Hépato-Gastro & Oncologie Digestive
MENUSplanchnic venous thrombosis and acute/chronic pancreatitis Volume 28, issue 2, Février 2021
- Key words: splanchnic venous thrombosis, acute and chronic pancreatitis, anticoagulation, segmental portal hypertension, gastrointestinal bleeding
- DOI : 10.1684/hpg.2021.2121
- Page(s) : 201-11
- Published in: 2021
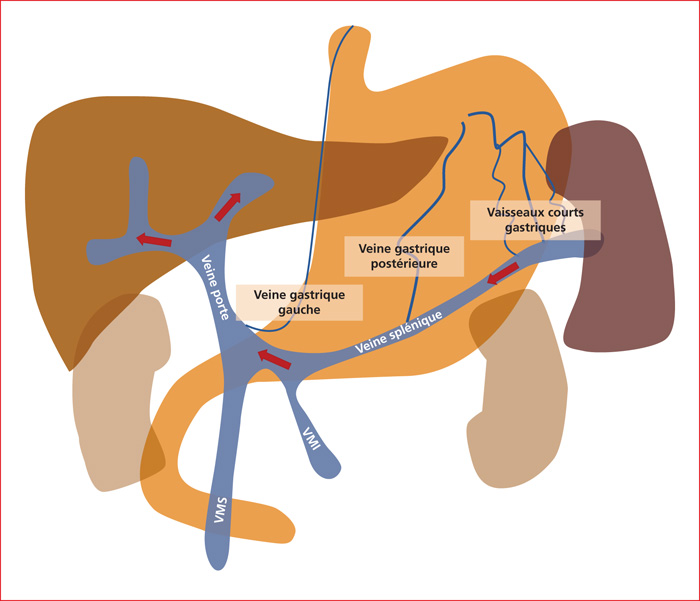
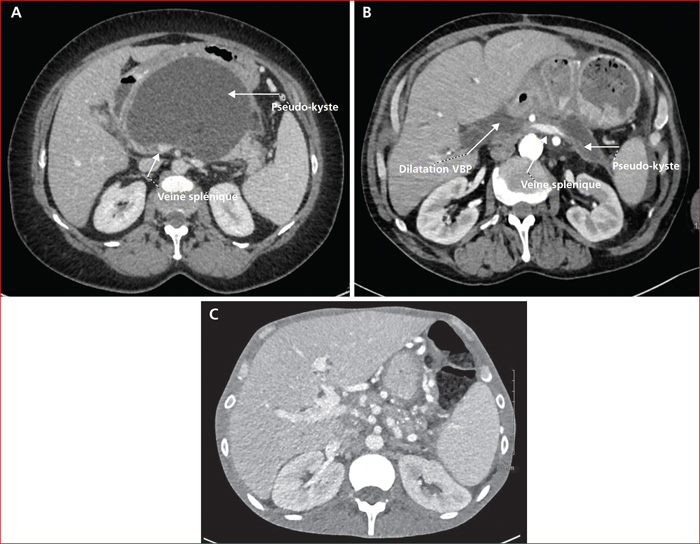
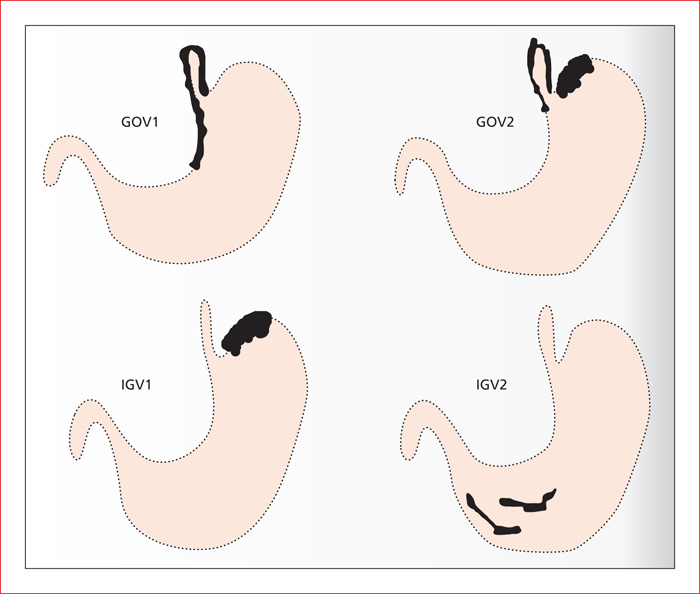
Splanchnic vein thrombosis is one of vascular complication of acute and chronic pancreatitis. The incidence varies among studies and ranges from 1.8 to 35%. Due to the localization, splenic vein thrombosis is the most common. Patients are asymptomatic more than 90% of cases. Doppler ultrasonography is an excellent first-line examination, to be confirmed by axial CT or MR imaging using vascular contrast agents. Local inflammation (necrosis, fluid collections, pseudokysts), due to the close proximity of the vascular network, appears to be the major predisposing condition. Thrombophilia and hypercoagulable state due to the inflammation are not identified as independent risk factors. Consequently, thrombophilia should not be systematically screened. Anticoagulation therapy is indicated for 3 to 6 months in portal vein thrombosis, in mesenteric vein thrombosis and debated in isolated splenic vein thrombosis. Portal hypertension with development of gastric varices is the main complication. In case of gastrointestinal bleeding, which occurs in approximately 12.3%, endoscopic treatment is effective, followed by endoscopic treatment or in beta-blocker monotherapy. Splenectomy or splenic artery embolization are rarely used due to their rate of complications but remain an alternative in cases of uncontrolled bleeding.