European Journal of Dermatology
MENUPost-surgery morphea mimicking relapse of breast cancer Volume 32, issue 5, September-October 2022
Figures
Locoregional cutaneous manifestations of breast cancer are common and have a heterogeneous appearance, including infiltrated eczematous plaques. For this reason, the clinical differentiation from scleroderma-like manifestations remains difficult. Breast morphea is a rare condition, usually reported as a complication following adjuvant radiotherapy of breast cancer [1–3]. Here, we present a woman with localized scleroderma arising after surgery on a non-implanted, non-irradiated breast.
A 52-year-old Caucasian woman presented with a five-day history of tension pain on her left breast. Two weeks before, she had undergone retroareolar quadrantectomy for an infiltrating Stage pT1C ductal breast carcinoma on the left side. Adjuvant radiotherapy was scheduled to begin in four weeks.
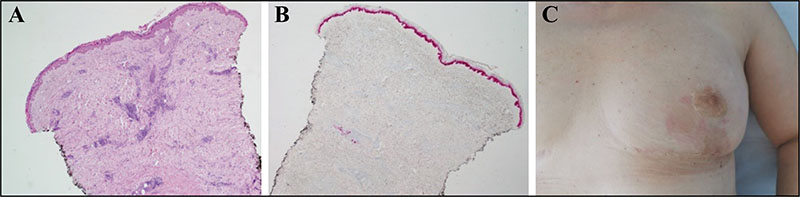
Physical examination showed a peri-areolar brownish-erythematous plaque with puckered skin on the quadrantectomy scar. At first, acute mastitis or breast cancer relapse were suspected. Routine blood analysis (CA 15.3 [1 U/mL] and CEA [0 ng/mL]) was within normal limits. Breast ultrasound was also unremarkable. Skin biopsy was performed on the lesion. Microscopic examination revealed thickened dermal bundles and a CD3/CD4/CD8+ lymphocytic perivascular infiltrate. Immunohistochemistry for pan-keratin (AE1/AE3) showed no evidence of an epithelial neoplasia (figure 1A, B). All initial diagnostic hypotheses were gradually ruled out and the diagnosis of localized morphea of the breast was made. Topical clobesol was prescribed, with clinical improvement. To reduce the risk of cancer recurrence, the patient underwent adjuvant radiotherapy (35 Gy/10 Fx). No skin complications appeared following irradiation.
Three months later, approximately 15 days after a follow-up mammography, the patient presented with a recurrence of skin symptoms. At clinical examination, the periareolar skin reappeared hardened, erythematous and infiltrated (figure 1C). Tumour markers remained within normal limits. Breast magnetic resonance imaging was performed and showed neither signs of mastitis, nor tumour relapse. An incisional skin biopsy was repeated. Microscopic examination confirmed the histological report of the previous punch biopsy, showing no neoplastic changes. The diagnosis of morphea was thus confirmed. Prednisone (0.75 mg/kg) and topical pimecrolimus where initiated. Mycophenolate mofetil at 500 mg bd was added due to ineffectiveness of steroid therapy alone. Four months later, the patient showed complete remission and reported optimal tolerability. Immunosuppressant therapy was suspended after tapering over two months.
As far as we know, this is the second report of localized scleroderma arising after surgery on a non-implanted, non-irradiated breast [4, 5]. In our patient, the surgical trauma was likely the main triggering factor; in addition, compression of the diseased area during mammography could be a precipitating factor for morphea relapse. In fact, studies on the pathophysiology of fibrosis have shown that recurring or chronic trauma increases the regulation of endogenous toll-like receptor ligands, thereby inducing a fibrogenic self-amplification loop [6].
Radiotherapy is known to correlate with both the induction of sclerodermatous skin changes and their precipitation. It has been shown that such fibrotic mechanisms induced by ionizing radiation can induce morphea-like manifestations, even in the long term [7]. However, in our patient, the onset of morphea prior to the initiation of radiotherapy excludes the latter as a triggering factor.
Despite the rarity of breast morphea cases, most of which have been described following radiotherapy, we believe that dermatologists and physicians managing these patients should be aware of it and promptly initiate the differential diagnostic process, which includes surgical-site infection, lymphoma or primary cutaneous disease. Patients should be informed of the possibility of this rare complication and reassured of its benign nature and the existence of several therapeutic options. Systemic therapies may be necessary when topical therapies are ineffective. In our case, it was necessary to introduce mycophenolate mofetil, in agreement with oncology colleagues, because of the poor response to topical and systemic steroids. Immunosuppressants in patients recently diagnosed with malignancies should be used with extreme caution. However, in our patient, the expected short duration of the therapeutic cycle, the absence of residual neoplastic disease, and the frequent check-ups which the patient was scheduled to undergo, made this therapeutic option viable.
Disclosures
Acknowledgments: none. Funding source: none. Conflicts of interest: none.