Hépato-Gastro & Oncologie Digestive
MENUPortopulmonary hypertension in 2016 Volume 23, issue 9, Novembre 2016
service d’hépatologie et de soins intensifs digestifs,
25000 Besançon,
France
service d’hépato-gastroentérologie, de nutrition et d’alcoologie,
60109 Creil Cedex,
France
- Key words: cirrhosis, pulmonary arterial hypertension, portopulmonary hypertension
- DOI : 10.1684/hpg.2016.1361
- Page(s) : 839-49
- Published in: 2016
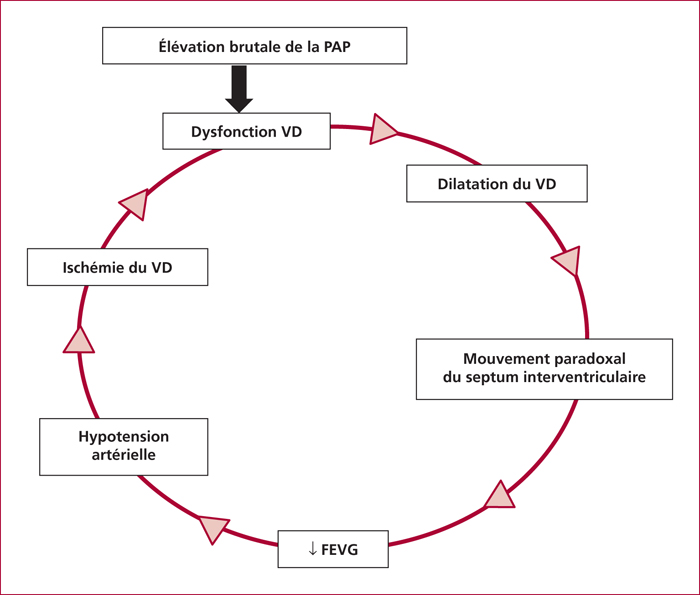
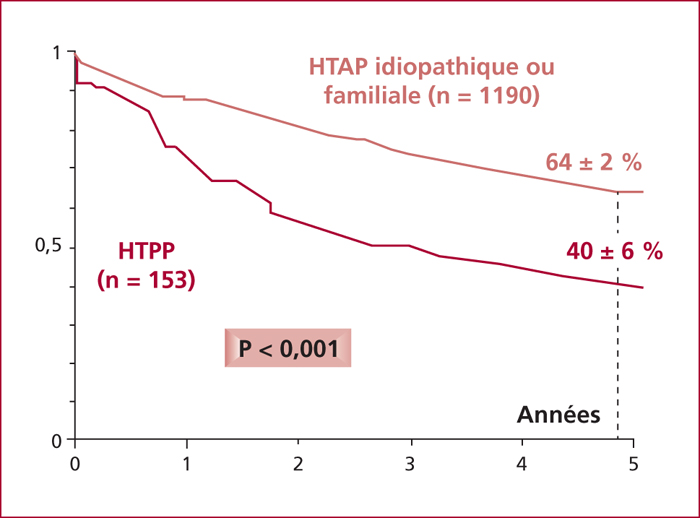
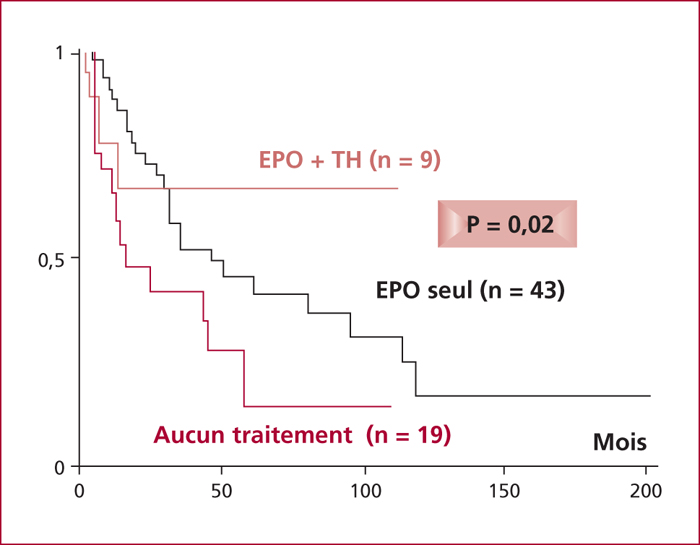
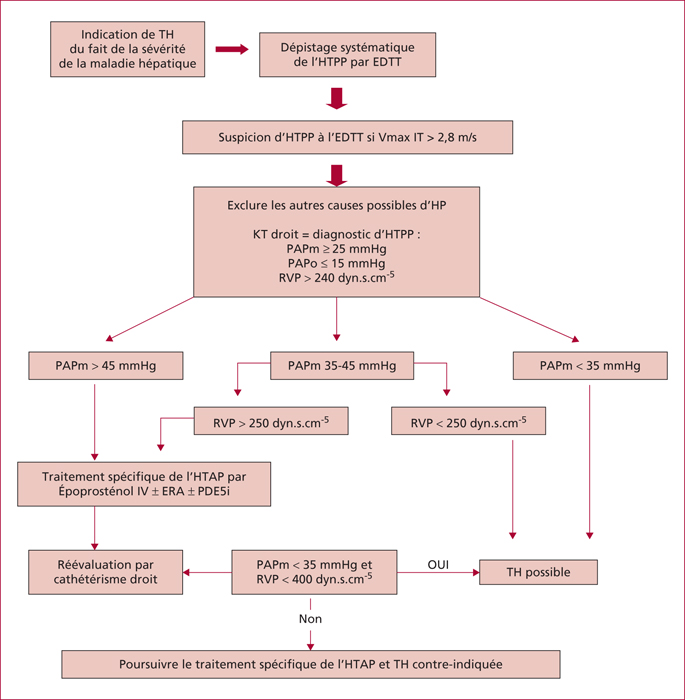
Portopulmonary hypertension (PoPH) is defined by the association of precapillary pulmonary arterial hypertension and portal hypertension with or without cirrhosis. Right heart catheterization (RHC) defined PoPH as a mean pulmonary artery pressure (mPAP) ≥ 25 mmHg at rest, a pulmonary vascular resistance (PVR) >240 dyn.s.cm-5 and a pulmonary capillary wedge pressure < 15 mmHg. Estimated prevalence of PoPH ranges between 2 % and 6 %. Pathogenesis of PoPH is unknown but is characterized by vasoconstrictive, proliferative and obliterative changes in the pulmonary vascular bed leading to a progressive obstruction of the pulmonary arterial blood flow. Dyspnea occurs often late in the course of PoPH. Doppler echocardiography screening is advised for all cirrhotic patients awaiting liver transplantion. The management of PoPH should involve the expertise of hepatologists, anesthesiologists and competence centers for pulmonary hypertension because therapeutic approaches have not been well validated. Although guidelines based on randomised trials are lacking, beta-blockers and anticoagulants are not recommended in PoPH. We currently have three classes of specific treatments of PoPH (prostacycline analogs, endothelin receptor antagonists and phosphodiesterase type-5 inhibitors) which have demonstrated significant improvements in cardiopulmonary hemodynamics measurements. These drugs act to cause vasodilatation and to target the vascular remodeling. PoPH is not considered an indication for liver transplantation but could be an option for selected patients improving their haemodynamic parameters under medical treatment without increasing cardiovascular risk.