOs prior to resection (Van ‘t Klooster et al., 2017). Attention now is also being directed towards non-invasive localization of HFOs, and there is evidence that these events can be recorded with scalp EEG (Andrade-Valenca et al., 2011) and MEG (Tamilia et al., 2017; Van Klink et al., 2017). There continues to be debate regarding distinctions between pathological and physiological HFOs, and their value for localizing the epileptogenic region for surgery remains experimental; however, modern EEG telemetry equipment vendors are now all offering sampling rates sufficient to record HFOs. Data are being acquired at many centers around the world that promise to greatly increase opportunities for this unique epileptiform abnormality to be an important diagnostic biomarker for surgery in the future.
In addition to continuing important advances in the use of structural MRI, such as the use of 7 Tesla, innovative post-processing, and diffusion tensor imaging (DTI) (Vakharia et al., 2017; Bernasconi et al., 2019), there is also increasing interest in fMRI. This imaging technique was initially used to delineate the anatomical localization of interictal spikes, but there was also hope it could distinguish spikes generated in the epileptogenic region from those generated elsewhere or propagated (Gotman and Pittau, 2011). More recently, however, there has been increasing interest in connectomics, the study of neuronal networks, including networks responsible for epileptogenesis and ictogenesis (Engel et al., 2013; Tavakol et al., 2019). The technique of resting fMRI (rfMRI) is now being used to identify a variety of networks using independent component analysis or seed-based region of interest analysis. The first to be identified was the default-mode network (DMN) which is present during the resting state, but a large number of other networks relating to specific brain functions have now been identified (Bartolomei et al., 2017; Sinha et al., 2017). These may eventually have value in localizing functional disturbances associated with the epileptogenic region. rfMRI was felt to have such a high potential for epilepsy diagnosis that, early in the 2000s, the image of the brain used as the logo for the American Epilepsy Society replaced the anatomical detail with nodes and edges, the symbols used to delineate networks revealed by rfMRI. This potential, however, has yet to be fully realized.
Two other novel imaging technologies developed at the end of the last century are magnetic resonance spectroscopy (MRS) (Petroff and Duncan, 2008) and optical imaging (Haglund et al., 2008). MRS can be used to localize disturbances in a variety of metabolic processes, with a temporal resolution of a few minutes, better than PET, but not as good as fMRI. Optical imaging is an invasive technique that measures alterations in light passing through the brain, mediated by changes in neuronal activity. Optical imaging has been used to visualize the onset and propagation of ictal activity along the neocortex, and efforts are undertaken to perform optical imaging through the skull. To date, however, neither of these techniques have yet realized a practical role in presurgical evaluation.
With respect to surgery itself, the introduction of numerous technical advances during the last century have greatly improved the safety and efficacy of resective surgery for epilepsy, but recent attention has focused on novel procedures that would not only improve surgical results, but increase the population of patients who might benefit from surgical intervention. Multiple subpial transection (MST) was introduced at the end of the last century to treat epileptogenic regions in eloquent cortex that could not be resected (Morrell et al., 1989). Transection of neocortex perpendicular to the surface is designed to disconnect cortico-cortical fibers responsible for lateral spread of epileptic activity, while leaving cortical columns functionally intact. MST was applied to epileptogenic regions in language and motor cortex and initially appeared to be effective; however, this procedure has fallen out of favor due to late reoccurrence of seizures (Polkey and Smith, 2008). Other surgical approaches for patients who are not candidates for standardized resective surgery have utilized neuromodulation. In addition to vagus nerve stimulation (VNS), which employs external continuous stimulation of the vagus nerve to reduce seizure frequency and severity (Schachter and Boon, 2008), for decades there has been interest in direct stimulation of the brain to achieve a similar, and perhaps more robust, palliative effect (Velasco et al., 1987). This eventually led to a randomized controlled trial of continuous deep brain stimulation (DBS) of the anterior thalamus in 2010 (Fisher et al., 2010), demonstrating sufficient efficacy to warrant approval in Europe, and eventually the United States in 2018. A more effective palliative stimulation approach is closed loop response neurostimulation (RNS), which makes use of a small computer inserted in the skull, attached to electrodes in contact with the epileptogenic region. These electrodes are used to identify the onset of a seizure, and stimulate to abort it. In 2011, a randomized controlled trial demonstrated the efficacy of this technique for well-defined epileptogenic regions which cannot be removed, either because they involve essential cortical areas, or are bilateral (Morrell et al., 2011). Although RNS is palliative and very few patients become seizure-free, it has greatly extended the population of patients who can benefit from surgical intervention.
Various techniques designed to locally ablate, rather than resect, small epileptogenic regions have been proposed since the beginning of modern epilepsy surgery and a popular approach at the end of the last century was stereotactic radiosurgery through the intact skull, termed gamma knife surgery (GKS) (Regis et al., 1995). An advantage of this procedure is that it does not require breaching the skull, but a disadvantage is that the resultant lesion, when effective, often requires a year or more to take effect. A randomized controlled trial comparing GKS with open surgery for mesial temporal lobe epilepsy in 2018 did not support its continued use except in patients with medical contraindications to craniotomy (Barbaro et al., 2018). Radiofrequency thermal ablation with electrodes placed for presurgical SEEG evaluations are sometimes used in Europe in lieu of open surgery (Dimova et al., 2017), however, laser interstitial thermal therapy (LITT), utilizing laser thermal ablation via a fiber probe inserted through a twist drill hole has recently gained popularity in the United States (Kang and Sperling, 2018). This approach is particularly useful for ablating difficult to reach epileptogenic regions, such as hypothalamic hamartomas, but it is not as effective as open surgery for mesial temporal lobe epilepsy (Jermakowicz et al., 2017; Gross et al., 2018). Future approaches could conceivably make use of currently experimental novel technologies such as focused ultrasound (Krishna et al., 2018), and optogenetic manipulation of discreet neuronal cell populations (Camporeze et al., 2018).
Advances in presurgical evaluation and surgical techniques have broadened the patient population undergoing surgical treatment for drug-resistant epilepsy. Whereas surgical therapy was seen as a luxury afforded only by industrialized countries, in recent decades the streamlining of presurgical evaluation procedures has made epilepsy surgery available in many countries with limited resources where it has proven to be highly cost-effective (Engel et al., 2005; Radhakrishnan, 2009). There is also an increasing application of surgical treatment to the pediatric population, particularly for infants and young children with life-threatening epilepsies that have now been demonstrated to result from large, but resectable, dysplastic cortex (Mathern et al., 1999). There has also been an increase in neocortical resections as a result of the ability of high-resolution MRI to identify small localized lesions, such as focal cortical dysplasias (FCDs) (Blümcke et al., 2016). As a result of preferential referral of patients for neocortical resection, and preferential referral of pediatric surgery for conditions that are also primarily neocortical, the percentage of surgeries for mesial temporal lobe epilepsy has decreased (Jehi et al., 2015). This has led to the impression that the condition of classic mesial temporal lobe epilepsy with hippocampal sclerosis is gradually disappearing. More likely, however, this reflects the fact that referral for epilepsy surgery in general, in the industrialized world, has actually decreased, despite marked improvements in the safety and efficacy, although relatively less so for neocortical epilepsy (Engel, 2016; Vakharia et al., 2017). It has been estimated that less than 1% of patients with drug-resistant epilepsy in the United States are referred to an epilepsy center (Engel, 2016), therefore, it would be unreasonable to infer any changes in the total number of patients with mesial temporal lobe epilepsy based on the small number who are referred for surgery.
Since the beginning of the 21st century, there have been three randomized controlled trials of epilepsy surgery, two for temporal lobe epilepsy (Wiebe et al., 2001; Engel et al., 2012) and one for pediatric epilepsy (Dwivedi et al., 2017). Based on the first randomized controlled trial, and a survey of the literature, a Practice Parameter was published by the American Academy of Neurology, in association with the American ILAE chapter and the American Association of Neurological Surgeons, recommending surgical intervention as the treatment of choice for drug-resistant temporal lobe epilepsy (Engel et al., 2003). Nonetheless, surgical referrals have continued to decline in North America and Europe. Not only are a very small proportion of patients with drug-resistant epilepsy referred to epilepsy centers, but those who are referred for surgery are referred an average of over 20 years after onset of their epilepsy (Berg et al., 2003), often too late to reverse longstanding psychological and social disability when seizures have been successfully eliminated. Two studies have demonstrated that this delay to surgical referral remains the same despite the first randomized controlled trial and Practice Parameter (Choi et al., 2009; Haneef et al., 2010).
This review of the history of epilepsy surgery has highlighted major technical and conceptual advances that have elevated this alternative therapy to standard of care for a large portion of patients with drug-resistant epilepsy, not only in the industrialized world, but in countries with limited resources as well. Research also promises to further improve the safety and efficacy of current techniques and to offer novel surgical approaches in the future. It would seem, therefore, that the major hurdle now in realizing the full potential of epilepsy surgery is not in the continued improvements of the treatment itself, but in addressing the treatment gap that is greatly limiting referral of potential surgical candidates to full-service epilepsy centers (Engel, 2019). This suggests that more effective education of patients and their physicians about the advantages of surgical therapy would offer the best chance for increasing application of this therapy going forward.
Supplementary data
Summary didactic slides are available on the www.epilepticdisorders.com website.
Acknowledgements and disclosures
Original research reported by the author was supported in part by grants NS02808, NS15654, NS21444, NS29625, NS33310, NS42372, and NS100064 from the National Institutes of Health, and the Resnick Family Foundation. Part of the review was adopted from Engel, 1993a and 2005.
None of the authors have any conflict of interest to declare.
* To celebrate the 110th anniversary of the International League Against Epilepsy, Epileptic Disorders is publishing a series of educational manuscripts on ground-breaking topics that have significantly influenced the field of epilepsy, written by past Presidents of the ILAE.