Hépato-Gastro & Oncologie Digestive
MENUIntraductal papillary neoplasm of the bile duct: A biliary equivalent to intraductal papillary mucinous neoplasm of the pancreas? Volume 21, issue 6, Juin 2014
pôle des maladies de l’appareil digestif,
service de gastroentérologie et pancréatologie,
100, boulevard du général Leclerc
92118 Clichy Cedex, France ;
Université Paris-Diderot-Paris 7,
DHU Unity,
France
- Key words: IPN-B, cholangiocarcinoma, hepatic résections, IPMN
- DOI : 10.1684/hpg.2014.1030
- Page(s) : 460-6
- Published in: 2014
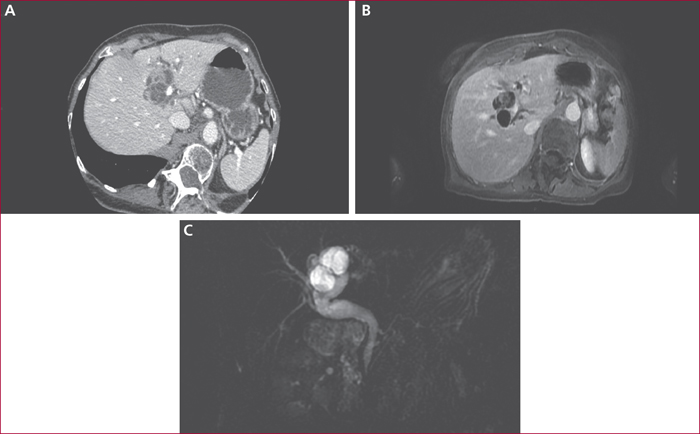
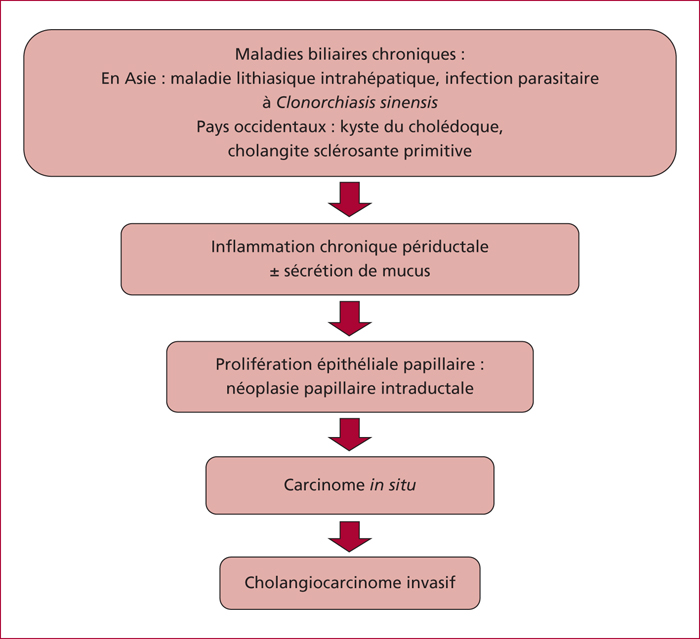
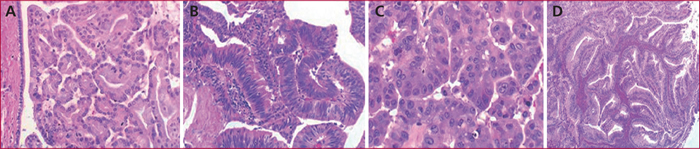
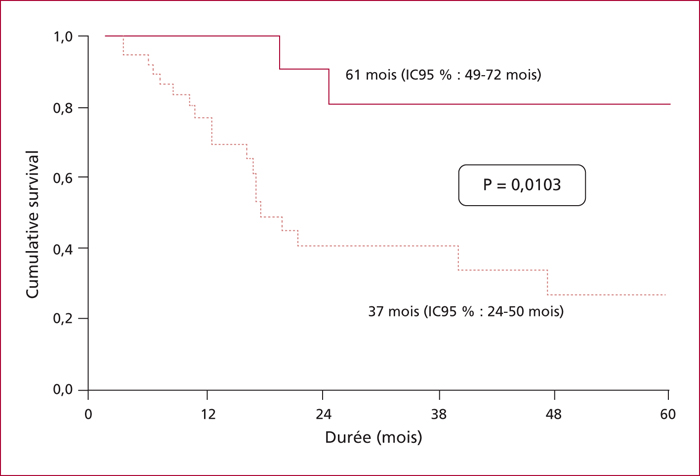
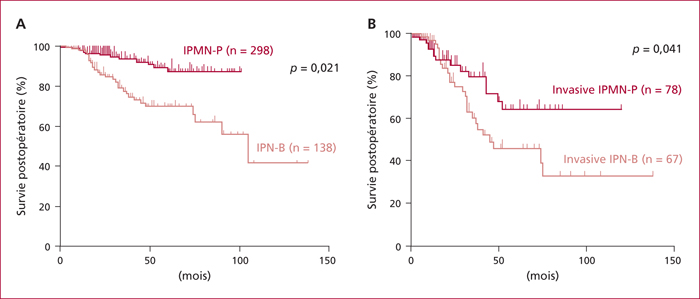
Intraductal papillary biliary neoplasm of the bile duct (IPN-B) is a rare intraductal tumor characterized by a papillary proliferation of the biliary epithelium responsible of a variable mucin hypersecretion, causing a dilatation of the bile ducts. IPN-B is the biliary equivalent to intraductal papillary mucinous neoplasm of the pancreas (IPMN). Like IPMN, there are 4 histological types with different prognosis. Magnetic resonance cholangiopancreatography (MRCP) and abdominal ultrasonography are the key procedure for diagnosis showing cystic lesion of the biliary tree associated with down-stream ductal dilatation. The distribution of histological types is different with a predominance of gastric subtypes in IPMN and pancreatobiliary subtypes in IPN-B explaining a better prognosis of IPMN. Carcinogenesis of IPN -B is characterised by an evolution from adenoma to adenocarcinoma. Seventy four per cent of IPN-B are diagnosed at the stage of in situ carcinoma or cholangiocarcinoma. Without contraindication, surgery is the best treatment because of the high risk of malignancy. The 5-year postoperative survival rate is 44 % for the invasive carcinoma.