Epileptic Disorders
MENUAn audit of the predictors of outcome in status epilepticus from a resource-poor country: a comparison with developed countries Volume 18, issue 2, June 2016
Status epilepticus (SE) is a life-threatening neurological emergency with significant morbidity and mortality. The underlying aetiology is considered the most important prognostic factor determining outcome (Neligan and Shorvon, 2010). Both clinical studies and experimental data have shown that the duration of SE before initiation of treatment and time required to control SE strongly influences outcome (Towne et al., 1994; Mazarati et al., 1998; Neligan and Shorvon, 2011). Age, level of consciousness at the time of admission, previous history of seizures, and EEG findings are some of the other variables shown to determine the outcome of SE (Neligan and Shorvon, 2011).The aetiology and time gap between onset of SE and initiation of treatment significantly differs in developing countries as compared to the western world (Mhodj et al., 2000; Murthy et al., 2007; Sinha et al., 2010).
In this context, with only limited data available in the literature from the developing world, we conducted this study to assess the clinical profile, treatment, and predictors of outcomes of SE, both convulsive (CSE) and non-convulsive (NCSE), in a tertiary care centre which has a comprehensive epilepsy care programme in India, and aimed to highlight the similarities and differences of data available from the western world.
Methods
All patients treated for SE, both CSE and NCSE, between January 2000 and September 2010, were included based on prospectively maintained records. Patients who developed SE in the epilepsy monitoring unit during video-EEG monitoring and those with febrile SE were excluded. Patient data comprising of demographic details, clinical features, investigations (including neuroimaging and EEG), treatment details, and in-hospital outcomes were collected utilising a structured proforma and were compared with data available from the western world.
Definitions
SE was defined as a condition resulting either from failure of the mechanism(s) responsible for seizure termination or from initiation of mechanism(s) that lead to abnormally prolonged seizures, lasting at least five minutes. It is a condition, which can have long-term consequences (especially if it lasts more than 30 minutes), including neuronal death, neuronal injury, and alteration of neuronal networks, depending on the type and duration of seizures (Trinka et al., 2015).
Refractory SE (RSE) was defined as status that does not respond to initial anticonvulsant treatment with at least one first-line intravenous (IV) antiepileptic drug (AED), benzodiazepines and one or more second-line AEDs, and requires general anaesthetic agents regardless of the delay from the onset of the seizure (Shorvon and Ferlisi, 2012).
Super refractory SE (SRSE) was defined as SE that continues or recurs 24 hours or more after the onset of anaesthesia, including those cases in which SE recurs during reduction or withdrawal of anaesthesia. (Shorvon and Ferlisi, 2012).
Aetiology
Aetiology of SE was classified as acute symptomatic (AS), progressive symptomatic (PS), remote symptomatic (RS), or unknown aetiology (UE), according to the International League Against Epilepsy (ILAE) recommendations (Commission on Epidemiology and Prognosis, 1993). SE was considered “AS” when it occurred within a week of acute central nervous system (CNS) or systemic insult (i.e. stroke, neuro-trauma, meningitis, hepatic encephalopathy, or alcohol intoxication or withdrawal) (Beghi et al., 2010); “PS” when it occurred as a result of non-static CNS conditions (i.e. CNS tumours, or degenerative neurologic diseases); and “RS” when a CNS insult in the past was presumed to result in a static encephalopathy associated with an increased risk of epilepsy (i.e. stroke, head trauma, cerebral palsy, or encephalitis). The classification “UE” covers subjects with epilepsy of unknown cause.
Treatment
The sequence in which AEDs were administered, including dose and duration (in case of continuous infusion), control of seizures, and development of adverse effects were all noted.
All patients with SE (CSE and NCSE) were treated as per a standard protocol, devised by our epilepsy care team according to the recommendations by the ILAE.
- –0-5 minutes from recognition of SE: first-line AEDs, i.e. short-acting benzodiazepines (lorazepam, midazolam or diazepam) were administered;
- –5-30 minutes: second-line AEDs, i.e. non-anaesthetic drugs (phenytoin, valproate, phenobarbitone, levetiracetam or topiramate) were administered;
- –30-60 minutes: additional second-line AEDs were administered;
- –>60 minutes onwards: patient was intubated, third-line (midazolam) and fourth-line (propofol or thiopentone) continuous IV anaesthetic agents were administered.
Outcome
The outcome was classified as:
- –return to baseline;
- –development of new disability (neurological deficit/epilepsy);
- –death.
The outcome was defined at the time of discharge and at subsequent follow-up visits, up to one year. The development of disability or death was grouped as “poor outcome” and achievement of pre-SE functional status was defined as “good outcome”.
Statistical analysis
Data were expressed using descriptive statistics as mean±standard deviation (SD) for continuous variables and frequency and percentage for categorical variables. The patients were grouped according to outcome into “good outcome” and “poor outcome”. The prognostic variables were compared between the two groups. Continuous and discrete variables were assessed using the Student's t-test and the Chi square test or Fischer's exact test, respectively. The factors shown to be significant in univariate analysis were further ascertained by a step-wise multivariate regression analysis. A p value <0.05 was considered statistically significant. Statistical analysis was performed with SPSS version 17.0 statistical software (SPSS Inc., Chicago).
Results
During the study period, a total of 129 events were identified from computerised prospectively maintained medical records using an ICD-9 code. An additional seven cases were identified based on a search for discharge or death. Twenty-eight events (supplementary figure I) were excluded from the analysis as they did not fulfil the inclusion criteria for SE: no conclusive SE (n=8), epilepsia partialis continua (EPC; n=2), and medical records could not be retrieved or important variables missing or lost to follow-up (n=18). A total of 108 events in 84 patients, comprising of 64 adults and 20 children, were analysed in detail. Single episodes of SE were treated in 72 (86%) patients and 12 were treated for multiple events, ranging from two to six events per patient. The mean age at admission was 24.1±20.3 years and 63% patients were males (table 1).
SE in patients with epilepsy
The characteristics of patients (n=65) with a history of epilepsy are presented in table 2. The age at onset of epilepsy in these patients varied between three months and 65 years of age. Frequent seizures (>one/week) were noted in 25% (n=16). All, but one patient, were on AEDs and 20% were on poly-pharmacy (
Aetiology
Thirteen patients (15.7%) had an acute symptomatic SE (table 1). Aetiologies included: encephalitis (n=6), menigoencephalitis (n=4), metabolic (n=1), hypoxic ischaemic encephalopathy (n=1), and unknown (n=1). In patients with a history of epilepsy (table 2), remote symptomatic aetiology was commonest (60.7%). Among remote symptomatic aetiology (n=51), epilepsy due to gliosis/scarring related to perinatal insult (hypoxia, hypoglycaemia, neonatal CNS infection, perinatal ischaemic event, or bleeding) constituted the majority (36.9%), and was the predominant cause in children (n=16). Gliosis due to stroke(n=5), atrerio-venous malformation bleeding (n=2), and trauma (n=1), accounting for 12.3%, were found exclusively in adults. Focal cortical dysplasias accounted for 4.6% cases of RS nature. Progressive symptomatic aetiology was documented in 8.3% (n=7), five of whom had CNS neoplasms and two progressive myoclonic epilepsy. In 13 patients, aetiology remained unknown. De novo SE occurred in 19 patients, and included all cases of AS, four with RS (two cases of post-stroke seizure, two cases of post encephalitis sequelae, and one case of birth asphyxia), and one patient with PS status (brain tumour).
EEG findings
EEG was performed for all patients and continuous EEG (cEEG) during 97 SE events (89.8%). EEG was performed during all RSE events (n=23). Fourteen (61%) RSE patients underwent cEEG monitoring until seizures were abated totally, and in others, frequent intermittent EEG (for at least eight hours a day) was performed. In 85 (87%) events, EEG was performed within 24 hours of hospitalisation, and for 31 of these (32%), within six hours of admission. Interictal epileptiform abnormalities (IEDs) were the most common EEG abnormality noted in 80 (82%) of the events and these were the only EEG abnormality noted in 41 (42%) events. Discrete (clinical/electrographic) seizures were noted in 12 (12.3%), periodic epileptiform abnormalities in seven (7.2%), NCSE in three (3%), and SE in three (3%). EEG showed suppression during six events (6%). Only non-specific slowing was noted in 12 (12.3%) events and five (5%) EEGs during SE were essentially normal.
Treatment
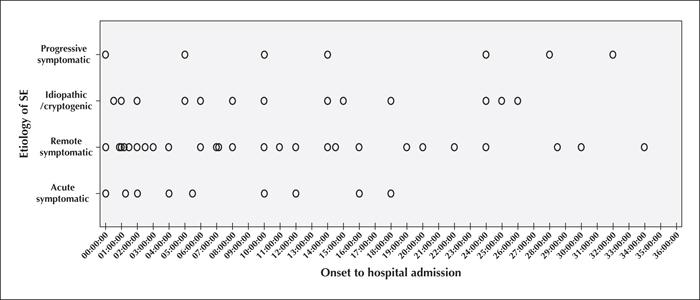
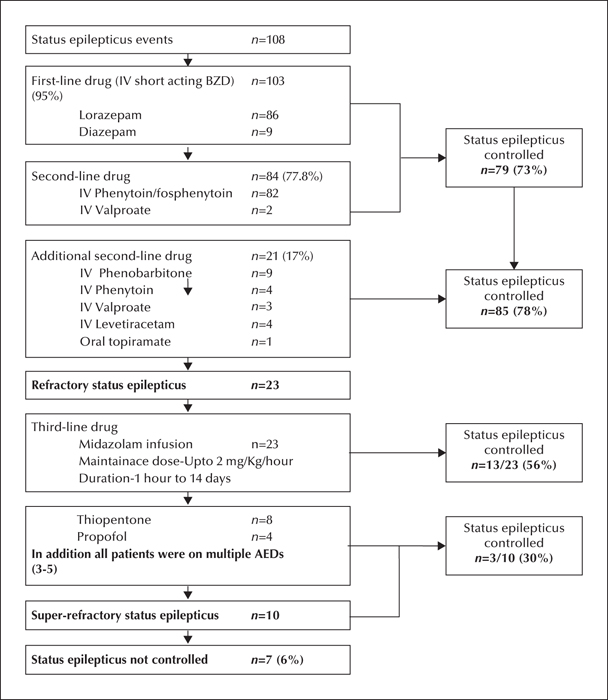
The mean time from onset of SE to initiation of management was 12.8 hours (1-72 hours) (figure 1). The SE management was initiated outside our hospital in 58% of the events. In 103 (95%) of the events, SE management was started with IV benzodiazepines. Among these, in 86 (80%) events, lorazepam was used. Second-line medications were administered in 84 (77%) of the events and additional second-line drugs were used in 21 (17%) events. With first and second-line medications, 79 (73%) SE events were controlled, and the control of SE events increased to 85 (78%) after administration of additional second-line agents. In three patients, phenytoin was temporarily stopped due to hypotension (n=2) and generalized itching (n=1). In 23 (21%) events, the control was not achieved with these AEDs, and was labelled as RSE. Thirteen (56%) RSE events were controlled with continuous IV midazolam infusion. In 15 (66%) events, midazolam infusion was stopped within 24 hours, either due to control of SE (n=10), development of adverse effects (n=3), or change to another anaesthetic agent (propofol/thiopentone) (n=2). Ten events (10%) were SRSE. Only three out of ten SE (30%) events, which were not controlled with midazolam, could be controlled with fourth-line AEDs (thiopentone/propofol). Hypotension not responding to conventional treatment and requiring modification or discontinuation of thiopentone occurred in four (50%). All four patients who received propofol had serious side effects, such as hypotension (n=2), severe metabolic derangement (n=1), and cardiac arrhythmia leading to death (n=1). Seven events of RSE could not be controlled.
For the treatment of SE in the paediatric age group, other treatment modalities tried were pyridoxine in two cases of cryptogenic SRSE and magnesium in two cases of suspected mitochondrial cytopathy. The ketogenic diet was tried in three children with SRSE, however, it failed to control SE and children developed severe adverse effects that included aspiration pneumonia, constipation, gastroesophageal reflux, and in one case caused fulminant pancreatitis and was thus discontinued. The treatment administered and the results obtained are summarised in figure 2.
The mean hospital stay was 7.8±16.6 days (1-130 days). Ninety-five (88%) events were managed in the neuro-medical intensive care unit (ICU), four (4%) in the neuro-surgical ICU, one (1%) in the cardiology ICU, and the remaining eight (7.4%) in well-equipped neurology wards. The mean ICU stay was 6.2 days. In 39.8% of the events, ventilator support was required and in the majority (77%) of the events, patients were weaned off within 72 hours. Medical complications developed in 23 (21%) events and in four (4%) resulted in death despite control of SE that included refractory hypotension (n=2), sepsis with multiple organ dysfunction syndrome (n=1), and disseminated intravascular coagulation (n=1).
Outcome
The outcome of 108 SE events were analysed (supplementary figure II). Seventy-two events (66.7%) could be effectively treated and patients had “good outcome” in the form of returning to baseline. Thirty-six events (33.3%) had “poor outcome” in the form of development of disability or death.
Development of new neurological deficits following control of SE was noted after 24 SE events (22%); cognitive dysfunction in 11, motor deficits in three, and global deficits in the remaining 10. A total of 12 patients died (11 deaths/100 events), and mortality was 46% (n=6) in AS SE, 37.5% (n=3) in PS, and 2.8% (n=2) in RS.
Aetiology was the most important predictor of poor outcome (p<0.001) (table 3). In the AS group, 12 out of 13 had either new disability (n=6) or death (n=6). Patients who developed RSE had poor outcome compared to those in whom the status was controlled with first and second-line medications (p<0.001). Age at presentation was found to be another predictor of outcome, unrelated to aetiology. Children had better outcome, compared to adults (p=0.05). The poor outcome group had a mean age of 27.2 years, compared to a mean age of 18.4 years in the good outcome group (p=0.05). Treatment delay was also found to affect outcome. Mean delay in the initiation of treatment in the poor and good outcome groups was 24.1 and 9.3 hours, respectively (p=0.03). Gender and EEG abnormality was not found to be significant. Level of sensorium (GCS) at the time of ICU admission was found to influence the outcome in univariate analysis, but significance was lost in multivariate analysis (p=0.1).
Discussion
The outcome of SE reported in various studies worldwide is variable and a mortality rate of 5 to 56% is reported (Logroscino et al., 2005; Maharaj et al., 1992; Tsai et al., 2009; Cook et al., 2012). The differences in the demographic factors, aetiologies, and treatment variables are likely to be responsible for the heterogeneity in outcome noted. The aetiology of SE (Neligan and Shorvon, 2010) and the severity of the underlying disease (Rossetti et al., 2007) are the most consistent determinants of outcome. Age and sensorium at presentation are the other two prognostic variables that are invariably noted to influence outcome (Neligan and Shorvon, 2011).
The cohort reported from the developing world significantly differs from the developed world (Neligan and Shorvon, 2011). Infectious aetiology accounts for the majority of cases of SE in developing countries (Visudtibhan et al., 2006; Murthy et al, 2007; Chen et al., 2009; Sinha et al., 2010). However, in our series, remote symptomatic aetiology accounted for the majority of cases, but morbidity and mortality were noted to be higher in acute symptomatic SE compared to patients with remote aetiology (table 3).
We found that treatment delay was significantly higher in this part of the world (Mhodj et al., 2000; Murthy et al, 2007; Sinha et al., 2010). Only three patients (2.8%) reported for treatment within 30 minutes of SE, 9% within an hour, and 28% within three hours. A mean delay of 12.8 hours before the start of the treatment was noted in our cohort. Time delay (>one hour) in the initiation of treatment, relative to less than one hour, was a predictor of poor outcome in western countries, with an odds ratio of 9.79 (DeLorenzo et al., 1995) and 17.9 (Towne et al., 1994). Experimental data suggest that the risk of developing treatment refractoriness and poor outcome is higher with prolonged untreated SE (Kapur and Macdonald, 1997). In contrast, the duration of SE did not influence outcome in some studies (Logroscino et al., 1997; Rossetti et al., 2006a). After the initial few hours, duration of SE may become a less reliable predictor of outcome (Drislane et al., 2009). Despite significant delay in initiating SE management in our series, the incidence of RSE and case fatality is comparable with other cohorts (Novy et al., 2010), and even less than that reported in some other series (Mayer et al., 2002), with the majority of patients responding to the standard SE management. Similar observations were made by several authors in resource-poor countries where treatment delay is universally reported (Murthy et al., 2007; Amare et al., 2008). There are reports of good outcome following prolonged SE (Standley et al., 2012). However, these findings cannot be used to justify less emergent management of SE, and every possible step to terminate ongoing SE needs to be taken. However, prolonged SE or treatment delay should not always be considered a hopeless situation.
A substantial proportion of patients remain responsive to medications despite a delay in treatment and thus cannot be termed “refractory” until they are given an adequate supervised trial of antiepileptic drugs. The RSE definition should be based on failure of medicine trials (Jagoda and Riggio, 1993) rather than time-based (Stecker et al., 1998; Prasad et al., 2001). Shorvon and Ferlisi have defined RSE as “status epilepticus requiring general anaesthesia” (Shorvon and Ferlisi, 2012). This definition is more logical and practical. The diagnostic labelling of RSE is not only important for prognostication, but also implies more intensive medical care with higher risk of medical complications and adverse effects due to anaesthetic agents.
As per the practice guidelines at our centre, midazolam is the initial choice as the anaesthetic agent for management of RSE. There is little evidence to choose between midazolam, propofol, and thiopentone, and all have shown comparable efficacy. In our series, thiopentone and propofol were tolerated poorly, compared to midazolam, and additional benefit with thiopentone/propofol was noted only in a few patients who failed midazolam. The published guidelines do not recommend one anaesthetic agent over another because of the lack of evidence of efficacy or tolerability in comparative data (Meierkord et al., 2010). Barbiturates are reported to have a higher success rate in achieving burst suppression and cause least breakthrough seizures (Claassen et al., 2002).
The available evidence does not provide any distinct advantage of aggressive burst suppression in EEG over control of seizures in terms of short or long-term outcome (Rossetti et al., 2005). The aggressive control of NCSE may not always translate into better outcome (Ferguson et al., 2013) and it has the potential to adversely affect outcome due to prolongation of mechanical ventilation, causing hypotension and other medical complications (Kowalski et al., 2012). The incidence of adverse events requiring termination of therapy and death during therapy was reported to be highest with barbiturates and lowest with the midazolam group (Shorvon and Ferlisi, 2012). Propofol infusion syndrome remains one of the major drawbacks for patients requiring prolonged infusion (Iyer et al., 2009). Due to the relatively better tolerability of midazolam and lack of evidence showing any definite benefit of achieving burst suppression versus control of seizures, we continue to prefer midazolam over thiopentone/propofol as initial management of RSE. Based on our data, we have formulated a pragmatic protocol for management of SE (supplementary figure III).
In our study, in addition to aetiology and treatment delay, older age and absence of past history of epilepsy adversely affected outcome. This finding is in agreement with earlier studies from the West (Rossetti et al., 2006b; Neligan and Shorvon, 2011). Sensorium at the time of ICU admission was not found to be a significant predictor in multivariate analysis. The aetiology per se influences the sensorium level which can become further confounded by drug administration prior to admission. Also, the emergent EEG data failed to provide prognostic information in our study, but is helpful in the management of non-refractory and refractory SE patients, as noted previously by us (Firosh Khan et al., 2005). The majority of patients need only a short ICU stay and ventilatory support.
Of all those with epilepsy, around 80% live in resource-limited countries and up to 90% of these patients receive no treatment at all (Caraballo and Fejerman, 2015).There are a number of impediments to appropriate and satisfactory management of epilepsy in general, particularly of SE, in many of the developing countries, where the inadequacy of the available resources poses a major obstacle. These factors have been variably noted to include unmanageable treatment costs, lack of access to newer AEDs, and in certain settings, a steady supply of even first-line agents, and physicians being solely dependent on clinical findings due to non-availability of imaging and electrophysiological modalities (Caraballo and Fejerman, 2015). In our study setting, in the southern-most state in India, though the per capita income places the state among the lowest in the country, other health, educational, and developmental indices place it among the best in the country and it is sometimes commended as being comparable to western standards. A combination of social and cultural factors and focused, committed bureaucratic impetus, even in the face of severe limited resources, are among the reasons for this. The fact that treatment had been initiated in 58% of patients in another centre before arrival to our institute augurs well, particularly for a system which lacks coordinated emergency and paramedical services that initiates out-of-hospital treatment.
This study is limited by its retrospective nature. Being a tertiary referral centre, our data are expected to over-represent refractory patients which, in turn, can influence morbidity, mortality, and refractoriness ratios. The outcome of return to “baseline state” versus “neurological deterioration” based on patient charts has its limitations. However, significant worsening is unlikely to be misclassified.
The reasons for treatment delay could not be studied. In developing countries, the lack of public awareness, absence of prompt availability of medical care, lack of infrastructure to transport to appropriate centres, and lack of expertise to recognise NCSE are likely reasons for treatment delay. A coordinated effort to train the populace as well as general physicians, at the grass root level, in early recognition, treatment initiation, and early referral should be undertaken. Despite its limitations, our study provides valuable information regarding the outcome of a sizeable number of patients based on standard protocol-driven management, which in turn may be crucial to set up standards of care for the management of SE in developing nations.
It can be concluded that, as is the case in the western world, aetiology is also the most important prognostic factor in resource-poor nations. A significant treatment delay may not necessarily imply a grave outcome, but may influence the outcome.
Supplementary data
Supplementary figures are available on the www.epilepticdisorders.com website.
Acknowledgements and disclosures
This work was not supported by any grant.
None of the authors have any conflict of interest to disclose.