Hépato-Gastro & Oncologie Digestive
MENUSupport for anal incontinence in adults in 2016 Volume 23, issue 6, Juin 2016
Figures
-
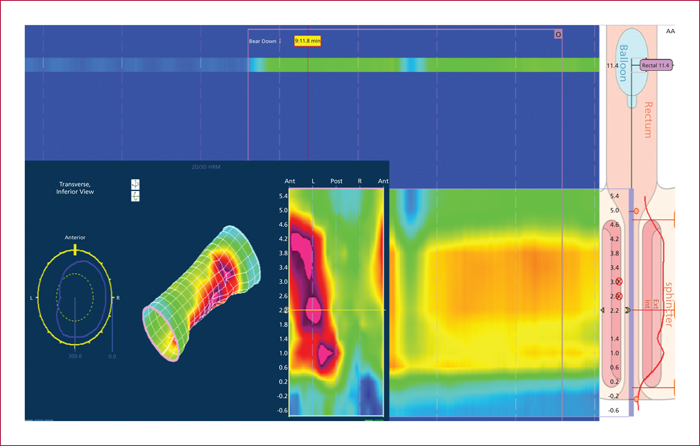
Figure 1 -
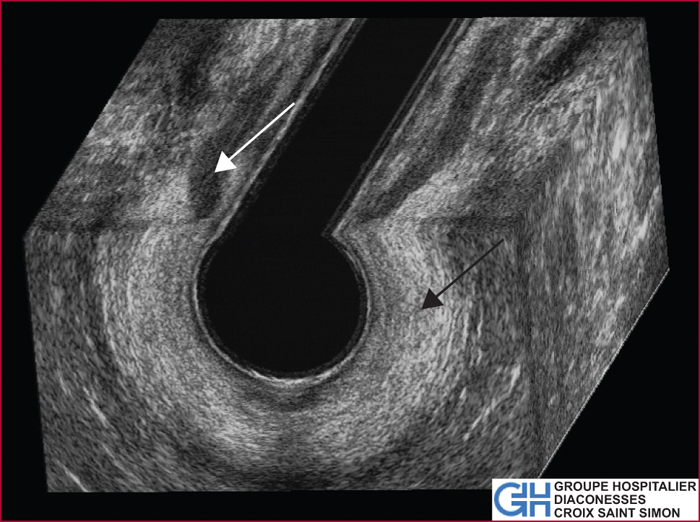
Figure 2 -
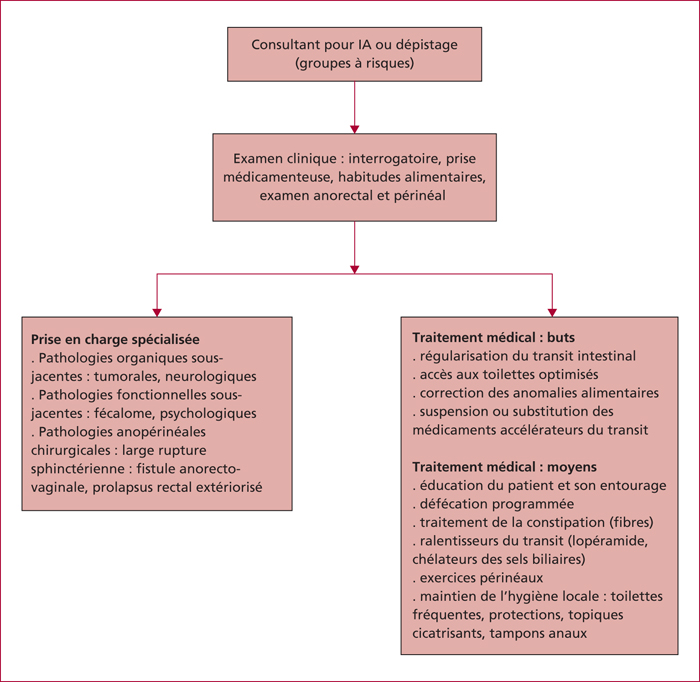
Figure 3 -
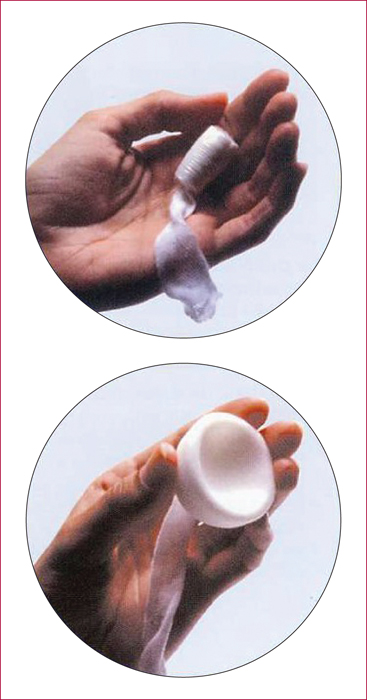
Figure 4 -

Figure 5 -

Figure 6 -
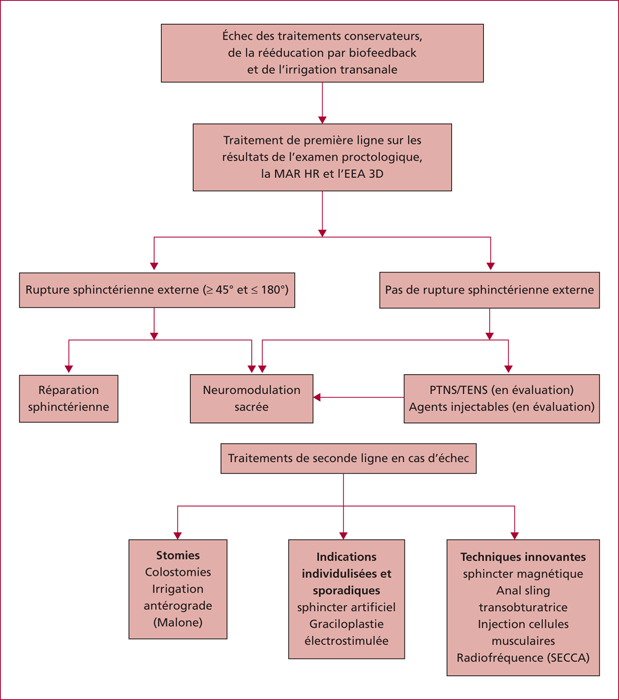
Figure 7 -
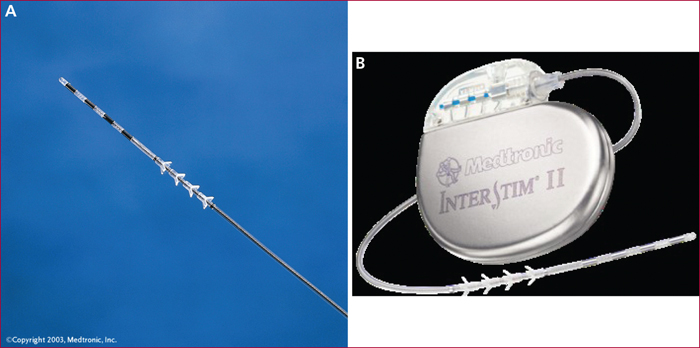
Figure 8 -
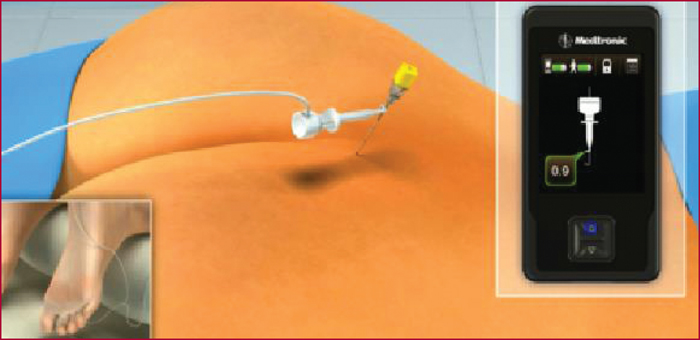
Figure 9 -
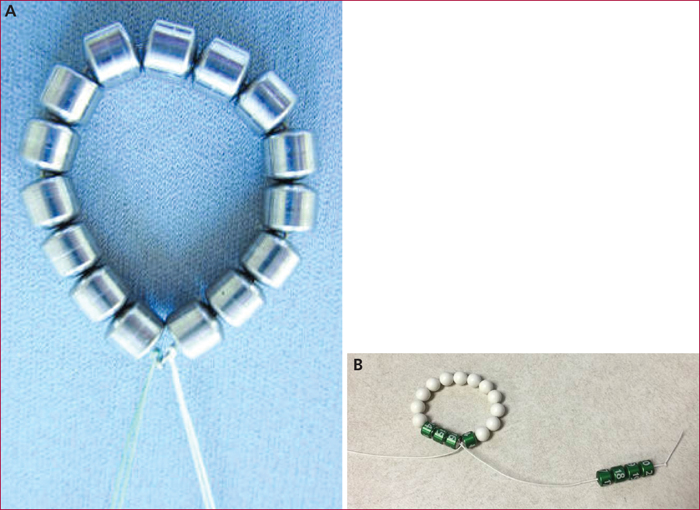
Figure 10 -
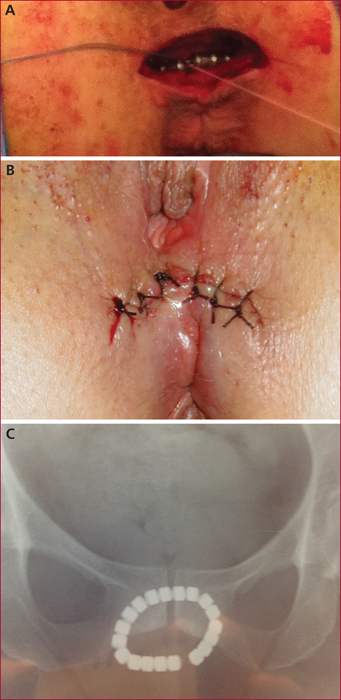
Figure 11 -
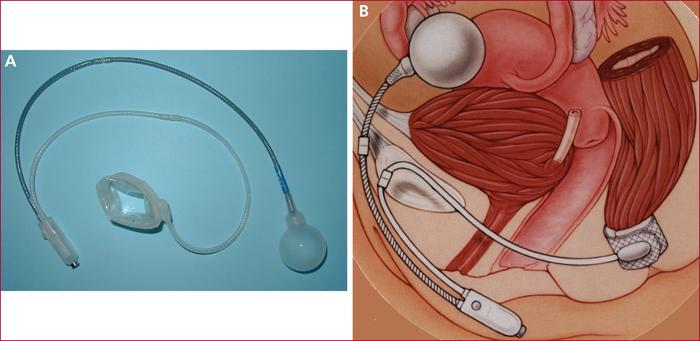
Figure 12 -
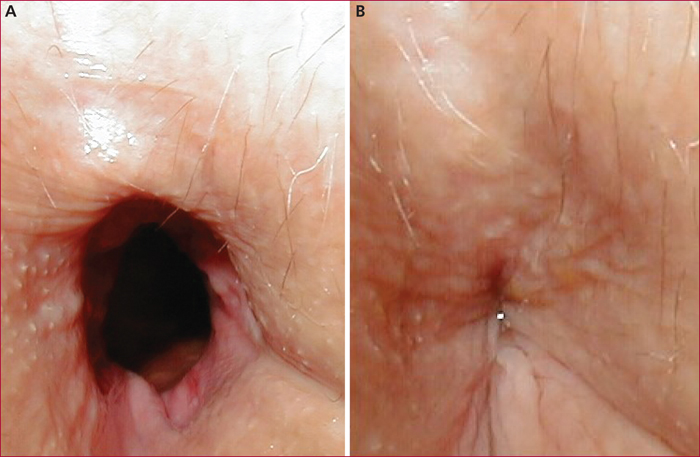
Figure 13
Tables
service de proctologie médico-interventionnelle (Site Avron),
125 rue d’Avron 75020 Paris,
France
- Key words: anal incontinence, anal incontinence, biofeedback, endoanal ultrasonography, magnetic anal sphincter, artificial anal sphincter
- DOI : 10.1684/hpg.2016.1309
- Page(s) : 527-37
- Published in: 2016
Anal incontinence is an underestimated public health problem. There are often multiple causes requiring medical and surgical management. As a rule, a non-surgical approach is proposed as the first line treatment, leading to a beneficial response in about 50% of patients. Rehabilitation, at best using biofeedback techniques, peripheral stimulation, and in certain cases retrograde colonic irrigation can further improve therapeutic response. If medical treatment is unsuccessful, operable patients may benefit from innovative surgical procedures after a careful posterior anoperineal work-up using high-resolution anorectal manometry, 3D endo-anal ultrasound, or magnetic resonance defecography. Indications for these surgical procedures, designed to preserve deficient anorectal anatomic structures, are established at multidisciplinary pelvi-perineology meetings for patients with severe anal incontinence who fail to respond to medical treatment and rehabilitation. Sacral neuromodulation is currently the most widely used technique. The magnetic sphincter is in the evaluation phase while the artificial anus, a highly targeted indication, is being proposed less often despite encouraging results. Preventive measures limiting deleterious maneuvers injuring the anatomic structures guaranteeing anal continence should be a constant concern for interventional proctologists, digestive surgeons, radiotherapists, and obstetricians.

