Journal de Pharmacie Clinique
MENUA cross-sectional qualitative comparison between the perceptions of physicians and pharmacists of their collaboration in hospital settings Volume 37, issue 3, Septembre 2018
- Key words: Switzerland, interprofessional relations, surveys and questionnaires, needs assessment, comparative study, hospital
- DOI : 10.1684/jpc.2018.0390
- Page(s) : 143-52
- Published in: 2018
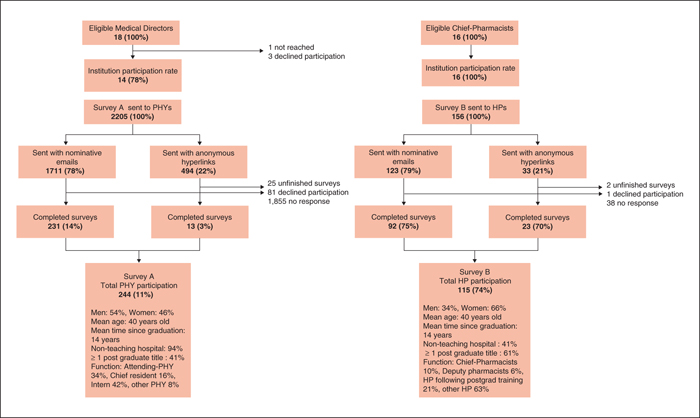
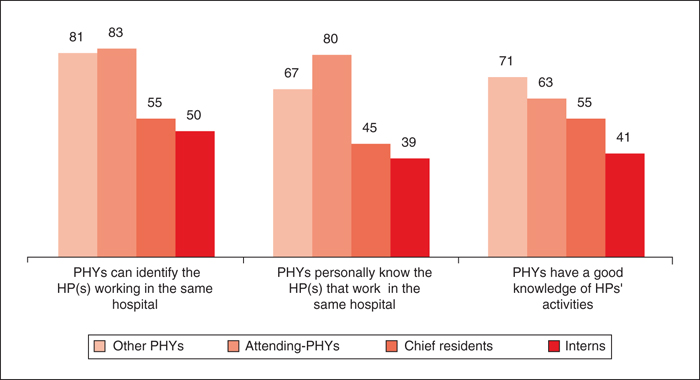
Objective: To identify and compare physician-pharmacist perceptions concerning mutual collaboration in hospital settings. Methods: Two similar questionnaires were emailed to all French speaking physicians and pharmacists working in Swiss hospitals where medical-directors/chief-pharmacists had approved the study. Questions were developed based on previous physician interviews. Results: 14/18 medical-directors and 16/16 chief-pharmacists gave permission for the study. 244 (11%) physicians and 115 (74%) pharmacists answered the surveys. 49% physicians estimated interacting together <5x/year and only 52% contact the pharmacy when they have drug-related questions. Pharmacists considered that there was more contact than this between themselves and physicians. 97% physicians highly value knowing their colleagues, but 39% have trouble identifying pharmacists. 85% physicians would like an increased pharmacist presence in wards. Pharmacists misperceive the importance physicians give to meeting and knowing them. 59% physicians and 87% pharmacists believe physicians need more information about pharmacists’ activities in order to better collaborate. 91% physicians expressed an interest in collaborating with pharmacists and 79% agreed that their current human relations are good. 96% participants consider pharmacists’ global competences to be good. Pharmacist participation during ward rounds is well perceived. Conclusion: Participation rates in the questionnaire give a snapshot of current physician-pharmacist collaboration; pharmacists being the more concerned. Results show an infrequent pharmacist-physician interaction. Physicians’ knowledge about pharmacists’ activities should be improved as understanding one another's professional roles leads to better collaborative relationships. Reasons why physicians do not contact the pharmacist when they have drug-related question should be sought, as poor communication and failure to seek information has been shown to have negative consequences for patients.