Epileptic Disorders
MENUGeneralized seizure with falling and unresponsive staring provoked by somatosensory stimulation: a video-EEG study Volume 17, issue 3, September 2015
Reflex seizures are characterized as seizures provoked by highly specific stimulations such as photic stimulation, auditory stimulation, hot-water stimulation, reading, and eating (Kasteleijn-Nolst Trenité, 2012; Striano et al., 2012; Italiano et al., 2014). Somatosensory stimuli, such as skin friction and touching of specific cutaneous regions, as well as brushing the oral cavity, may also provoke seizures; these are called “somatosensory reflex seizures” (Italiano et al., 2014). Most consist of partial seizures, commonly starting with some sensory aura, followed by tonic seizures without unconsciousness. Here, we report a paediatric case of generalized seizures with abrupt falling and unresponsive staring, provoked by somatosensory stimuli of the face.
Case study
The patient, a 4-year-old boy, was referred to our hospital due to frequent episodes of falling, followed by brief staring. Pregnancy and delivery were normal. The patient had several episodes of breath holding at three months of age and febrile seizures at 2 years. His father appeared normal mentally, but had a history of several episodes of staring associated with eye deviation, lasting for around five minutes. This developed at six months of age, but was not provoked by specific sensory stimuli, and was treated with antiepileptic drugs until 3 years of age. The boy's seizures were initially noticed at 3 years of age, when episodes of staring upwards, lasting for seconds, developed and progressively increased in frequency. Sodium valproate was initially started and clonazepam was added soon after at another hospital, however, seizures were not well controlled. At 4 years of age, he was admitted to our hospital because of frequent episodes of falling, followed by staring with unresponsiveness for around 10 seconds. Most of these staring manifestations were consistently triggered by wiping his entire face with a towel several times, but rarely seen in a spontaneous manner. Seizures did not occur when he himself rubbed his eyelid. Physical and neurological examinations were not remarkable. His development quotient was 58 according to the Japanese Tsumori-Inage developmental scale test, and he was judged to have mild delay in psychomotor development. Brain MRI and interictal cerebral blood flow SPECT imaging using Tc-99m ECD were normal. Somatosensory evoked potentials using medial nerves and visual evoked potentials showed normal values for latency and amplitude of waves.
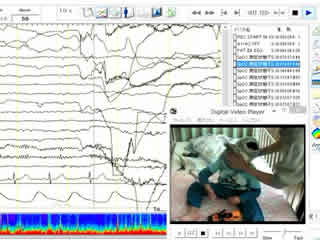
Interictal EEG revealed 3-Hz generalized spike-and-slow-wave complex discharges, lasting for one to five seconds during sleep (figure 1). The background activities during wakeful states consisted of 8-Hz alpha activity in occipital areas, and intermittent photic stimulations, hyperventilation, or eye-closure did not elicit abnormally responsive discharges. Video-EEG recording exhibited ictal manifestations of falling down on the bed and unresponsive staring upwards for around 10 seconds, followed by immediate recovery of consciousness and posture. These episodes were easily provoked by wiping his entire face with a towel. Simultaneous ictal EEG showed 3-Hz generalized spike-wave complex discharges after the wiping, lasting for around 10 seconds, which were then followed by 4-Hz high-voltage slow waves, predominantly appearing in the bilateral frontal areas for around 10 seconds (video sequences). Suppression of respiration was associated during the seizure (video sequence 2). Seizures did not improve with valproate (dose up to 30 mg/kg) or clonazepam (dose up to 0.08 mg/kg) added with levetiracetam (dose up to 60 mg/kg), but they were unprovoked and disappeared using a combination of valproate (30 mg/kg) and lamotrigine (1 mg/kg).
Discussion
In this study, we have identified a patient with stereotypic ictal events provoked by wiping the face, comprising an abrupt fall, immediately followed by staring upwards, with unresponsiveness lasting for 10 seconds, and 3-Hz generalized spike-wave complex discharges on EEG. The clinical features in this patient were not those of typical absence seizures, as in childhood absence epilepsy, for several reasons. Interictal 3-Hz generalized spike-wave complex discharges were not recorded during wakeful states, but appeared exclusively during sleep. The seizures were not elicited by hyperventilation, but provoked by the somatosensory stimulation on the face. Diminution of muscle tone may be ictal manifestation associated with typical absence seizure, but initial abrupt falling in this patient was rarely an associated feature. It is speculated that the seizures originated from the frontal lobe because there were persistent 4-Hz high-voltage slow wave activities in the bilateral frontal areas following the end of the generalized spike-and-slow-wave discharges (frontal absences).
Somatosensory reflex epilepsy triggered by rubbing a circumscribed area of the body has been reported as “rub epilepsy”, which is regarded as partial epilepsy presenting sensory Jacksonian march, leading to subsequent unilateral tonic contractions with intact consciousness (Kanemoto et al., 2001). Although seizures in our patient were triggered by “rubbing”, ictal manifestations and EEG features were totally different from “rub epilepsy”, as reported.
Generalized seizures with staring provoked by somatosensory stimuli have been very rarely reported. One report in the literature showed absence seizures triggered by tapping the forehead or parietal regions with an appearance of a short burst of diffuse high-voltage spike-wave discharges (DeMarco, 1990). Other studies report absence seizures triggered by walking several steps (Lin et al., 2011), complex visual stimuli such as reading or watching television (Matricardi et al., 1991), and more complex stimuli of recalling an emotion of a traumatic episode in the past (Bencze et al., 1988).
The mechanism of generalized reflex seizures provoked by somatosensory stimulation is unknown. It is proposed that the seizures are propagated by forming a self-propagating oscillatory loop between corticothalamic pyramidal neurons and thalamic relay neurons, due to the hyperpolarizing rhythmic and synchronizing drive provided by burst-firing thalamic relay neurons (Seidenbecher and Pape, 2001; Gorji et al., 2011). In this context, it is speculated that the reflex seizures in this patient may be explained by direct or indirect activation of thalamic relay neurons from abnormally activated signals from somatosensory cortex, topographically corresponding to the face. More detailed evaluations are needed to elucidate the precise mechanisms. Functional neuroimaging techniques, including functional MRI and PET, combined with EEG, may be helpful to understand the mechanism (Gotman and Pittau, 2011).
Supplementary data
Summary didactic slides and supplementary figures are available on the www.epilepticdisorders.com website.
Acknowledgements and disclosures
Drs. Suzuki, Sassa, and Abe have no conflict of interest to report. Dr. Yamanouchi has received funding for teaching purposes from Otsuka Pharmaceutical, USB Pharma Japan, GlaxoSmithKine (GSK), and Novartis.
None of the authors have any conflict of interest to disclose.
* This report was partially presented at the 47th annual meeting of the Japan Epilepsy Society held in October, 2013.