Epileptic Disorders
MENUElectroclinical markers to differentiate between focal and generalized epilepsies Volume 23, issue 3, June 2021
Figures
Tables
Learning objectives for the ILAE curriculum
The key learning objectives of this report, in-line with the ILAE Roadmap for a competency-based educational curriculum in epileptology, align to Sections 1.3, especially 1.3.5, and 1.7 [1].
1.3 Identify and describe seizure semiology using standardized ILAE terminology and classification systems
1.3.1 Learn and recognize the seizure semiology and distinguish it from other non-epileptic manifestations
1.3.2 Extract semiology information from patient history
1.3.3 Extract semiology information from video recordings
1.3.4 Interpret semiological signs and symptoms allowing hypotheses on the localization of focal seizures
1.3.5 Interpret semiological signs and symptoms suggesting focal vs. generalized onset
1.3.6 Classify seizures according to the ILAE classification
1.7 Accurately diagnose and classify epilepsies and epilepsy syndromes using the most recent ILAE classification
1.7.2 Correctly distinguish between focal and generalized epilepsies (and recognize epileptic encephalopathies*)
1.7.3 Correctly diagnose and classify focal epilepsies
1.7.4 Correctly diagnose and classify generalized epilepsies
1.7.5 Correctly diagnose and classify combined focal and generalized epilepsies (including epileptic encephalopathy*)
* epileptic encephalopathy is covered in another Epileptic Disorders report.
Competencies and learning objectives acquired from reading this report should result in being able to:
- •Understand the definition of a generalized versus a focal seizure
- –Document the ILAE definition and understand how this relates to brain network propagation of seizure foci
- •Document the terminology to describe generalized and focal epileptic seizures
- –Understand the relevance of focal seizures with or without loss of awareness
- –Describe the different motor and non-motor seizures occurring in generalized and focal epilepsies
- •Understand the challenges in differentiating between focal and generalized seizures
- –Understand how to attain a comprehensive history from the patient and witnesses
- –Establish the indicators in the past medical history and clinical examination to support focal versus generalized seizures
- –Identify the clues in the seizure semiology to support focal versus generalized seizures
- –Understand how investigations aid differentiation of focal versus generalized seizures
- –Understand what the potential confounders or pitfalls are to challenge differentiation of focal versus generalized, e.g. maturity of the child, co-morbidities, failure to witness seizure onset.
Epileptic seizures are traditionally divided into focal, generalized, combined and unknown epilepsy categories [2]. The classification of seizures by the International League Against Epilepsy (ILAE) is predominantly a descriptive and dynamic process, and if there is a lack of clarity then this should be acknowledged until it is possible to be more certain of the correct epilepsy term [3].
What is a generalized seizure and what is a focal seizure? (tables 1, 2)
A generalized-onset seizure originates at a point within the brain, and rapidly engages bilaterally distributed networks [3]. In comparison, a focal-onset seizure originates within networks limited to one hemisphere which may be discretely localized or more widely distributed. The result is that the clinical manifestations in the resultant seizures differ according to the network activity.
Epilepsies which include generalized seizures are documented to be more prevalent than focal epilepsies, however, focal epilepsies account for 20% to 66% of incident epilepsies in published studies [4]. Virtually all prevalence and incidence studies report a preponderance of seizures of unknown cause [5]. Such estimates are challenged by a lack of information from many regions and where the quality of the assessment of whether events are generalized or focal is lacking [4]. The wide range documented in studies of focal epilepsies illustrates this.
According to the ILAE 2017 classification of seizures, focal seizures are divided into those in which the affected person is aware and those in which there is impaired awareness [2, 3]. The previous terms used, namely “simple” or “complex partial seizures”, are no longer considered appropriate in the descriptive terminology for focal seizures. Focal seizures are further categorized into those with motor or non-motor features [3]. Motor-onset events include automatisms, epileptic spasms, and atonic, clonic, hyperkinetic, and myoclonic and tonic events; whilst non-motor onset can be autonomic with behavioural arrest, cognitive impairment, emotional change and sensory features.
The ILAE 2017 classification defines generalized seizures under the same headings as focal seizures, i.e. motor and non-motor [2]. Loss of awareness occurs with most, but not all, generalized events, and can be challenging to measure, e.g. in myoclonic seizures [2, 6, 7]. Generalized motor-onset events are tonic-clonic, tonic, clonic, atonic, myoclonic, myoclonic-tonic-clonic, myoclonic-atonic and epileptic spasms, whilst non-motor are absences which can be typical, atypical, myoclonic or eyelid myoclonia [3].
The ILAE classification also acknowledges that patients may have both generalized and focal seizures, referred to as “combined”.
If a seizure is of unknown onset, useful defining motor (e.g. tonic–clonic) or non-motor (e.g. behavioural arrest) characteristics to the event can still be noted [3]. Targeted follow-up can lead to consolidation of these findings and re-categorization into focal or generalized onset. As such “unknown-onset” is not a characteristic of the seizure, but a term to use whilst awaiting a more definitive categorization. In this setting, as it may not be possible to categorize a patient, a diagnosis of “unknown onset” should be used instead during follow-up.
More detailed descriptions of the semiology of the various focal seizure manifestations and types of generalized seizures are eloquently summarised by the “Instruction Manual for the Operational Classification of Seizure Types” by Fisher et al.[3].
Table 1provides a concise summary of key differentiating features between generalized and focal epilepsies.
Table 2 summarizes the common generalized seizures in relation to their electroclinical semiology, associated epilepsy syndromes and other relevant points.
Table 3 details lateralizing features which can assist in the identification of the focal region of seizure onset, but also highlights features which may assist better delineation of “unknown-onset” cases, as well as where the seizure may still be generalised.
What is the relevance to diagnosing a generalized or a focal seizure?
Once a diagnosis of an epileptic seizure is confirmed, delineating the type of seizure is the next activity recommended on the ILAE roadmap [8, 9]. Clarifying the type of seizure affecting the patient has implications for the aetiology and subsequent investigations [10]. Differentiating between focal and generalized seizures can influence selection of antiseizure medications (ASMs) and referral for epilepsy surgery assessment [11]. Confirming an epilepsy syndrome diagnosis may influence the choice of treatment and the prognosis. Identifying an epilepsy syndrome can also highlight the need to monitor for the development of further seizure types, which may occur as part of a syndrome, or become evident with brain maturation. Infants with West syndrome, consisting of the triad of developmental delay or regression, epileptic spasms and hypsarrhythmia, can evolve to Lennox-Gastaut syndrome in early childhood with new seizure types and requiring different ASMs. Dravet syndrome is associated with different seizure types, manifesting as the affected child becomes older.
Various settings can result in both focal and generalized epileptogenic dysfunctions co-existing, namely diffuse hemispheric abnormalities, multifocal abnormalities, and bilaterally symmetrical localized abnormalities [12]. As such, a neurologic disorder which affects both hemispheres, whilst having a generalized effect on neurocognition and function, can still be associated with focal seizures, generalized seizures or combined seizures. An example of this would be a person with meningitis or encephalitis, in whom both hemispheres incurred insults, and focal seizures resulted from various regions independently of each other. Accordingly, diagnosing focal seizures does not necessarily equate to an isolated area of brain involvement, and extensive networks can still be involved.
How can one differentiate generalized from focal seizures?
Differentiating between focal and generalized epilepsy is traditionally based on the combination of clinical history, detailed description of seizure semiology, physical examination, inter-ictal EEG, imaging data, and if possible ictal video-EEG (vEEG) recording [10]. The process can be complex.
As illustrated in tables 1, 3, it is useful to consider the key differentiating features between generalized and focal epilepsies.
The anatomical region of the seizure onset influences the clinical manifestation of the event. For example, seizures which commence in networks in the frontal lobe are typically more involved in higher intellectual or motor functions, the parietal lobe with simple sensory components and temporal lobe with emotion, hearing and smell, whilst the occipital lobe is involved with vision. Table 3, adapted from the comprehensive report by Loddenkamper and Kotagel, provides a detailed summary of lateralizing features supportive of an anatomical ictal focus [13].
Generalised seizures are typically considered to be associated with loss of awareness, but subtle signs are described in the prelude to an event, and affected individuals may be conscious of “trigger” activities or settings that place them most at risk [14]. Usually this is immediately (seconds) before the ictal event, but may permit the affected individual to sit down or reach out to someone [15]. However, there are some generalized seizure disorders with retained awareness during the ictal event. This is reported in patients with juvenile myoclonic epilepsy [7, 16].
An adult-based study explored seizures with altered awareness and minimal motor involvement, to identify differentiating features between focal seizures and generalized seizures [6]. In this study, 10 of 16 patients had recall of vEEG documented generalized seizures. Automatisms in this group were not found to be reliable differentiating events. Similarly, whilst head deviation was found more frequently in patients with focal seizures, it also occurred to a lesser extent in those with generalized seizures [6]. However, preceding aura was only recorded in patients with focal seizures and as such, if identified, is a reliable delineating event. Sensory unilateral auras tend to be contralateral to structural lesions and can assist epilepsy surgery planning, especially when they are well localized [13].
Seizures of short duration ([6]. The same study reported that eye blinking was also more evident in patients with generalized seizures. However, another study of 180 seizures from 50 patients with medial or neocortical temporal lobe epilepsy found that patients over 18 years of age were more likely to blink during seizures compared to those in the childhood and adolescent age group [17]. They suggested that there was a developmental influence for the manifestation. As such, blinking during a seizure is not a reliable sign to differentiate between focal- and generalized-onset seizures.
The differentiation between generalized seizures and focal seizures which have evolved to bilateral generalized seizures can be challenging. In children with generalized seizures, mouth-opening during the event and post-seizure motor movements are more likely to occur in the setting of focal seizures with bilateral generalized seizures [18].
Versive events which equate to forced and involuntary movements, resulting in sustained unnatural positioning, are often contralateral to the side of seizure onset [19]. This sign is considered useful when present in generalized seizures suspected to be of focal onset evolving to bilateral generalized seizures [20]. However, versive events are also reported in generalized-onset seizures [12]. Overall, if version occurs immediately before the tonic-clonic phase of a seizure, is associated with neck extension, and also associated with late ipsiversion after the end of a generalized tonic–clonic seizure, these features support a focal-onset event [21].
Asymmetric seizure termination, whereby the last clonic jerk is ipsilateral to the hemisphere of seizure onset, supports generalized seizures as bilateral generalized with focal-onset. [22].
Asymmetric tonic limb posturing during a seizure manifests typically with one arm flexed at the elbow, and the other extended, often referred to as the “sign-of-4”. Patients with bilateral generalized seizures, inclusive of asymmetric tonic limb posturing, have an ictal focus contralateral to the extended arm in most cases, especially patients with TLE [23].
Patients with idiopathic generalized epilepsies do not have unilateral dystonic posturing compared to patients with TLE in whom it is common, when bilateral tonic-clonic seizures occur [24, 25].
Post-ictal states can also provide useful differentiating features. Todd's palsy always equates to the contralateral side of the focal seizure onset [13]. Postictal confusion can be challenging to differentiate from aphasia following a focal seizure originating from the dominant hemisphere. In this setting, speech and language assessment of expressive, receptive and mixed aphasia is important.
Clinical information
What information is important to access from the patient or caregiver?
The personal and familial medical history is important to assimilate. Explore events in the patient's history which might represent risk factors for developing epilepsy. Examples include a peri-natal insult, traumatic brain injury, meningitis or encephalitis, brain tumour or history of prolonged febrile seizures in childhood for adult patients [10]. Familial history of epilepsy or neurological diseases is also important with regard to genetic disorders, such as tuberous sclerosis complex (TSC). Furthermore, familial history of epilepsy and hereditary predisposition is not unusual in patients with idiopathic generalized epilepsy [26].
What are useful semiological characteristics of seizure types
In order to differentiate these different types of seizures, the clinician needs to consider a “detective style” approach which would allow him/her to clearly visualize the seizure semiology that probably occurred. This approach requires attaining all available details from the patient as well as witnesses, for ideally more than one event. This is particularly important for patients who are not aware during the event. People with bilateral tonic-clonic evolution are often mislabelled as having generalized seizures, hence the importance in the details of the onset of the event. Accordingly, the witness should have been present from the start of the event [27], in order to give details of the initial semiology that might be consistent with a focal onset, as illustrated in table 3[13]. Additional important clinical clues include establishing what the affected person was doing before the event started and if there was a change in their normal routine (less sleep or food, more stress, an intercurrent illness, etc.) [28]. Establishing if there are reproducible triggers to the event can support a diagnosis of epilepsy, for example, in the reflex epilepsy groups whereby events can be caused by reading, thinking or eating [29]. In the setting of a person who appears to be unaware, it is important to verify whether this was confirmed by lack of response to tactile stimulation.
Questions should be culturally appropriate using terminology which is understood by laypersons in their local setting. Questions should also be sensitive to the stigma often carried by having epileptic seizures and associated caution is needed as this results in reticence in divulging the full nature of associated events [30]. Providing the witness or caregiver with illustrations of the suspected events can be useful. As such, the clinician must become adept at performing clonic movements, myoclonic jerks and absence events to demonstrate typical events to witnesses. A caregiver may struggle to estimate the duration of an event especially in the setting of anxiety and concern of watching a “loved-one” seize. Demonstrating that a myoclonic jerk lasts a micro-second (shock-like) rather than being held for a few seconds (spasm or tonic seizure) is useful. Counting the seconds can help a caregiver estimate the duration in which a child with absence seizures is unresponsive. Lastly, the witness should also be asked whether they noted a change in behaviour of a person with epilepsy prior to the seizure event, for example, emotional lability, confusion, agitation, and so on.
In addition to the clinical description of the event, asking witnesses to point to the affected side of the patient can avoid potential confusion between left and right laterality. Erroneous documentation of laterality can lead to an assumption of poor anatomical correlation or that the person with epilepsy has more than one focal area of seizure involvement. Also, asking the witness to demonstrate a facial expression or movement that they saw can be very useful to differentiate between tonic, clonic, myoclonic or automatisms. Individuals are unwittingly biased in their interpretation of observations across multiple levels which includes assumptive terms used during witness descriptions and the clinician assimilation of this information provided [10]. Several witnesses can observe the same event and provide completely different descriptions [28]. For this reason, it is important to keep an open approach and to repeat the clinical history and description of the events often. Start with open-ended questions, such as “describe what you saw” and move to closed questions; “did his eyes go to one side”, “point to the arm that moved”, “could he talk to you after the event”, etc. Always ask about the state of the person with epilepsy at the end of the event, specifically if they are weak or have impaired movement following an event (Todd's palsy), also whether they can speak after an event and are able to correctly name common objects. Impairment in any of these areas would support a focal region being affected (table 3).
Asking the person with epilepsy what they remember of the events and whether they were all the same also assists with differentiation and localization. For example, a child with self-limited childhood epilepsy with centrotemporal spikes will often report an inability to speak at the start of the event but will retain language comprehension. Attaining this information aids both anatomical localization but also syndromic diagnosis. Other tools to incorporate include asking children to draw what they feel happens to them both during a seizure and how the condition makes them feel about themselves. Whilst a child may struggle to say how they feel or what they experience, they all learn to draw from an early age and often find this an easier way to express what happens to them [31].
In the current age of the smartphone, clinicians and caregivers are becoming increasingly engaged in the use of this as a tool to delineate seizure types. In some cases, this can be exceptionally useful, sparing the person with the events the need to undergo further costly or invasive interventions. The quality of the captured event tends to be the restricting element for the tool. The start of the events are rarely captured and, as illustrated above, this is vital in the setting of delineating both the semiology of a focal epileptic seizure and to be able to differentiate from a generalized-onset seizure [27].
What aspects of the clinical examination are important?
Clinical examination is important. Evidence of focal pathology, such as a hemiplegia, would support the anatomical region of concern being due to a focal aetiology. Examination may be relatively unremarkable and require subtle neurological screening to detect functional asymmetry, such as the Fogg manoeuvre in which the patient is asked to walk on the outer lateral boarders of their feet (feet inverted at the heels) and this destabilization in the gait leads to a clawing of the affected arm. Subjects may become habituated to this sign, therefore it is only useful in the early stages of routine examination. Evidence of a neurocutaneous syndrome may support a disorder such as tuberous sclerosis complex (TSC). Whilst over 80% of people with TSC have seizures which are focal in the majority, it cannot be assumed that this is the case without further exploration [32]. In a person with generalized epilepsy, especially those of genetic aetiology, clinical examination may be normal. However, other cases with structural or infective aetiologies may reveal clues of a global brain disorder, for example, microcephaly. As such, the finding of abnormal neurology can be useful to support a neurological process, but again, this would not necessarily be specific for focal versus generalized seizures. As stated earlier, the involvement of both hemispheres does not automatically dictate that an associated epilepsy is focal or generalized. For example, evidence of dysmorphology and cognitive delay may suggest a generalized brain disorder, but without clinical supporting evidence, associated seizures cannot be assumed to be generalized.
How can one differentiate between focal and generalized seizures using EEG?
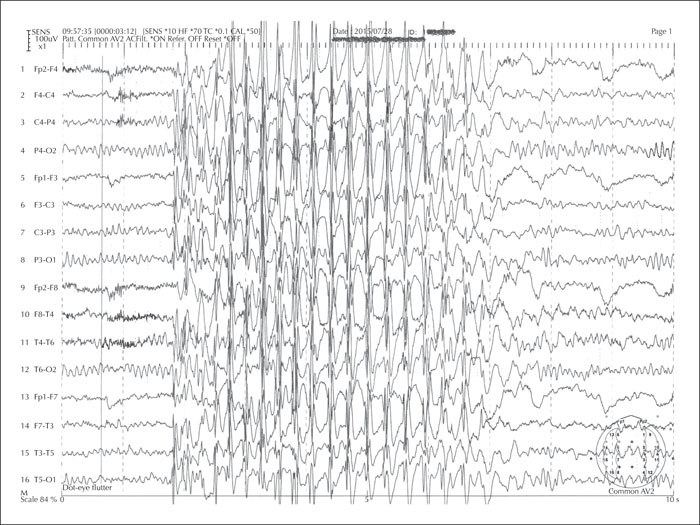
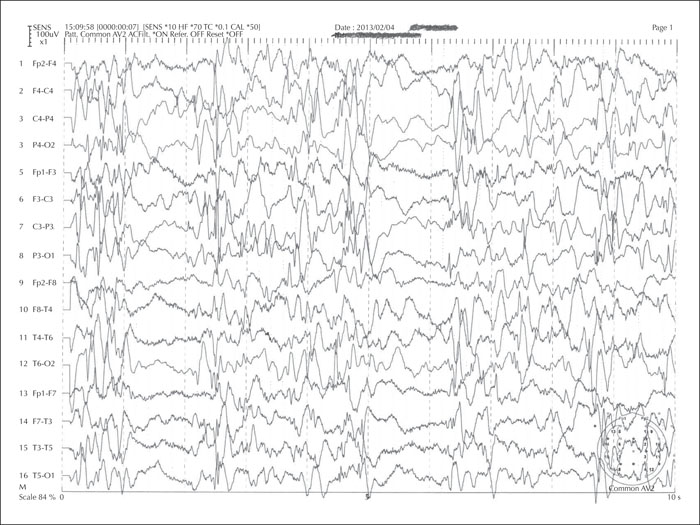
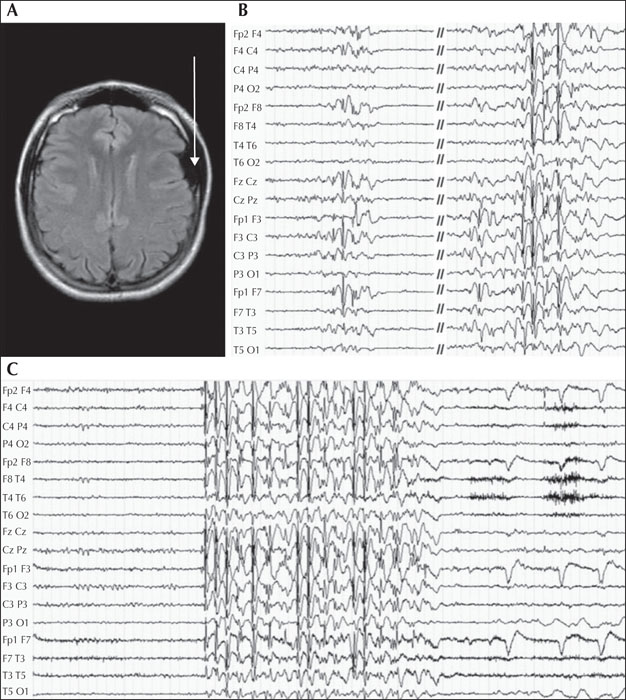
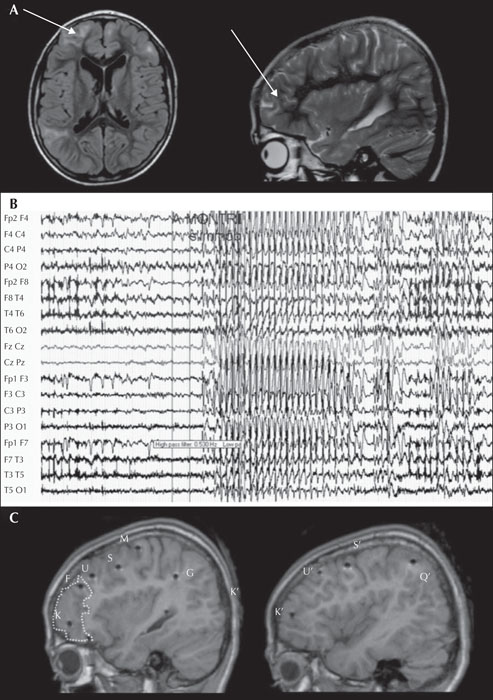
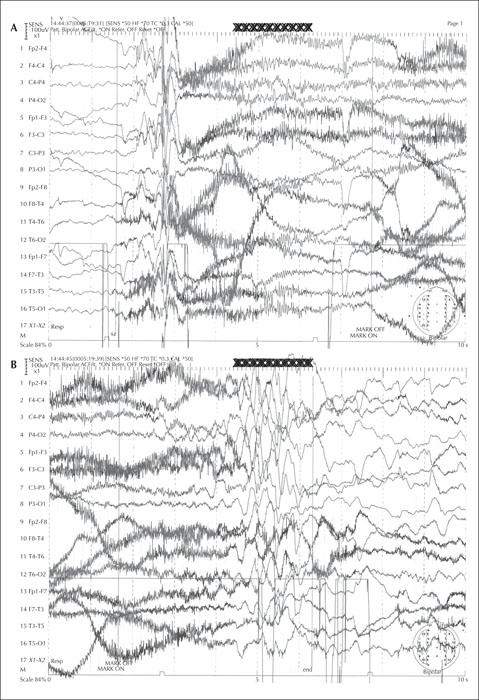
Electrophysiological (EEG) studies are useful supporting tools in the differentiation between focal and generalized seizures and also to define the type of focal or generalized epilepsy [33, 34]. For example, absence epilepsy exhibits a 3-Hz spike and wave, juvenile myoclonic epilepsy exhibits generalized spikes and photosensitive response evident in a third of affected people, epileptic spasms show the classic hypsarrhythmia, and so on (figures 1-6). When delineating between myoclonus and spasm events, attachment of electromyography (EMG) surface leads aids monitoring of the period of muscle activity correlating to the duration of the event. If the awake EEG is normal, then proceeding with a study in natural sleep, often enhanced by preceding sleep deprivation, can be useful. An EEG with normal background activity is not useful to differentiate between seizure subgroups [6]. If diagnostic doubt remains as to whether the events are ictal or not, or focal and generalized cannot be distinguished, then admission for vEEG prolonged recording can sometimes resolve this, as this tool is the gold standard intervention to support a diagnosis. Whilst this is time-consuming, costly and often inconvenient for the person with events and their caregivers, correct event delineation early in the disease course permits accurate diagnosis and management, avoiding the unnecessary legacy of mistreatment. Juvenile myoclonic epilepsy can manifest with focal myoclonic jerks leading to misdiagnosis of focal epilepsy; in this setting, vEEG capturing of ictal events is invaluable to delineate the process [35].
Care must be taken in the interpretation of the EEG as some people with generalized seizures are still able to generate independent focal interictal discharges, and focal discharges do not always correlate to the anatomical localization of the epilepsy [36-39]. This is common in patients with juvenile myoclonic epilepsy and juvenile absence epilepsy [40] (figure 3). In addition, incidental focal discharges are not uncommon in the general population. Surface electrode ictal recordings can be challenging if the propagating focus is deep as this can result in the appearance of asymmetry in the surface electrodes with an apparent focal “take-off” suggesting a focal onset to the event. Paradoxically, a deep focus can also result in the appearance of generalized activity on the ictal recording as the focal generating network is not detected until bilateral synchrony has occurred (figure 4).
What is the role of neuroimaging in differentiating between focal and generalized seizures?
Neuroimaging is recommended by the ILAE Epilepsy Neuroimaging Task Force [41]. This can assist with anatomical location of seizure focus, as well as understanding aetiology, treatment implications and prognosis. The study by Baykan et al. found that, in the setting of minimal motor seizures with loss of awareness, MRI for generalized seizures is usually normal but for patients with focal seizures, abnormalities are often identified [6]. However, as with EEG, neuroimaging should not be used as the only tool to differentiate between focal and generalized seizures but rather a supporting aid. Other neuroimaging tools can be useful, especially in MRI-negative cases with suspected focal pathology, these include positron emission tomography (PET) and single-photon emission computer tomography (SPECT) [42].
Other aetiology-driven investigations
Well-defined seizure semiologies can lead to targeted investigations for genetic, metabolic and immune aetiologies and result in precision medicine management. For instance, faciobrachial dystonic seizures are almost pathognomic of limbic encephalitis associated with LGI1 antibodies [43]. In young adults, association of primary generalized tonic-clonic seizures, myoclonus, new-onset cerebellar ataxia and slight cognitive impairment should result in genetic testing for type 1 progressive myoclonic epilepsy.
What are the pitfalls and how can one avoid them? (table 4)
Clinical history
Focal-onset seizures can evolve into bilateral tonic-clonic seizures and if the start of the event is not witnessed then the clinician may be misled into believing that the event is the clinical expression of a generalized epilepsy. On the other hand, focal seizure symptoms, as well as focal EEG abnormalities, can manifest in primary generalized epilepsies and be misleading [14] (figure 3).
Age at presentation
Age can complicate the delineation of focal from generalized seizures. Young children may be unable to express sensory symptoms, and as such, events from the temporal lobe, for example, are easily missed and under-reported [44]. Further brain maturation can influence the manifestation of seizure events, and generalized tonic-clonic seizures do not manifest in infants until adequate myelination has occurred, usually after 12 months of age [45]. In line with brain maturation time windows, an infant may manifest with epileptic spasms related to an underlying structural focal pathology. The spasms in this setting may be focal, but not always. As people with epilepsy age, the manifestation of events may vary and other co-morbidities can compound the recognition of seizure types, for example, distinction between early stages of dementia and focal seizures in the elderly, and notably transient epileptic amnesia that might be difficult to identify and require targeted investigations [46, 47].
Antiseizure medication
ASMs can also complicate the manifestation of seizures, for example, children with focal seizures, which may be syndromic (namely self-limited childhood epilepsy with centrotemporal spikes or Lennox-Gastaut syndrome), are often managed with lamotrigine as add-on therapy but this can exacerbate or bring out myoclonic seizures in some patients, leading the clinician to question the original diagnosis [48]. Further, self-limited epilepsy of childhood with centrotemporal or occipital spikes in children may evolve into encephalopathy with status epilepticus during sleep (ESES) when treated with carbamazepine, phenobarbital or phenytoin [49].
Seizure mimics
Childhood absence epilepsy can commonly mimic the loss of awareness reported in sensory focal seizures [12]. Clinicians may not be aware that simple automatisms are common during childhood and juvenile absence epilepsy. In this setting, children are placed on carbamazepine and suffer exacerbation of their absence epilepsy or myoclonus [50]. This is an important illustration of how relevant the clinical history is to clarify the difference in the two settings. In comparison to sensory focal seizures, absence events exhibit abrupt onset and termination, duration of less than 30 seconds and no post-ictal confusion. Juvenile myoclonic epilepsy is another condition often misdiagnosed as focal epilepsy, especially as asymmetrical myoclonic jerks are not infrequent [51, 52].
Co-morbidities
Children or adults with co-morbidities, inclusive of tics, anxiety, intellectual disability and autism spectrum disorder, can have an overlay of additional movements, behaviours and compromised expression which can further challenge delineation of seizure semiology. The diagnosis of patients with psychogenic non-epileptic seizures can be extremely challenging and these events can co-exist in the setting of epilepsy as well [53-56].
Conclusion
The differentiation between generalized and focal seizures remains a clinical process based on meticulous clinical history and examination. EEG, neuroimaging and other investigations (genetics, immune markers, etc.) can support the outcome but distinction between focal and generalized epilepsy in isolation is rarely achieved using such techniques. Certain clinical settings such as age, underlying aetiologies, and co-morbidities will be more predisposed to specific types of epilepsy, but again this is a guide and not a fixed modality.
Key points
- •The key tools to differentiate focal from generalized epilepsy is clinical history and examination
- •EEG can be misleading with incidental focal discharges reported in generalized epilepsy
- •Young children may not be able to report sensory features of seizures leading to under-reporting in this age group
- •Co-morbidities can compound delineation of ictal events.
- •It is important to keep an open approach and to repeat the clinical history and description of the events often.
Supplementary material
Summary slides accompanying the manuscript are available at www.epilepticdisorders.com.
Disclosures
None of the authors have any conflicts of interest to disclose.
Case 1 (generalized versus focal)
A nine-year-old boy, John, presented to the emergency department one hour after “an event” in the early hours of the morning. His previous medical history was unremarkable and he was not on any regular medications. He attended mainstream education.
On direct questioning, his parents remembered that he had a “funny turn” last year. He had no neurocutaneous skin lesions and was not dysmorphic. He is right-handed, fully orientated with a normal systemic and neurological examination.
His parents reported that he walked into their bedroom and appeared upset. They thought he was sleepwalking as he appeared awake but did not respond to them when they spoke to him. They noticed that his face was skewed to the left side. Shortly after this, his left arm and leg became stiff and he fell to the floor. His eyes remained open, he did not appear to “see” them or respond to them, and his left limbs started to twitch. His parents struggled to remember the duration of the abnormal movements but when provided with relevant defined time points, e.g. based on the duration of a radio news broadcast, they felt that this was no more than three minutes. As the movements slowed and stopped, John interacted appropriately (naming family members, oriented in time and place, and moving all limbs equally). He slept on the way to the hospital. On arrival he had returned to his normal state.
John said he felt completely well before going to bed, and denied being on his electronic devices before sleep. He awoke before his alarm clock normally woke him, and felt that “something was wrong”. Although he could understand what his parents said to him, he could not talk. The event was identical to the episode that occurred the previous year. He heard his mother say that his face looked odd but he had no memory of when he fell down. When he woke up, he knew where he was and he felt completely well at the hospital.
An EEG two weeks later recorded centrotemporal spikes over his right hemisphere which became bilateral when he entered natural sleep. His parents requested a “brain scan”, however it was explained that this is not indicated in the setting of the history, the clinical examination and the EEG findings.
John and his parents are counselled based on a diagnosis of a form of epilepsy which is termed “self-limited epilepsy in childhood with centrotemporal spikes”. The self-limited nature of the epilepsy means that antiseizure medication is not essential for his care and quality of life. However, if John or his parents feel that they would be more comfortable with medication, then these events usually respond well to carbamazepine.
Case 2
Adele is a 47-year-old Chinese patient who was referred to a tertiary epilepsy centre in 2015. Her main antecedent was a thyroid cancer that was operated on in 2004. A few months after, at the age of 36, she reported the appearance of brief episodes of loss of contact. She described a sudden arrest of her current activity. There was no subjective symptoms. No other symptoms were observed by the witnesses during the episodes, which lasted about 10 seconds. She did not report suffering from myoclonus. The initial inter-ictal EEGs showed bilateral and synchronous spike-waves discharges but also, at least on one EEG, left temporal slow waves. Brain MRI was normal. Overall, the diagnosis of epilepsy was made, but without a precise syndromic diagnosis. Sodium valproate was initiated. The seizures were initially controlled but the treatment was poorly tolerated. The neurologist who followed her then replaced this with gabapentin. After initial improvement, the situation remained difficult with frequent seizures. Carbamazepine was also tried without efficacy and resulted in a rash. Gabapentin treatment was then resumed and the dose was gradually increased over the years despite the persistence of seizures.
Considering the situation when she was referred to the tertiary centre, a long-term video-EEG was organized in order to better characterize the syndromic diagnosis. This showed seizures characterized by isolated loss of contact associated with bilateral and synchronous 3-4-Hz spike-wave discharges. No focal EEG abnormalities were observed. MRI was repeated and remained normal.
In this context, gabapentin was stopped and the choice of antiseizure medication was made exclusively towards broad-spectrum agents. After she developed depression on levetiracetam, in combination with sodium valproate at a small daily dose, for tolerability, zonisamide was tried. The patient is currently free of seizures and her long-term EEG monitoring is normal.
In this patient, the initial issue was a difficulty in making a syndromic diagnosis. Although the picture remains atypical because of the age at epilepsy onset, many elements are present to consider that this epilepsy fits into the spectrum of idiopathic generalized epilepsy. This reorientation of the syndromic framework made it possible to better target treatment options and avoid maintaining pseudo-pharmacoresistance.
![]() This work is licensed under a
Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License
This work is licensed under a
Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License