Epileptic Disorders
MENUDisconnective surgery in posterior quadrantic epilepsy: a series of 12 paediatric patients Volume 16, issue 3, September 2014
Multilobar involvement is not unusual in paediatric epilepsy patients. Multilobar pathologies comprise 12-22% of large epilepsy surgery series in children and 3-9% of mixed paediatric/adult series (Sarkis et al., 2012). Head trauma, type II focal cortical dysplasia (FCD), and perinatal insults are among the most common aetiologies of multilobar epilepsy (Sarkis et al., 2012). Children with intractable epilepsy due to extensive lesions involving the posterior quadrant (temporal, parietal, and occipital lobes) form a significant subset of the multilobar epilepsy population. Most reports on the seizure and developmental outcomes were encouraging after temporo-parieto-occipital (TPO) resection or disconnection (Chugani et al., 1993; Leiphart et al., 2001; Fogarasi et al., 2003; D’Agostino et al., 2004; Daniel et al., 2007; Guan et al., 2013).
Resection or functional disconnection of the TPO lobes to treat intractable epilepsy has been reported, however, these surgical procedures constitute less than 5% of epilepsy surgeries in children (Harvey et al., 2008). Multilobar resection can be considered in medically refractory patients after presurgical evaluation in selected cases (Villemure and Daniel, 2006). Large portions of the hemisphere are removed which leaves a large cavity (Daniel et al., 2007). Posterior resection has resulted in a good percentage of patients being seizure-free, although when the occipital lobe is involved persistent visual abnormalities have been reported postoperatively (Sinclair et al., 2005; Battaglia et al., 2012). On the other hand, cognitive development has surprisingly been relatively little affected in children with occipito-parietal lesions who have undergone resection (Battaglia et al., 2012).
The surgical approach for TPO epilepsies has evolved progressively toward more disconnection and less resection (Villemure and Peacock, 1997; Villemure and Daniel, 2006; Daniel et al., 2007; Delalande et al., 2007; Schramm et al., 2012; Dorfer et al., 2013). Disconnective procedures are based on the concept that interrupting the epileptiform discharge/spreading pathway and isolating the primary epileptogenic zone would have the same effect as removing the epileptiform focus. The potential benefits of this approach include smaller craniotomies, reduced blood loss, and fewer long-term complications, such as hemosiderosis and disturbances of cerebrospinal fluid circulation (De Ribaupierre and Delalande, 2008). However, disconnective surgery theoretically would include the risk of leaving epileptogenic cortex “undisconnected” due to intraoperative orientation problems. This difficulty has been suggested as a possible reason for unfavourable seizure outcome reported in some hemispherotomy series, especially in patients with malformation of cortical development (Devlin et al., 2003). The number of patients with intractable epilepsy of the posterior lobes who have undergone disconnective surgery is relatively small but results have shown that the procedure is effective for preventing seizures with a range from 56 to 91% of patients becoming seizure-free (Mohamed et al., 2011; Thomas et al., 2012). It should be emphasized that disconnective surgery is not palliative surgery, which is possible only by cutting the corpus callosum, but is equivalent to resective surgery to prevent seizures.
The primary aim of this study was to report our experience of TPO or PO disconnection surgery to treat children with intractable posterior quadrantic epilepsy with anatomical lesions, observed on MRI and functional abnormalities revealed by 2-deoxy-2[F-18]fluoro-D-glucose positron emission tomography (FDG-PET) imaging, who underwent such surgery, and assess surgical outcomes. A secondary aim was to assess cognitive outcomes and neurological deficits after TPO or PO disconnection surgery.
Patients and methods
All patients who underwent TPO disconnection surgery at Fuzhou General Hospital Epilepsy Center between September 2009 and September 2012 were reviewed retrospectively. The study was approved by the Clinical Research Ethics Board of Fuzhou General Hospital. TPO surgery was offered if patients had seizures that were refractory to medication. Prior to surgery, 2 antiepileptic drugs (AEDs) had been tried in 5 patients, 3 AEDs in 4 patients, and 4 AEDs in 3 patients. The indications for TPO deconnection surgery included: 1) focal seizures with unilateral TPO onset or generalised seizures with asymmetric clinical or EEG features suggesting a focal basis in the TPO region on one side; 2) an ipsilateral posterior quadrant lesion on MRI or functional imaging abnormality in the ipsilateral TPO region; and 3) an unsuccessful pharmacological therapeutic protocol and requirement of surgery, without being a candidate for hemispherectomy, i.e. without a hemispheric lesion or progressive hemispheric disorder.
The contraindications to TPO disconnection surgery included: 1)preoperative investigations aimed at localising the epileptogenic zone that were discordant between imaging, EEG, and clinical evaluations, and chronic invasive recording was needed; 2) presence of risk factors for multifocal epilepsy, including cerebral anoxia, central nervous system infection, or bilateral multifocal tuberous sclerosis; 3) normal or non-localised MRI or FDG-PET findings; 4) more generalised seizure patterns on EEG than posterior quadrant unilaterally; 5) symptomatic epilepsy caused by a vascular lesion, such as an arteriovenous malformation or tumour requiring resection for treatment of the substrate; 6) a pathological substrate responsible for the seizure disorder that was progressive, such as Rasmussen's encephalitis, which may later necessitate hemispherectomy; or 7) a visual field defect caused by a contralateral hemisphere pathological substrate. Also, one patient who had previously undergone a frontal lobe topectomy at another centre was excluded from this study.
Presurgical evaluation
All patients in this study underwent a comprehensive evaluation including detailed history and neurological examination, long-term video-electroencephalogram (VEEG) monitoring, and MRI (3.0T). More than three episodes of natural attacks were recorded. Also, interictal FDG-PET was performed in all patients to evaluate the functional status of the fronto-central lobe and the contralateral hemisphere, and to define more precisely the extent of dysplasia and/or to detect dysplastic cortex in the contralateral hemisphere. If necessary, invasive recordings, i.e. long-term extra-operative recording to detect the expression of epileptiform foci located in the TPO region, and stimulation of functionally indispensable (“eloquent”) cortical areas, which included areas involved in language, motor, and sensory functions, were also performed.
Preoperative and postoperative neuropsychological test results were assessed by a psychologist. Patients over the age of 14 years were administered the Wechsler Adult Intelligence Scale (Chinese version), 6-13-year-old patients were administered the Wechsler Child Intelligence Scale (Chinese version), and 4-6-year-old patients were administered the Wechsler Preschool and Primary Scales of Intelligence (Chinese version). According to the preoperative full-scale intelligence quotient (FIQ), patients were divided into four groups: severe intellectual disability (IQ≤34), moderate intellectual disability (IQ 35-49), mild intellectual disability (IQ 50-70), and no intellectual disability (IQ>70). The preoperative assessment was performed within one month before surgery and the postoperative assessment was performed three months after surgery.
Surgical technique
Surgery comprised either PO disconnection, which was performed in one patient who had a previous ipsilateral temporal lobectomy, or TPO disconnection in patients who had previously not undergone surgery.
TPO disconnection was performed via a periinsular approach, similar to that described by Daniel et al. (2007) with some modifications, as follows:
- (1)In order to reduce trauma and blood loss, the incision was reduced in size. The incision was an elongated “barn-door” incision with the anterior and posterior limbs ending at 3 cm over the zygoma and 2 cm over the anterior third of the transverse sinus, respectively. The medial part of the incision extended to about 2 cm from the midline.
- (2)An elongated bone flap was cut, exposing the post-central region from 2.5 cm to the midline, down to the posterior temporal operculum.
- (3)Prior to dissection, the post-central sulcus was identified by correlating gyral and venous landmarks from the exposed cortex with three-dimensional surface reconstructions of the patient's MRI scans (Naidich et al., 1995; Yousry et al., 1995; Boling et al., 1999). After confirming the central sulcus by median nerve somatosensory evoked potential (SEP) phase reversal recorded through a subdural grid electrode, an 8-contact subdural strip electrode was positioned on the long axis of the post-central gyrus. Thereby, continuous SEP monitoring during the disconnection procedure was provided.
- (4)Disconnections were started with a corticotomy and subpial suction/resection at the parietal operculum reaching the ventricular trigone. In patients with small ventricles, we further removed the temporal operculum to find the temporal horn.
- (5)During the resection of the parietal and temporal cortex and the white matter on the line of the disconnection, care should be taken to preserve as many of the arteries and veins as possible; the sulci should be passed over and the arteries and veins inside the sulci should be completely preserved. The gyri between sulci were cut open segmentally to form successive windows, but these windows were not connected by a line.
- (6)When looking for the lateral ventricles and establishing a rational approach, a navigation system is a very useful auxiliary tool (Dorfer et al., 2013), however, navigation was used only for the last patient in our series because our epilepsy centre had been only recently equipped with a navigation system.
Resection or biopsy specimens from at least one area, most commonly the superior temporal gyrus or angular gyrus, were available for review in all patients. Large crossing veins, arteries, and bridging veins were spared throughout the procedure.
Postoperative follow-up
Patients were assessed after surgery at 3 months, 6 months, and 1 year, and then annually. Postoperative examinations included thorough neurological, neuropsychological, and neuro-ophthalmological evaluations, as well as 48-hour video-EEG monitoring. MRI was performed at 3 months and 12 months after surgery. Seizure outcome was based on the Engel classification system according to patient and family reporting.
Withdrawal of antiepileptic drugs was recommended two years after surgery, provided that the patient was completely seizure-free and EEG control examinations did not show epileptiform activity.
Statistical analysis
Categorical data were presented as counts and percentages. Continuous data were presented as medians and ranges. The comparisons of pre- and postoperative intelligence quotient (IQ) were performed by Wilcoxon signed rank test. Statistical analyses were carried out using SPSS software version 17 (SPSS Inc, Chicago, IL, USA). A two-tailed p of <0.05 was considered statistically significant.
Results
The patients’ demographic and clinical characteristics are presented in table 1. Their median age at onset was 4 years (range: 0.25-11). The mean preoperative seizure frequency was 15 seizures per month (range: 6-120). All patients had developmental delay, 5 (41.7%) had mild delay, 3 (25.0%) had moderate delay, and 4 (33.3%) had severe delay. The presenting seizure types were epileptiform spasms in 8 children, focal seizures in 3, and tonic-clonic seizures in 1 child. Ten children subsequently developed other seizure types including atonic (n=3), tonic (n=2), tonic-clonic (n=5), and atypical absence (n=1) seizures. At the time of surgery, 3 children had atonic seizures, 4 had symptomatic epilepsy with focal seizures and alteration of consciousness, and 4 had secondarily generalised seizures; one child also had spasms and tonic seizures (Case 12). Median age at the time of epilepsy surgery was 12.3 years (range: 4-18). All 12 children, 6 girls, and 6 boys underwent posterior quadratic disconnective surgery. Seven children underwent left TPO surgery, a PO disconnection was performed (combined with a previous temporal lobectomy) in one patient, and 4 underwent right TPO surgery.
After disconnection surgery, the background slowing increased in the related brain regions. Though there were still some epileptiform discharges, the extent was reduced after surgery and the discharges did not spread to other brain regions. The median postoperative IQ was significantly higher than the median preoperative IQ (58 vs. 47; p=0.04) (table 1). One patient (Patient 12) had remarkable developmental acceleration with an increase in IQ from 37 preoperatively to 60 postoperatively.
The seizure outcome was determined by Engel classification; there were nine (75.0%) patients in class I, two (16.7%) in class II, and one (8.3%) in class III. Two patients exhibited severe brain swelling five days after the surgery. This swelling was attributed to inappropriate management of blood vessels during the early stage of our experience with this surgical procedure. One of these two patients underwent a second resective operation and had a good recovery. The other patient developed new motor deficits, as hemiparesis worsened slightly postoperatively. In the later stage of our experience, all of the large crossing veins, arteries, and bridging veins were spared throughout the procedure, and therefore no severe brain oedema occurred.
With regard to EEG findings, 12 patients had EEG abnormalities over the posterior quadrant or within the involved hemisphere, but with marked posterior predominance. The interictal EEG mainly demonstrated asymmetric background abnormal activity (slowing) and repetitive paroxysmal activity of high-amplitude spikes, polyspikes, and spike-wave complex on the affected hemisphere, with predominance on the posterior and temporal regions. In 3 patients, independent contralateral abnormalities were detected. Prolonged video-EEG recordings clearly demonstrated the origin of the epileptiform activity arising from a large radiological abnormality in all patients with propagation of activity to the anterior cortices or contralaterally in ictal recordings. In all but 1 patient, who underwent TPO resection in a second operation, postoperative EEG showed localised epileptiform waves in the disconnected posterior regions of the affected side, without contralateral and anterior spreading.
There were 2 patients who had a visual deficit before surgery. One of these 2 patients had undergone right ATL surgery in another hospital and there were homonymous defects in the upper quadrants of both eyes and contralateral limb hemiparesis before surgery. With respect to postoperative neurological deficits, this patient had brain swelling on the fifth postoperative day and hemiparesis was aggravated on the left side. For the other 11 patients, no significant motor dysfunction was observed. All 12 children had contralateral hemianopia postoperatively.
Example case
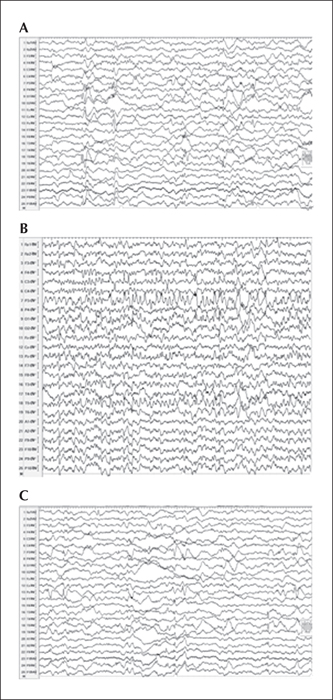
An example case is Patient 12, a 5-year-old boy born at term after an uneventful pregnancy, who, three months after birth, began to have tonic seizures and epileptiform spasms with asymmetric tonic posture, and eye blinking and deviation to the right side. He had 2-14 seizures per week. The seizures were intractable to multiple antiepileptic drugs. On admission, he was given valproate at 750 mg/day and lamotrigine at 100 mg/day. His development was significantly delayed with an IQ of 37. Interictal EEG revealed asymmetric background abnormal activity (slowing) and lateralised epileptiform discharges (spike-wave activities) on the left TPO area (P3, T5, O1, P9, Pz) (figure 1A). Ictal EEG was characterised by unilateral epileptiform discharges with an alpha-theta recruiting rhythm over the left posterior quadrant area (P3, T5, O1) (figure 1B).
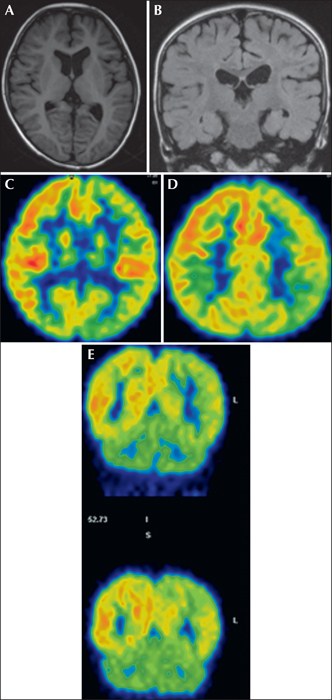
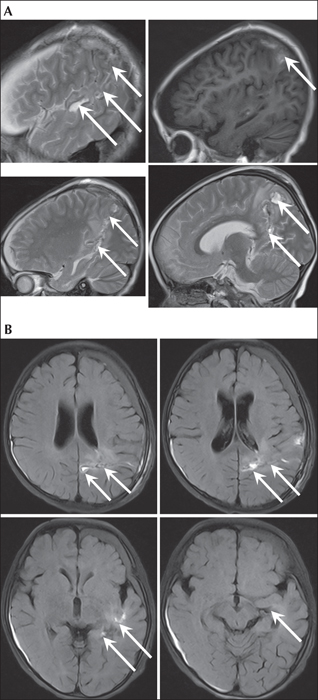
MRI revealed mild atrophy in both cerebral hemispheres and it was more significant in the left hemisphere (figure 2A and 2B). An FDG-PET study revealed obvious hypometabolism in the left temporal, parietal, occipital, and frontal regions (figure 2C-2E). These radiological findings suggested TPO cortical dysplasia. The aim of surgery was to eliminate the influence of the large dysplastic epileptogenic zone comprising the temporal, parietal, and occipital lobes. The patient underwent a left TPO disconnection with no postoperative complications (figure 3A and 3B). Postoperative EEG showed epileptiform activity confined to the disconnected region (figure 1C). The patient became seizure-free after surgery, and he showed remarkable developmental acceleration (23-point increase in IQ scores), with development of language and learning abilities. Histological examination of the angular gyrus revealed FCD IIb.
Discussion
In this study, we reviewed the surgical outcomes of 12 paediatric patients with posterior quadrantic epilepsy who underwent TPO or PO disconnective surgery to prevent seizures and found that at a median follow-up duration of 34 months, 9 patients had seizure-free outcomes (Engel class I). Of the 3 remaining patients, 2 were classified as Engel class II and 1 as Engel class III. These 3 patients did not become seizure-free because it turned out that the extension of the dysplastic and epileptogenic area was beyond the range of TPO surgery and therefore that surgical approach was unable to solve the problem. Two patients had the complication of brain swelling and one of these patients underwent a second operation. Our results showed that TPO and PO disconnection surgical procedures are safe and effective for treating children with posterior quadrantic epilepsy.
The importance of functional cortical mapping in TPO surgery has previously been pointed out (Daniel et al., 2007). We performed continuous cortical somatosensory and/or motor evoked potential monitoring to optimise the planned disconnection and increase the safety of the procedure. This maximizes the extent of disconnection and safety of surgery. Functional disconnection of the temporal, parietal, and occipital lobes evolved from functional hemispherotomy, in which there is minimal removal of brain tissue and preservation of the arterial and venous supply to the disconnected cortex. In one patient, we had to further remove the temporal operculum, parietal cortex, and underlying white matter along the line of the disconnection to obtain adequate vision of the ventricle. The presence of a previous temporal lobectomy did not preclude parietal disconnection, being equivalent to the functional posterior quadrantectomy of Daniel et al. (2007), although more often incomplete.
So far, only a few studies have focused on posterior quadrantic epilepsy surgery, and published data on seizure outcome of posterior quadrantic epilepsy surgery are difficult to interpret because there are only a relevant few studies (Leiphart et al., 2001; Fogarasi et al., 2003; D’Agostino et al., 2004; Dalmagro et al., 2005; Sinclair et al., 2005; Daniel et al., 2007; Mohamed et al., 2011; Sarkis et al., 2012; Dorfer et al., 2013; Guan et al., 2013). Seizure outcome in these series differed significantly, with seizure freedom ranging from 50 to 92%. This wide range of outcome is probably due to differences in patient selection and surgical techniques. If presurgical evaluation shows congruent data based on MRI, PET, interictal/ictal scalp EEG, and clinical neurological and neuropsychological examinations indicating seizure onset in one posterior quadrant, favourable seizure outcome can be expected (D’Agostino et al., 2004; Daniel et al., 2007). Posterior quadrant dysplasia has been described as a characteristic brain malformation (D’Agostino et al., 2004). Surgical treatment of these posterior quadrantic epilepsies with involvement of the TPO area has also been performed in other medically refractory epilepsy syndromes (Daniel et al., 2007; Mohamed et al., 2011). A recently published study reported by Mohamed et al. (2011) also included children with normal or non-localising MRI findings and more generalised seizure patterns on EEG. Six of the 16 children had generalised infantile spasms (hypsarrhythmia) on scalp EEG and four children had typical EEG patterns observed in Lennox-Gastaut syndrome. Seizure outcome after TPO surgery was Engel class I in only 56% of the patients.
In our study of TPO disconnective surgery, only 2 (16.7%) patients had the complication of brain swelling. One of the patients required a second operation. Daniel and Villemure (2003) noted that, compared to resective surgery, the rate of hydrocephalus is reduced by disconnective surgery. Also, there are no reports of long-term complications, e.g. superficial cerebral hemosiderosis (Daniel et al., 2007). Binder and Schramm (2008) pointed out that even with modern hemispherectomy approaches, a considerable number of patients still have hydrocephalus that requires shunting. Villemure et al. (2000) reported a rate of hydrocephalus requiring shunting of almost 19% (10/53) using the Delalande technique for hemispherectomy and a rate of about 8% (5/63) using Villemure's perisylvian window technique. Shimizu and Maehara (2000) performed hemispherectomy using their technique and found that five of 32 (15.6%) patients had hydrocephalus necessitating shunting. Hemispherectomy performed with Schramm's transsylvian keyhole technique was found to result in hydrocephalus, requiring shunting in 4% (2/49) of patients (Binder and Schramm, 2006; Schramm et al., 2001).
All of the children in this study had developmental delay at the time of surgery. During follow-up, 8 of 12 children had higher IQ scores after surgery (table 2), and the improvement in IQ scores reached statistical significance. Also, there were observable developmental improvements. Our findings support those of several other studies of children who underwent epilepsy surgery. Freitag and Tuxhorn (2005) found that 42 (82%) of 50 children had stable velocity of development after surgery. Lippé et al. (2010), who reported on a study that included only 5 children, stated that their results suggested that brain plasticity permits young children to have cognitive skills for schooling after surgery. Ramantani et al. (2013) found that developmental outcome was better in children with acquired aetiology and older age at the time of surgery. In another study, Ramantani et al. (2014) observed that on a group level there was no deterioration in any cognitive variable after surgery. Mohamed et al. (2011) reported that, according to all the parents and caregivers, behaviour, temperament, and overall functioning improved and there were some reports of acquisition in new development skills, however, the authors noted that in some instances, these observations were not always supported by objective assessments.
We were not able to clearly identify which type of seizure-free patients had more improvement of development postoperatively and which had less. However, we speculate that less development is a greater likelihood in seizure-free children with FCD type Ib histopathology and seizure-free children with independent contralateral abnormalities. In our study, 3 children had FCD type Ib histopathology and 3 children had independent contralateral abnormalities.
This study was limited because it was retrospective in design. Another limitation was the small sample size of 12 patients. Because small sample size was also a characteristic of all previous such studies, a meta-analysis might be useful for drawing firmer conclusions about the safety and effectiveness of TPO and PO disconnective surgery. An additional limitation was the lack of a comparison group. A prospective study comparing resective surgery with disconnective surgery for patients with posterior quadrantic epilepsy would provide a better comparison between these two types of surgical procedures, however, because of the advantages of disconnective surgery with regard to perioperative and long-term complications, such a comparative study is probably not feasible.
To summarise, we found that, for children with epileptiform foci located in the TPO region in one hemisphere, the surgical outcome was excellent and the complications were less than for those with routine en bloc TPO resection. Our surgical procedure was improved in that it was simplified, a small incision was used, and the surgical trauma was minimal. Not only did we clearly confirm the importance of preserving arteries and veins on the brain surface, which has been previously demonstrated, but we also confirmed the importance of preserving arteries and veins in the brain sulci during surgery. Also, the transection was performed on a line connecting several windows, which was different from previous reports that used the trench-shaped transection method. TPO and parieto-occipital disconnection are safe and effective motor-sparing epilepsy surgical procedures in selected patients with the epileptiform zone localised to the posterior quadrant on one side. Technical adjuncts, including three-dimensional surface reconstructions of the patient's MRI (Mert et al., 2012; Ribas, 2010), and intraoperative electrophysiological monitoring, facilitate better visualisation and orientation, enabling a less invasive approach. This type of surgery does not add further deficit in children who have pre-existing hemianopia. It is also a pragmatic approach for intractable epilepsy in a child with regionalised, but imprecisely localised, posterior quadrant seizures based on EEG and functional imaging, or in a child with a poorly defined posterior cortex lesion, particularly in young children with developmental delay and low risk of language and learning deficit. In this specific context, TPO disconnection increases the likelihood of isolating the epileptogenic region. For cases in which the range of lesion or the epileptogenic area exceeds the TPO range, only intracranial EEG monitoring can exactly identify the surgical range and procedure, and obtain a better seizure outcome.
Disclosures
None of the authors have any conflict of interest to disclose.