Journal de Pharmacie Clinique
MENUMedication reconciliation in a short-stay geriatric service: overview after one year Volume 39, issue 2, Juin 2020
- Key words: medication reconciliation, medication errors, geriatrics
- DOI : 10.1684/jpc.2020.0430
- Page(s) : 102-12
- Published in: 2020
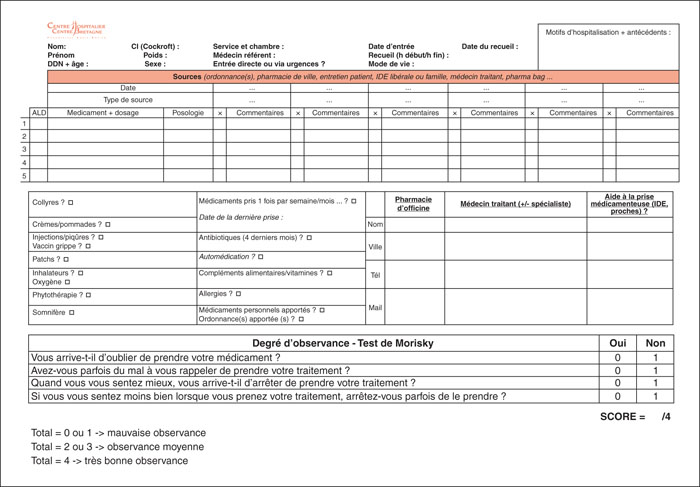
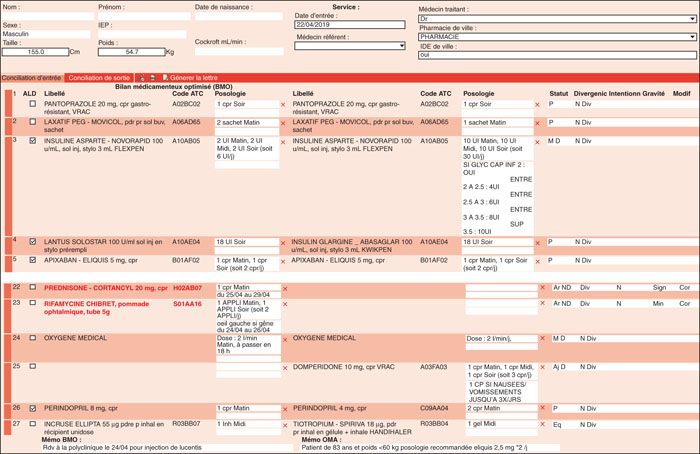
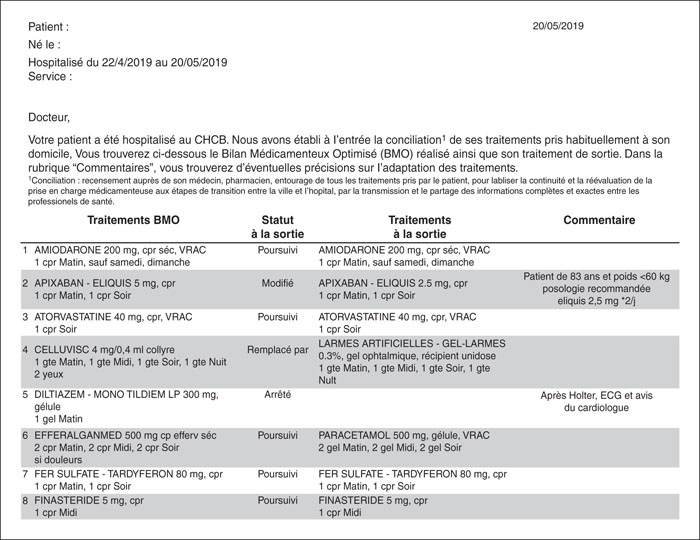
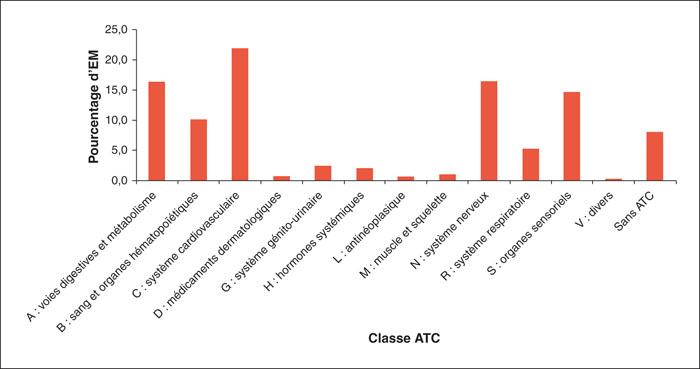
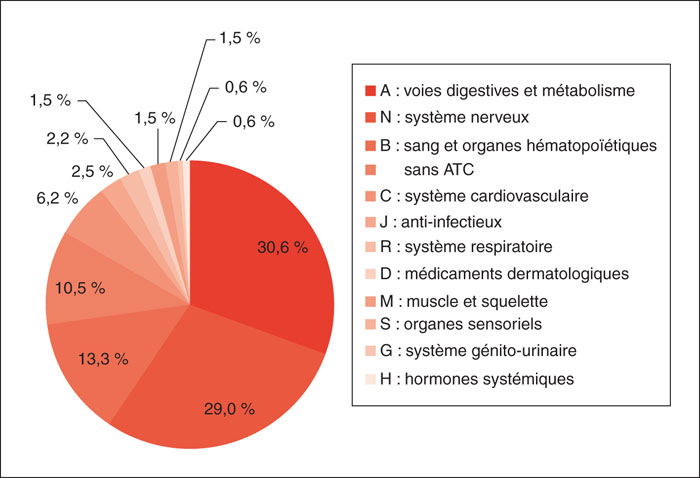
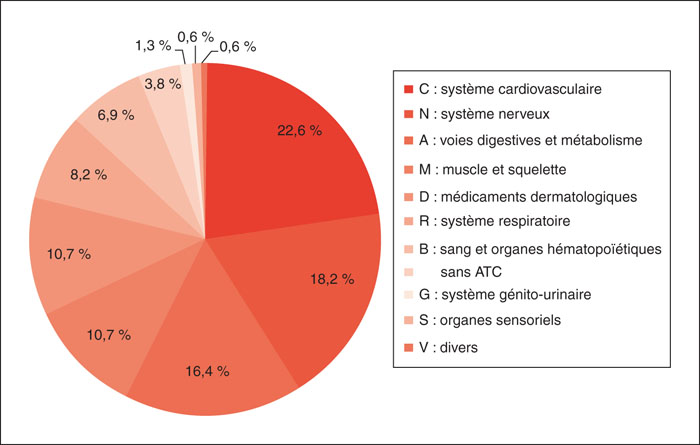
The aim of the medication reconciliation (MR) is to secure the patient's medicine management during his/her care journey. Since November 2017, MR for the admissions and discharges has been deployed in a geriatric service. A study was carried out over 1 year to establish an overview of the situation and identify areas for improvement in our organization; 213 patients living at home, of average age 85.7 years, received an MR at their admission (36.6% of patients defined as reconcilable); 287 medication errors were detected, i.e. 1.3 medication errors per patient. Pharmacists and doctors rated the severity of medication errors and qualified 3.8% of medication errors as major, 29.3% as significant and 66.9% as minor. Medication errors mainly concerned 3 pharmacological classes. Medication errors of cardiovascular class appear to be at higher risk (58.7% at least significant) than digestive tract class and metabolism (minor at 82.9%) or the nervous system class (minor at 53.2%). Of these 213 patients, 113 received MR at their discharge (63.5% of patients defined as reconcilable). At the end of hospitalization the number of drugs was higher than at the beginning (11.2 lines versus 9.8 lines). Improving the admission MR requires additional resources to increase the performance of our quantitative indicators; the improvement of the discharge MR will be at the qualitative rather than quantitative level with the implementation of the revision of the relevance of treatments during hospitalization.
![]() This work is licensed under a
Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License
This work is licensed under a
Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License