Hépato-Gastro & Oncologie Digestive
MENUDiagnosis and treatment of perianal Crohn's disease Volume 23, issue 4, Avril 2016
Hôpital de Hautepierre,
Pôle des pathologies digestives,
hépatiques et de la transplantation,
service d’hépato-gastroentérologie et d’assistance nutritive,
67098 Strasbourg Cedex, France
Hôpital de Hautepierre,
Pôle des pathologies digestives, hépatiques et de la transplantation,
service de chirurgie digestive,
67098 Strasbourg Cedex, France
Faculté de Médecine,
Unité INSERM 1113,
Laboratoire « Voies de signalisation du développement et du stress cellulaire dans les cancers digestifs et urologiques »,
3 avenue Molière, 67200 Strasbourg, France
Faculté de Médecine,
Fédération de Médecine Translationnelle de Strasbourg,
4 rue Kirschleger, 67000 Strasbourg, France
- Key words: Crohn's disease, perianal fistula, Anti-TNF monoclonal antibodies
- DOI : 10.1684/hpg.2016.1284
- Page(s) : 335-44
- Published in: 2016
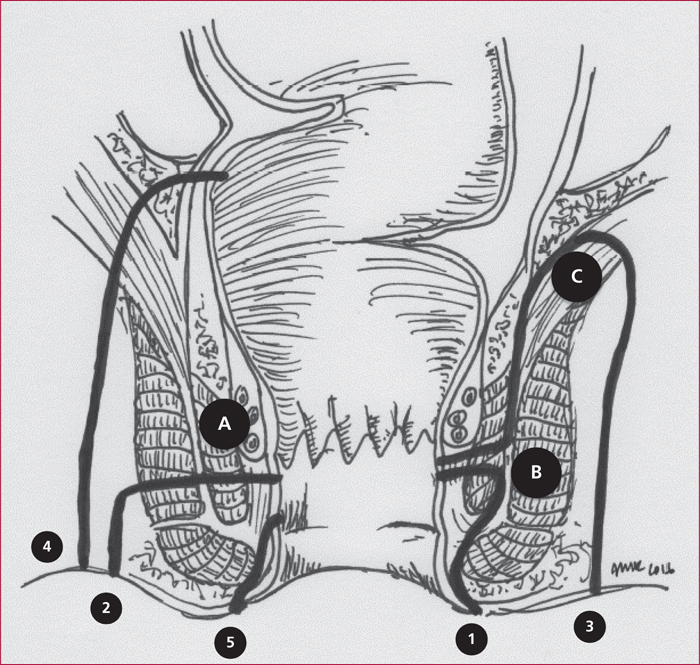
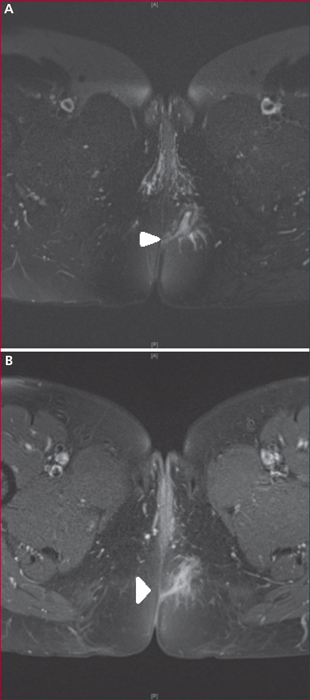
Perianal fistulas occur in up to 20% of Crohn's disease (CD) patients during the course of their disease. They can be particularly debilitating due to symptoms such as purulent discharge, pain, or fecal incontinence. In addition, they expose the affected patients to radical surgery including defunctioning stoma or proctectomy. Unfortunately, the available literature concerning their optimal treatment remains limited and their treatment still constitutes a matter of debate. Accurate diagnosis of the type of perianal lesions is essential as well as a proper appreciation of luminal CD extension and severity. Perianal fistula diagnosis is best achieved by using a combination of pelvic magnetic resonance imaging (and/or endorectal ultrasonography) and physical examination under anesthesia. Their treatment often requires the combination of medical therapy (mostly using anti-TNF monoclonal antibodies) and several surgical procedures needing to be performed with caution in order to avoid irreversible complications. Treatment strategy decision ideally requires a close cooperation between gastroenterologists, digestive surgeons and radiologists. The objective of this review is to present the current knowledge in this particularly challenging phenotype of CD.