Hépato-Gastro & Oncologie Digestive
MENUHow to manage chronic calcifying pancreatitis? Volume 30, issue 2, February 2023
- Key words: chronic pancreatitis, exocrine pancreatic insufficiency, diabetes, chronic pain, pancreatic ductal adenocarcinoma
- DOI : 10.1684/hpg.2023.2533
- Page(s) : 166-74
- Published in: 2023
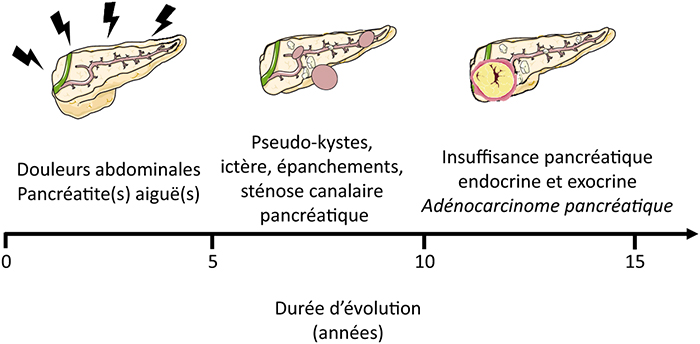
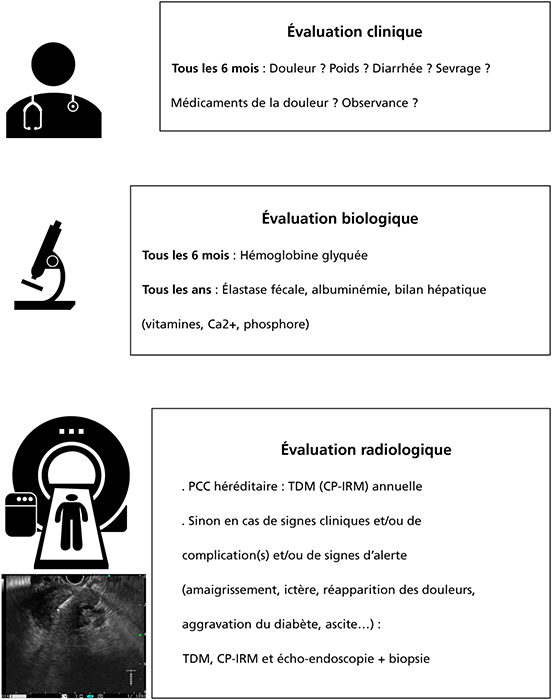
Chronic calcifying pancreatitis is a chronic inflammatory disease of the pancreas which leads to the development of parenchymal and ductal fibrosis. The main cause is chronic alcoholism. From its lesions arise symptoms, acute and chronic complications which will tag the evolution of this disease which takes place over 15 to 20 years. In addition to the clinical and paraclinical check-ups necessary for acute complications, the GI specialist must ensure the long-term follow-up. It will rely on several practitioners from different specialties reflecting the multidisciplinary nature of this disease. At the clinical level, a six-monthly consultation will address the problem of chronic pain (type, evolution, treatment, opiate medications, dependence), nutritional status, alcohol and tobacco consumption, signs of pancreatic exocrine insufficiency (weight, diarrhea) and diabetes, as well as complications related to chronic alcohol and tobacco consumptions. Biologically, exocrine insufficiency is detected by measuring fecal elastase (annually), and diabetes by measuring glycated hemoglobin every six months. It is also necessary to monitor the serum albumin level, the hydroelectrolytic, renal and hepatic parameters and the vitamin D level. Imaging (cholangiopancreatography MRI and/or CT scan) is necessary in case of complications or new symptoms and systematically over the long term to detect the occurrence of pancreatic adenocarcinoma, particularly in cases of hereditary chronic pancreatitis (imaging every year or two depending on the cause of the pancreatitis). If there is any doubt, an endoscopic ultrasound with biopsy will complete this assessment. It will therefore be necessary to adapt the treatment with analgesics, pancreatic extracts, oral antidiabetics or insulin, or even to discuss in certain cases a therapeutic endoscopy in an expert center. The multidisciplinary approach will involve the general practitioner, diabetologist, psychiatrist, addictologist, algologist, biliary and pancreatic endoscopist and sometimes even the pancreas surgeon.