Epileptic Disorders
MENUMyoclonic status epilepticus as a presentation of caspr2 antibody-associated autoimmune encephalitis Volume 16, issue 4, December 2014
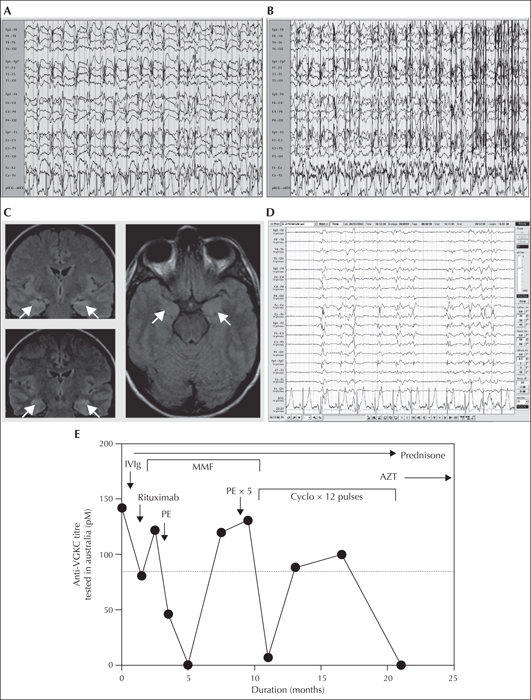
Figure 1
EEG, imaging, and laboratory investigations in a patient with caspr2 antibody-associated autoimmune encephalitis. (A) Day 3: EEG showing generalised periodic spike and polyspike-and-wave discharges. (B) Day 3: EEG showing frequent generalised myoclonic seizures which emerged with attempts to lighten sedation. Electromyographic artefact from the patient's seizure activity obscures the latter part of the trace. (C) Coronal and axial sections of T2 fluid attenuated inversion recovery (FLAIR) sequences on MRI demonstrating subtle bilateral hippocampal hyperintensity compatible with limbic encephalitis (indicated by arrows). (D) This EEG performed on week 2 of presentation demonstrates evidence of induced burst suppression. With attempts to wean off sedation, generalised spike discharges which were maximal centrally can be noted, with clinical accompaniment of myoclonus. (E) Graphical representation of anti-VGKC complex antibody titres (tested in Australia) over time and with treatment. Values above the dotted line (80 pM) are elevated above the normal range. Arrows indicate the timing of institution and duration of therapy. Anti-VGKC titre: anti-voltage-gated potassium channel complex antibody titre; AZT: azathioprine; Cyclo: cyclophosphamide (monthly pulses over twelve months); IVIg: intravenous immunoglobulin (five doses); PE: plasma exchange (five exchanges); MMF: mycophenolate mofetil.

