Hépato-Gastro & Oncologie Digestive
MENUSacral neuromodulation for faecal incontinence: it's time for change… Volume 23, issue 9, Novembre 2016
Figures
Tables
Institut Léopold Bellan,
service de proctologie médico-chirurgicale,
185, rue Raymond Losserand,
75014 Paris, France
service de chirurgie digestive,
185, rue Raymond Losserand,
75014 Paris, France
service d’urologie,
185, rue Raymond Losserand,
75014 Paris, France
Assistance Publique-Hôpitaux de Marseille,
service de gastroentérologie,
Chemin de Bourrely,
13015 Marseille, France
unité d’explorations fonctionnelles digestives,
5 Place d’Arsonval,
69003 Lyon, France
- Key words: faecal incontinence, surgery, sacral neuromodulation
- DOI : 10.1684/hpg.2016.1362
- Page(s) : 861-8
- Published in: 2016
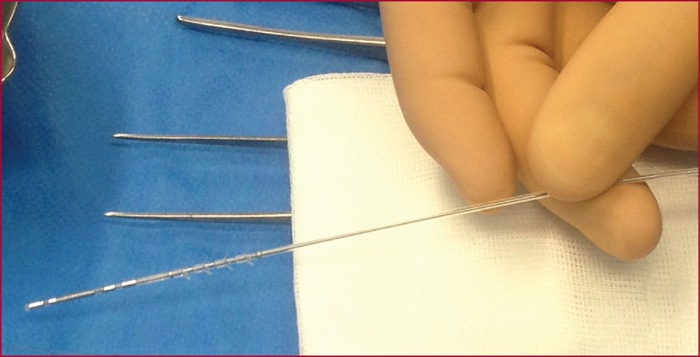
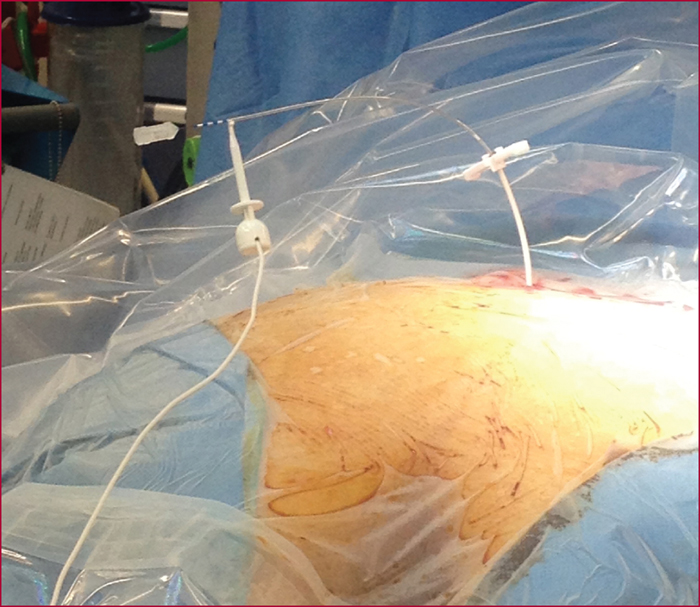
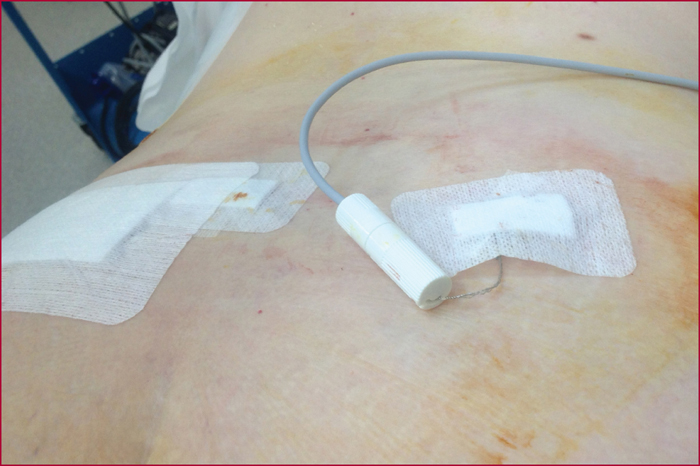
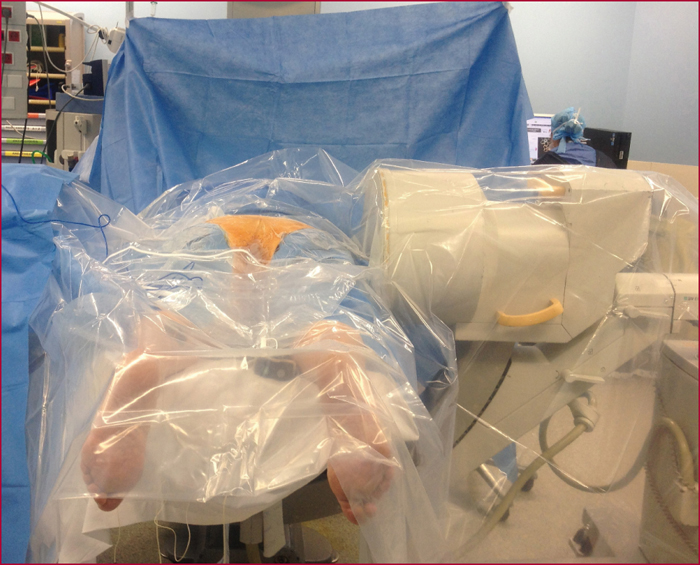
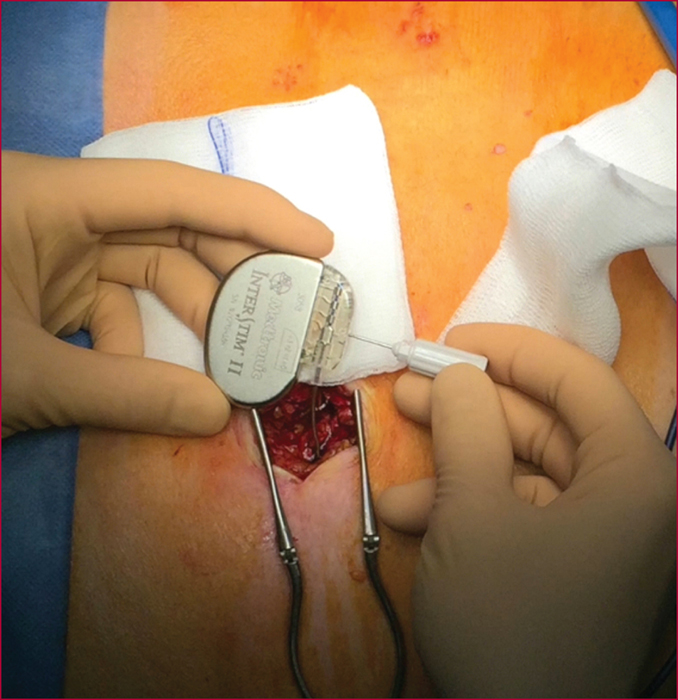
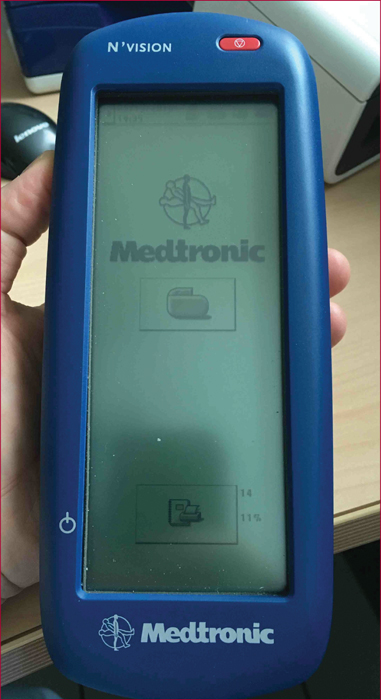
Sacral nerve stimulation (SNS) was initially developed for irritative and obstructive urinary disorders. Since 2009, its use to treat severe faecal incontinence after failure of first-line treatments has been fully reimbursed by the French healthcare system. The technique is based on electrical stimulation of the sacral nerve roots of the pelvi-perineal area by a percutaneously implanted electrode in the sacral foramen (S3 root) that is linked to a separate subcutaneously implanted pulse generator. Eligibility of patients for SNS must be decided in the setting of a multidisciplinary team after first undertaking a full assessment that includes a record of bowel movements, a score for the level of incontinence, endoanal ultrasound, anorectal manometry, uro-dynamic testing in case of associated urinary problems, and/or dynamic pelvic imaging for suspected pelvic floor disorders. The outcomes with this new technique have remained stable since the initial publications, and it is estimated that 50% of the patients who were eligible from the outset received this treatment. The mechanism of action is still poorly understood, and despite a large number of published studies, no significant predictive factors for long-term outcomes have been identified. Its effect is not limited to stimulation of an anatomically intact but functionally defective sphincter, as it also acts on colonic motility, on the sensorimotor response to rectal distension, and on cortical processing of anorectal sensation. These different modes of action explain the recent inclusion of faecal incontinence with a sphincter defect and the effects of rectal or rectosigmoid resection as indications for SNS treatment. Post-implantation monitoring is an essential aspect that involves very specific skills. It consists of checking the circuit connections, and -if need be- making very empirically-based adjustments to the generator settings, as well as probing for any complications.