Hépato-Gastro & Oncologie Digestive
MENUManagement of bowel dysfunction in patients with Spina Bifida: what is the place of the gastroenterologist? Volume 23, issue 10, Décembre 2016
service des maladies de l’appareil digestif,
Université de Rennes 1,
2 rue Henri le Guillou,
35033 Rennes cedex,
France
service d’explorations fonctionnelles digestives,
Université de Rennes 1,
Rennes,
France
- Key words: Spina Bifida, multihandicapped, constipation, fecal incontinence
- DOI : 10.1684/hpg.2016.1383
- Page(s) : 946-53
- Published in: 2016
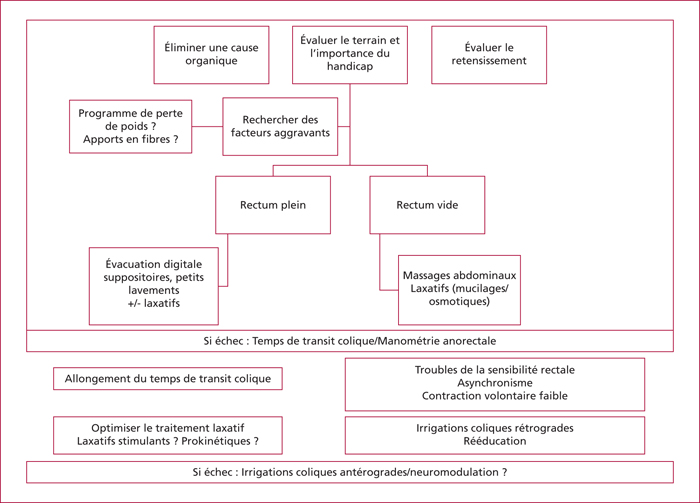
Spina bifida is a rare birth defect due to incomplete closure of the neural tube. Spina Bifida is associated with multiple functional impairments: patients with Spina Bifida are multihandicapped and require a multidisciplinary approach. Bowel dysfunction such as constipation and fecal incontinence is the second most common major concern in patients with Spina Bifida behind lower urinary tract dysfunction. In contrast to the well-established care of urological disorders, bowel dysfunction lacks evidence to assist in physician decision-making. Neurological level is not associated with bowel dysfunction highlighting the importance of the initial evaluation. In case of failure of the first line treatment, anorectal manometry and colonic transit time can be useful. The management of bowel dysfunction is based on abdominal massages, softeners, anal digitation to defecate, biofeedback and retrograde/anterograde enemas.