Epileptic Disorders
MENUEncephalopathy related to Status Epilepticus during slow Sleep: from concepts to terminology Volume 21, supplement 1, June 2019
Despite Encephalopathy related to Status Epilepticus during slow Sleep (ESES) being first reported more than 45 years ago, its defining features and diagnostic criteria are still a matter of debate. In addition, inconsistent terminology and concepts are used when referring to ESES, possibly causing unnecessary difficulties in the delineation of the syndrome and in the interpretation of the results provided by different studies. Edouard Hirsch, Roberto Caraballo, Bernardo Dalla Bernardina, Tobias Loddenkemper and Sameer M. Zuberi, five “epileptologists” with interest and experience in the diagnosis and management of ESES, express their opinions on the definition, the diagnostic assessment and the terminology that may be considered for this condition by answering selected predefined questions. The aim is to identify concepts for which there is a shared view (such as, for instance, ESES as a childhood epileptic encephalopathy encompassing Landau-Kleffner syndrome; the need to demonstrate, for the diagnosis of ESES, that the sleep EEG pattern has a clinical correlate, that is the appearance of cognitive/behavioral disorders; the possible role of disruption of sleep homeostasis), and areas where there are still disagreements on classification or controversies (such as, for instance, EEG evaluation and biomarkers, neuropsychological assessment, and terminology) which demand further studies and research (see also Tassinari and Rubboli, p. S82-7).
1) Is ESES a syndrome or a “self-limited” EEG pattern like hypsarrhythmia?
Roberto Caraballo (RC). It is an epileptic syndrome within the group of epileptic encephalopathies. According to age at onset, clinical manifestations, EEG pattern, evolution and prognosis, independent of etiology, it meets the criteria of the well-defined epileptic syndrome (Commission ILAE, 1989).
Bernardo Dalla Bernardina (BDB). ESES and Landau Kleffner syndrome (LKS) are one syndrome with variable clinical features; it is a childhood-onset encephalopathy characterized by the appearance of neuropsychological and behavioral disorders related to a significant and sustained activation of EEG paroxysms from drowsiness throughout all NREM sleep.
The clinical impairment can appear abruptly or progressively:
- –it can appear in a previously normal child or it can be a worsening of a pre-existing neuropsychological impairment;
- –it can be a global cognitive impairment or it can concern a specific domain only (Kuki et al., 2014);
- –the behavioral and psychiatric disorders can be of variable type and degree, leading to an autistic-like condition in some cases.
This peculiar electroclinical condition can appear, for unknown reasons (genetic predisposition, immunological mechanism, etc.), in any type of focal epilepsy of infancy or childhood of genetic (idiopathic), structural (both genetic or acquired), or unknown origin (Dalla Bernardina et al., 1978, 1989). In some cases, it can be induced by some AEDs.
Even if the mechanisms inducing the impairment are probably multiple and complex, one important factor can be a focal (Huber et al., 2004) or diffuse (Tononi and Cirelli 2014) disruption of sleep homeostasis induced by the recurrence of paroxysms (Tassinari and Rubboli, 2006; Cantalupo et al., 2011).
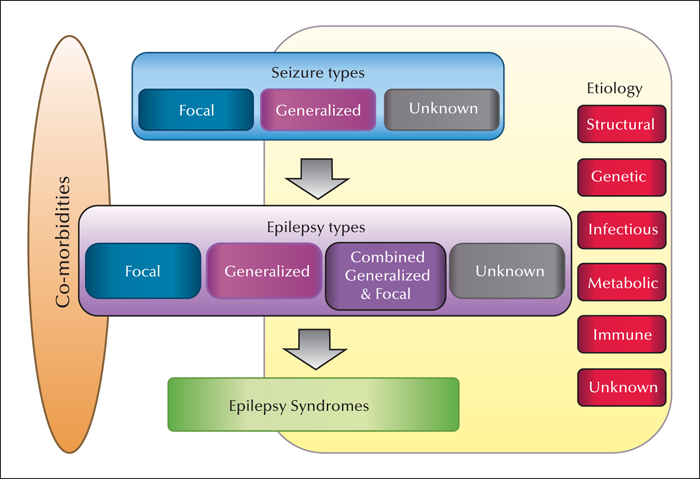
Edouard Hirsch (EH). Syndromes are defined according to non-fortuitous associations with signs and symptoms. To date, syndrome definitions have been based on expert opinions. In 2014, an ILAE position paper (Fisher et al., 2014) recognized epilepsies and syndromes as a group of diseases. The 1989 classification of epilepsies was revised in 2017 (Scheffer et al., 2017) (figure 1).
The Nosology and Definition Task force of the ILAE in 2018 are still discussing the definition of a syndrome. It is proposed that a syndrome is a characteristic cluster of clinical, EEG and laboratory (imaging, neuropsychology, etc.) features in an individual with epilepsy, often with etiologic, prognostic and therapeutic implications. Syndromes may have age-dependent presentations and specific co-morbidities.
The main changes in classification for “LKS”- “ESES” are presented in (figure 2):
- –Epilepsy Type: Generalized and Focal seizures may co-exist;
- –“LKS”-“ESES”, may have multiple etiologies even in an individual patient eg. genetic, structural, immune, inflammatory, metabolic.
The new ILAE commission on classification and terminology “2017-2021” is going to work on “syndrome” definitions and limits. One of the difficulties for this new commission is to try to have a scientific-based definition of syndromes.
Until now, I personally think that:
LKS and ESES are one syndrome:Childhood-onset Epileptic Encephalopathy with usually Generalized and/or Focal seizures and always Cognitive and Behavioral Acquired Co-morbidities and a Self-limited EEG pattern characterized by activation of Focal and Generalized EEG pathological “epileptiform transients” during sleep responsible for disruption of Sleep Homeostasis*.
* Disruption of sleep homeostasis: location and density of spike waves and slow waves are related to an alteration of the physiologic overnight decrease of the focal slow wave slope (Hirsch et al 2006; Bölsterli Heinzle et al 2014; see also Rubboli et al., p. S62-S70).
Tobias Loddenkemper (TL). Physicians utilize ESES terminology differently, and this may lead to miscommunication (Fernandez et al., 2013). Due to lack of consistent use, several colleagues conferred, and decided to use the term ESES for the EEG finding of sleep-potentiated or sleep-activated spiking. Therefore, to prevent confusion or miscommunication, we usually use ESES to describe the EEG feature that is one of the diagnostic features for epileptic encephalopathies within this seizure susceptibility complex of conditions. As with any terminology, this is simply convention, and there is ultimately no correct solution one way or another, as this is simply a term. However, it is crucial that all use the same terminology and assessment approach (Fernandez et al., 2013).
Sameer M. Zuberi (SMZ). The association of status epilepticus during sleep and encephalopathy through childhood is associated with too many different aetiologies, too many different treatments and too many different outcomes for it to be classified as an epilepsy syndrome. ESES should be regarded as an important self-limited EEG pattern associated with a degree of potentially reversible cognitive and physical impairment that can occur in many epilepsy syndromes and with multiple different aetiologies. As noted above, this EEG pattern can be triggered by AEDs. How many syndromes are produced by AEDs? The broader concept of encephalopathy is fundamental to all types of epilepsy, whether the encephalopathy is due to the aetiology, the nature of the epilepsy type or syndrome or the use of medication. Encephalopathy in epilepsy should not be separated into a syndrome. The potential for different degrees of encephalopathy must be acknowledged in everyone with the brain disease epilepsy and having a separate group “the epileptic encephalopathies” averts the gaze of the clinician to this important issue.
Epilepsy classification should serve better treatments and encourage research in the epilepsies. Clinical groupings comprising many conditions with shared EEG features but markedly disparate aetiologies, outcomes and treatments such as Ohtahara syndrome, Lennox-Gastaut syndrome and ESES have had an important role in the history of epilepsy classification but have reduced clinical relevance as science reveals underlying aetiologies and mechanisms with the goal of more precise therapies (Scheffer, 2017).
Landau-Kleffner syndrome (LKS) is an epilepsy in which ESES is a key clinical feature and I would regard LKS as an epilepsy syndrome.
2) If it is a syndrome, what are the minimum criteria for definition?
RC. This is a well-defined epileptic syndrome in the group of epileptic encephalopathy (Engel, 2001: Berg et al., 2010) starting in childhood characterized by focal motor seizures, complex focal seizures, apparently generalized seizures (clonic, tonic-clonic seizures, absences), and myoclonic seizures, associated with neurological deterioration involving cognitive, behavioral and/or motor domains. Typical EEG pattern is a status epilepticus during sleep (ESES) at sleep onset defined as a pattern of diffuse spike-and-waves (symmetric, asymmetric, unilateral or focal) occurring in up 85% of slow sleep and persisting for months or years. Less than 85% of the spike-and-waves index should also be considered. Its relationship with focal idiopathic epilepsies of childhood particularly Rolandic epilepsy is very well known, and Epileptic Encephalopathy with SES may correspond to a broader clinical phenotype of idiopathic focal epilepsies of childhood. The genetic findings in these groups of patients could be explained by their close genetic link. Landau-Kleffner syndrome could be considered a variant of Epileptic Encephalopathy with SES considering that most of the patients with auditory verbal agnosia present ESES.
BDB. (A) Childhood onset; (B) appearance or worsening of Neuropsychological and/or Cognitive and/or Behavioral impairment; (C) Self-limited EEG pattern characterized by sustained focal and/or diffuse EEG paroxysms activated by drowsiness throughout all NREM sleep; (D) Focal/multifocal/generalized seizures mainly nocturnal, and rare in most cases. In some cases overt clinical seizures may be lacking; (E) Atypical absences with or without associated motor phenomena, mainly inhibitory, in some cases.
Only A,B,C are consequently mandatory criteria.
EH. (A)Childhood onset; (B) Cognitive and Behavioral Acquired impairment; (C) Self-limited EEG pattern characterized by activation of Focal and Generalized EEG pathological “epileptiform transients” during Sleep responsible of Sleep Homeostasis Disruption; (D) Generalized and/or Focal seizures
Mandatory: A+B+C
TL. ESES may refer to the EEG pattern associated with childhood seizure susceptibility syndromes, including Landau Kleffner syndrome, and Continuous Spike and Wave during Slow wave sleep (CSWS). For a suspected diagnosis of CSWS, consideration of the following parameters may be helpful: A) childhood onset, B) sleep-potentiated/-activated generalized or focal spiking or sharp waves, C) comorbidities in two cognitive/developmental domains (including fine and gross motor, language and social/behavioral, among others), and - not mandatorily - generalized and/or focal epileptic seizures. For a suspected diagnosis of LKS, consideration of the following parameters may be helpful: A) childhood onset, B) sleep-potentiated/-activated generalized/focal spiking or sharp waves on EEG and C) impairment in language development, and - not mandatorily - generalized and/or focal epileptic seizures.
Ultimately, a longitudinal course, recognition of evolution through different disease stages (Fernández et al., 2012), and application of treatment and response to treatment (specifically in EEG and cognitive features) may also serve as confirmation of a diagnosis. Response to treatment may be more evident in children presenting with more frequent spiking and more acute or more severe onset of development and cognitive features, or lesser cognitive reserve, including regression. Therefore, response to treatment and resolution over time may be an additional diagnostic criterion, and while confirmatory, this approach may at times not be practical when encountering a patient during the acute phase of the condition. However, a similar approach including the response to intervention has been successfully adopted for non-convulsive status epilepticus (Beniczky et al., 2013).
SMZ. As described above, I do not regard ESES as a separate syndrome. I would agree that the features of ESES include: A. Childhood onset; B. Encephalopathy with acquired impairment of cognitive, behavioral and sometimes motor function; C. Self-limited focal and generalized spike-wave EEG abnormalities during sleep sufficient to disrupt sleep homeostasis.
These criteria are insufficient in themselves to comprise a syndrome. The disruption to sleep homeostasis and the functions of sleep is critical to understanding the impact of status epilepticus during sleep. Sleep is for the brain and generated by the brain. Understanding how sleep disruption in general impacts on health and well-being in epilepsy is an important focus of research. Normal sleep is required for memory and learning with increasing evidence that consciousness and the organization and encoding of long-term memories are mutually exclusive. We need to undertake these processes in sleep in order to allow us to have reference points for consciousness in wakefulness.
3) Which EEG diagnostic criteria would you endorse for the diagnosis of ESES?
RC. We believe that the definition of the electro-clinical inclusion criteria of the epileptic syndrome or epilepsy type is fundamental, however accepting very strict inclusion criteria may sometimes hinder the inclusion of patients with typical or classical EEG patterns. Thus, we think that a group of patients with the characteristic clinical manifestation of epileptic encephalopathy but less than 85% of the ESES (between 50 to 85%) should be included. Other types of EEG abnormalities during slow sleep, such as multifocal spikes, frequent asynchronous bilateral spikes, diffuse slow-wave activity and different morphology of EEG abnormalities in both cerebral hemispheres should also be considered and discussed in the EEG inclusion criteria (Caraballo et al., 2015).
One point is to define the quantitative and qualitative EEG parameters in our daily practice and which are the EEG parameters that we should consider methodologically to develop a scientific study. A sleep EEG recording lasting 30-60 minutes could be enough in the first situation, whereas a whole-night NREM sleep should be considered in the second. There are different proposals to define the qualitative and quantitative aspect of ESES (see also Gardella et al., p. S22-S30), thus a consensus should be crucial to delineate the EEG inclusion criteria for this syndrome considering also the facilities commonly available in neurological departments.
BDB. The only EEG criterion is constituted by a sustained activation of focal and/or diffuse EEG paroxysms from drowsiness throughout all NREM sleep, provided that it is related to a documented clinical impairment.
The paroxysms can remain focal (unilateral or bilateral) (see figure 3 in Gardella et al., p. S22-S30 hemispheric (see figure 4 in Gardella et al., p. S22-S30) or they can become bilaterally diffuse (see figures 1, 2 in Gardella et al., p. S22-S30).
The frequency of the paroxysms is not part of the definition but they must be clearly and continuously more frequent than during wakefulness.
Even if frequency, topography, and morphology of the EEG paroxysms do not constitute diagnostic criteria, they must nevertheless be analyzed and reported because the clinical features can vary according to different EEG patterns.
On awakening, the paroxysms can be focal/multifocal/diffuse or, although rarely, even absent. Consequently, EEG paroxysms on awakening do not constitute a mandatory criterion.
EH. Self-limited EEG pattern characterized by the following:
- 1During wakefulness: focal and/or generalized focal or multifocal spikes and/or spike-waves; “epileptiform transient”
- 2Tangential dipole for “epileptiform transient”
- 3Sleep activation of focal and/or generalized EEG transients
Mandatory: 1+2+3
TL. A) Sleep-activated/-potentiated focal or generalized spikes and sharp waves are supportive of a diagnosis, specifically during sleep stages I, II, and III. Spikes and sharp waves may be generalized or focal (Fernández et al., 2013; see also Gardella et al., p. S22-S30). These spikes and sharp waves are usually not seen at the same frequency during wakefulness or REM sleep. While the spike-wave index and spike frequencies during slow-wave sleep are most frequently used, ranging from 25% to 100% (or with even greater range), and while a spike wave index of at least 50% may be overall helpful, a specific cut off may not be the optimal EEG parameter, depending on the stage of the condition, as EEGs are at this point merely reflective of a short period of time, and based on assessment method. Of note, the spike wave index may temporarily drop below any certain percentage during treatment, and recur, but this drop does not imply that the condition has entirely resolved, and may likely imply sampling and information bias. Equally important for diagnosis rather than the actual frequency of spiking during sleep may also be the sleep (including stages I, II, and III) to wakefulness (or REM) ratio of spikes, meaning that spikes usually are more frequent during sleep than during wakefulness, and a ratio greater than 3:1 may frequently suggest a diagnosis. Again, this marker also suffers from sampling and information bias. Please note that any of these cut-off ratios have limitations, and that a combination of overall sleep frequency and a ratio between sleep and wakefulness over time may be most helpful. Ultimately, any specific figures for spike frequency/spike wave index, or a spike ratio may be based on expert opinion, and while currently most practical, both may only be a placeholder for more improved detailed longitudinal EEG assessments in the future.
B) Disruption or lack of normal sleep features and patterns may also help with the diagnosis. As outlined, spike frequency or spike wave index can be relatively conveniently assessed. Other EEG biomarkers, such as a lack of or decrease in normal sleep features, such as spindles, Vertex waves, and K-complexes, as well as disruption of sleep cycling, high-frequency in relation to slowing, and a related lack of changes in the slope of the slow wave sleep throughout the night, among others, may ultimately prove to be better EEG biomarkers (see also Rubboli et al., p. S62-S70, and Tassinari and Rubboli, p. S82-7). A simple biomarker, until better tools are available for assessment, without calculation of the slow-wave sleep slope over time, may be lack of (or reduction of) normal sleep features, implying also disruption of sleep homeostasis and nighttime memory formation and learning.
SMZ. Duration of the status epilepticus in sleep will impact on the degree of sleep homeostasis disruption however the duration required to produce an acquired encephalopathy will vary from individual to individual. Setting this percentage at 85%, 50% or 30% is to a degree arbitrary. The term status in epilepsy implies a particular continuous duration of focal or generalized EEG discharges or clinical abnormalities. The abnormalities in ESES may not be continuous throughout slow wave sleep.
Whether a particular percentage of sleep disruption results in an acquired cognitive, behavioral or motor impairment will depend on the resilience of the individual brain influenced by many factors (genetic and environmental) and also on the sensitivity of measures assessing impairment. The presence of spike-wave abnormalities in the awake EEG is not required.
ESES is present when there is a measurable acquired encephalopathy (cognitive, behavioral, +/- motor impairment) associated with sleep activation of focal and generalized spike-wave abnormalities.
4) How do you assess the occurrence of Encephalopathy in SES?
RC. By definition, neurological deterioration occurs in all cases of this syndrome. It usually is coincidental with the detection of ESES representing one of the crucial signs of the syndrome. The encephalopathy is represented most frequently by a combination of disturbances in one or more domains, including language, cognition, behavior, and motor abilities. A neuropsychological and motor assessment follow-up in all patients is fundamental to define neurological deterioration, their relationship with ESES, response to the treatment, evolution and prognosis. According to the cognitive profile of the patients we should choose the neuropsychological test to perform (see also Arzimanoglou and Cross, p. S71-5).
BDB. Considering that the diagnosis of ESES requires that the abnormal increase of the EEG paroxysms during sleep is associated with a documented appearance or worsening of a clinical impairment, the diagnosis and the management of ESES needs both repeated sleep EEG and neuropsychological assessments.
In the case in which the abnormal increase of the EEG paroxysms during sleep appears or is recognized in a child for whom a previous adequate neuropsychological assessment is available, the diagnosis of ESES can be done if a new assessment documents a neuropsychological impairment.
If a previous neuropsychological assessment is lacking, the diagnosis of ESES can be done if two sleep EEG-neuropsychological assessments (separated by 1-3 months) document a progressive impairment. The interval must be chosen according to the clinical picture.
The diagnosis of ESES can be ascertained upon recognition of the EEG picture during sleep in cases in which the sleep EEG has been performed due to the appearance of an unexplained clinical impairment.
EH. Onset of cognitive and/or behavioral acquired impairment not related to AEDs.
TL. Cognitive and behavioral co-morbidities in language, fine and gross motor, or social/behavioral domains, among others, play a role. Presence of regression (loss of function in different domains) is most significant, but may not always be present, depending on the stage of the condition and depending on prior treatment. Cognitive findings should ideally not be easily explained by other etiologies.
SMZ. The encephalopathy is the clinicalimpairment and as such ESES cannot be defined on EEG criteria alone. It is important that children with ESES have early and continuing neuropsychological assessment and that developmental monitoring is linked with appropriate psychological, social and psychiatric support to improve mental wellbeing and social participation. Evaluations need to be consistent in any individual and separated by a reasonable time. Re-testing using the same neuropsychological instrument may require a gap of 6 months. General observation and description of behaviour does have clinical value and should not be neglected. Full scale IQ and performance IQ should be evaluated with awareness that more specific impairments in subsets including verbal IQ may be present (Dorris et al., p. S88-S96). Instruments for behavioral assessment such as the Child Behavior Checklist (CBCL) should be considered. If motor impairments develop alongside cognitive and behavioral problems, these should also be assessed including the use of serial videotape recordings.
5) How would you define the resolution of ESES?
BDB. A recovery or a documented improvement of the neuropsychological picture related to the disappearance of the abnormal activation of EEG paroxysms during sleep.
The improvement can be transient or permanent. Only with an adequate follow-up according to the age of the child can resolution be considered as permanent.
In several cases, the clinical improvement following the EEG improvement can be very slow and in many cases, it is not a complete recovery. Consequently, the resolution of ESES must be considered as the resolution of the EEG picture associated with a clinical improvement and not necessarily the recovery of the pre-ESES clinical status.
EH. Recovery of pre-morbid cognitive and/or behavioral status.
TL. With regards to resolution of the condition, recovery of EEG biomarkers and neuro-developmental features to baseline levels (or ideally levels relative to normal peers at the same age) for extended periods of time (ideally into adulthood) may be optimal, and resolution of seizures may be supportive. However, depending on etiology, some patients may have life-long cognitive deficits and continue to present with EEG features later in life, and with current monitoring and interventions may not return to premorbid or peer-related baseline. Remission of EEG features may be defined by reduction of EEG features below diagnostic criteria, but similar to other conditions, frequent monitoring may be required into adulthood to evaluate for recurrence.
SMZ. The disappearance or significant improvement in the EEG abnormalities with no further evidence of a progressive encephalopathy as demonstrated by neuropsychological assessment. Many of the children after resolution of the ESES do not return to their premorbid state (Dorris et al., p. S88-S96).
6) Several eponyms have been proposed, i.e. ESES (encephalopathy related to status epilepticus during slow sleep), CSWS (continuous spike and waves during sleep), ECSWS (encephalopathy with continuous spike and waves during sleep), Tassinari's syndrome. Is there one that you would suggest, or would you propose an alternative one?
BDB. In my opinion the best choice would be “Tassinari's syndrome”. If the introduction of new eponyms is no longer accepted by the ILAE Classification Task Force, the only choice justified is “ESES”, i.e. “Encephalopathy related to Status Epilepticus during slow Sleep”.
For the syndrome definition, the term CSWS is unacceptable because it is an EEG descriptor and it is impossible to define a syndrome on the basis of the EEG pattern only. However, the EEG pattern cannot be described using the term of the syndrome. Hypsarrhythmia is not a syndrome and West syndrome is not a descriptor of the hypsarrhythmic pattern.
The term CSWS may be used to describe the EEG pattern. The criticism of this choice would be the fact that the component “continuous” is not mandatory in the definition of the syndrome. One possibility would be to describe the condition as “Spike Wave Status during Sleep” (SWSS).
In other words, ESES (Encephalopathy related to Status Epilepticus during Sleep) is in fact an epileptic “Encephalopathy with SW Status during Sleep, i.e. ESWSS”.
LKS is one of the clinical types of ESES with predominant language impairment as well as cases with “autistic regression”, cases with “absences and inhibitory phenomena”, “atypical benign partial epilepsies (ABPE)”, and cases with “specific neuropsychological impairment”. These latter conditions are other clinical types of ESES needing in some way different treatments and especially different rehabilitative strategies.
EH. Current 1989 definitions for LKS as well as for ESES are too narrow. Former ILAE Classification Commissions & Task Forces do not seem to support new eponyms for syndromes. One alternative is Penelope Syndrome of Childhood (PSC) to name a Self-Limited Childhood Epileptic Encephalopathy with Spike Wave Status during Sleep and disruption of sleep homeostasis (Cantalupo et al., p. S31-S40).
TL. It is crucial recognize the ground-breaking contributions of Drs. Tassinari, Landau, and Kleffner, and many others, also including the prestigious coauthors of this article and in this special issue, to the spectrum of these conditions, and I would like to honor the contributions of these pioneers in the field. However, allow me to also recognize that any specific terminology may not be sufficiently broad to capture the longitudinal presentation and evolution as well as implications of this spectrum of conditions for learning, memory and development during sleep. An overarching terminology for the spectrum of these conditions would be very helpful, and some colleagues currently try to broadly refer to this larger category as childhood seizure susceptibility syndrome(s), in an attempt to characterize the longitudinal course as well as temporary susceptibility to increased epileptogenicity and often temporary sleep features and pattern disruption. While there is need for a common broader term, there are no scientific arguments for or against certain terminology, only expert opinion. A common terminology would, however, greatly benefit all, most importantly including our patients, and facilitate recognition, care, treatment, and future research.
SMZ. Encephalopathy related to Status Epilepticus during slow Sleep (ESES) includes the key clinical features and is sufficient. As I don’t regard the clinical entity as consistent enough to be a syndrome, I don’t think it should be given an eponymous name.
Landau-Kleffner syndrome is appropriate for this condition.