Hépato-Gastro & Oncologie Digestive
MENUPancreatic cancer: causes, genetic forms and screening Volume 24, supplement 2, Juin 2017
Université Paris 7, service de gastroentérologie et pancréatologie,
Clichy-La-Garenne, France
- Key words: pancreatic cancer, screening, causes, epidemiology
- DOI : 10.1684/hpg.2017.1445
- Page(s) : 7-17
- Published in: 2017
Pancreatic ductal adenocarcinoma (PDAC) currently accounts for the seventh most frequent cause of cancer worldwide with an increasing incidence. Its prognosis remains very poor with a 5-year survival rate around 5% for all stages taken together.
There are three known precancerous lesions: pancreatic intraepithelial neoplasia, intraductal papillary mucinous neoplasia and mucinous cystadenoma. Evolution towards PDAC is not systematic and acknowledging malignancy features is highly important to avoid useless and dangerous surgery, and conversely, to avoid not to operate high-risk lesions.
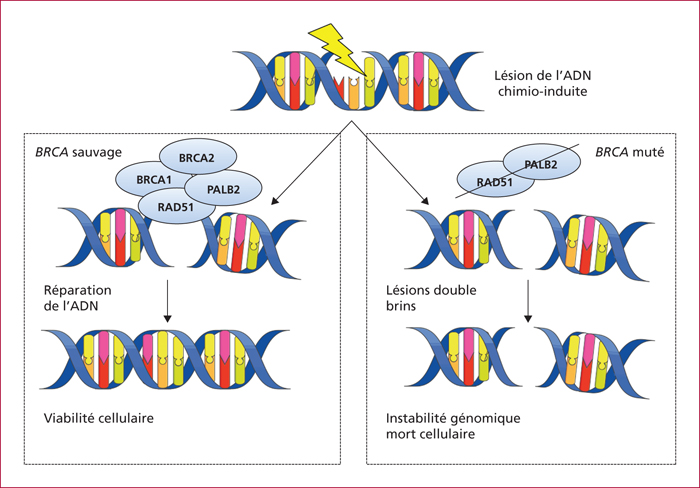
The risk of developing PDAC increases with age, in developed countries, in male subjects and in black individuals. Other risk factors include tobacco, obesity, diabetes mellitus, chronic pancreatitis and PDAC family history. Familial pancreatic cancers account for 5-10% of PDAC cases and are defined by the existence of a PDAC in at least two first-degree relatives. Although no germline mutation is identified in 80-85 %, an increase in the PDAC risk exists in mutation carriers within the BRCA-Fanconi pathway (BRCA1/2, PALB2, ATM, FANC genes) or affected with Peutz-Jeghers syndrome (LKB1/STK11 gene), hereditary pancreatitis (PRSS1 gene), familial multiple mole melanoma (p16/CDKN2A gene) or Lynch syndrome. Identifying these familial PDAC forms is warranted to proposed screening of relatives, prophylactic pancreatic surgery of precancerous lesions, or a therapy targeting molecular biology, such as PARP inhibitors in BRCA1/2 mutation carriers with advanced PDAC.