Hématologie
MENUClostridium difficile Infections and blood disease: what should I know? Volume 21, issue 1, Janvier-Février 2015
- Key words: blood disease, transplant of hematopoietic stem cells, diarrhea, Clostridium difficile
- DOI : 10.1684/hma.2015.0990
- Page(s) : 18-27
- Published in: 2015
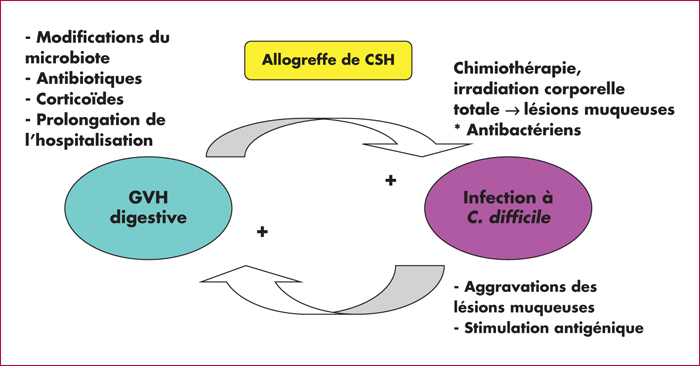
Clostridium difficile infection (CDI) is a major cause of nosocomial diarrhea and is recurrent in approximatively 20% of the cases. Its main risk factors being long hospitalizations and use of antibiotics, haematology patients are especially at risk. CDI is usually the result of a lesion of the gut mucosa combined with changes in local microbiota. New diagnostic tools are now available, looking for Clostridium difficile and/or its toxin that is directly responsible for the bacteria's virulence. Because of their immunosuppression, haematology patients are especially at risk of CDI. There are, additionally, some specificities of CDI in this population: the frequency of co-infection, the inadequacy of the classical severity criteria of CDI in neutropenic patients, and the difficulty to stop or modify antibacterials during febrile neutropenia. Additionally, in allogeneic stem-cell transplant recipients, studies show a significant association between CDI and gut graft-versus-host disease (GVHD). The 2014 therapeutic guidelines of the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) for CDI recommend metronidazole and vancomycin according to the severity of the infection, and also fidaxomycin, a novel antibiotic that looks promising to decrease recurrence rates, as well as fecal transplant which acts directly on the microbiota.